Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine III
75 - Utility of Procalcitonin to Evaluate Bacterial Infection in Febrile Infants Ages 8-60 Days
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 75
Publication Number: 75.105
Publication Number: 75.105
Quinney Fu, Phoenix Children's Hospital, Phoenix, AZ, United States; Jared Kusma, Phoenix Children's Hospital, Phoenix, AZ, United States; Sandra Gage, University of Arizona College of Medicine - Phoenix, Phoenix, AZ, United States; Richard Engel, Phoenix Children's Hospital, Scottsdale, AZ, United States; Vedant Gupta, Phoenix Children's Hospital, Phoenix, AZ, United States; Bo Borch-Christensen, Phoenix Children's Hospital, Phoenix, AZ, United States; Hannah Riggins, Phoenix Children's Hospital, Phoenix, AZ, United States; Lucia Mirea, Phoenix Children's Hospital, Phoenix, AZ, United States; Daniel L. Stone, Phoenix Children's Hospital, Mesa, AZ, United States; Jamie Librizzi, Phoenix Children's Hospital, Phoenix, AZ, United States
Quinney Fu, MD
Pediatric Emergency Medicine Fellow
Phoenix Children's
Phoenix, Arizona, United States
Presenting Author(s)
Background: Procalcitonin (PCT) is a known predictive tool for invasive bacterial infections (IBI), including bacteremia, urinary tract infections (UTI) and, meningitis. While PCT is routinely recommended as part of the initial work-up to help risk stratify febrile infants, few studies have examined PCT levels in young infants ages 8 to 60 days presenting with fever.
Objective: 1) Compare mean PCT levels in infants presenting with fever with an IBI versus those without bacterial infection; 2) Assess the ability of PCT to predict IBI in febrile infants ages 8-21, 22-28, and 29-60-days.
Design/Methods: This retrospective cohort study examined infants ages 8-60 days presenting with fever to the emergency department of a tertiary children’s hospital from 2018-2020. Exclusion criteria: prematurity ( < 37 weeks), previous intensive care stay, previous hospitalization for infectious etiology, current or prior antibiotic use, immunosuppression, and chronic comorbid conditions. Patients were identified via ICD-10 codes for fever, bacteremia, UTI, pyelonephritis, and meningitis; data was extracted via manual chart review of the electronic medical record. Data collected included demographics, PCT, bacterial culture results, and viral testing results. Mean PCT levels were compared between patients with and without IBI using the Wilcoxon rank sum test. Logistic regression models were fit to estimate the receiver operative characteristic (ROC) curve and the corresponding area under the curve (AUC). Sensitivity and specificity were estimated using a PCT threshold value set at the Youden index.
Results: A total of 894 patients were included: 17% 8-21 days old, 11% 22-28 days old, and 72% 29-60 days old. 204 patients (22.9%) were diagnosed with an IBI. Mean PCT levels for infants with IBI were 3.1 ng/mL compared to 0.3 ng/mL for infants without IBI (p-value < 0.001). Similar associations between PCT levels and IBIs were detected within each age group. Overall, PCT predictive ability was AUC=0.85, with 69% sensitivity and 90% specificity based on a PCT level 0.24ng/mL cutoff value. The youngest infants, ages 8-21 days, had the highest AUC=0.91, with 80% sensitivity and 92% specificity based on PCT level 0.47 ng/mL cutoff (Table and Figure).Conclusion(s): PCT remains a strong predictor of IBI in infants ages 8-60 days with fever especially among those ages 8-21 days. Further study is warranted to specifically examine PCT in relation to bacteremia, UTI, and meningitis.
Table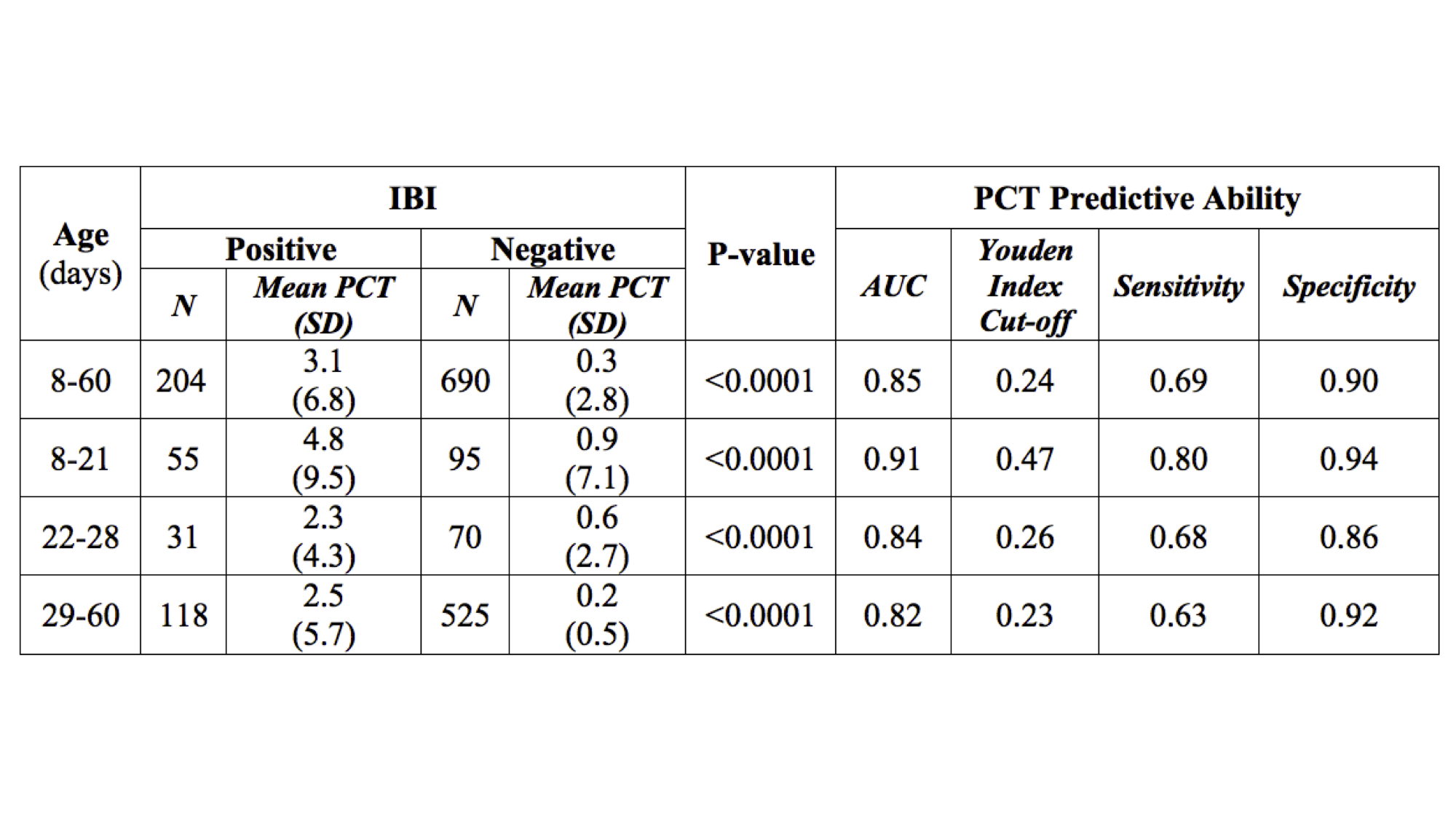 PCT and IBI in febrile infants ages 8-60 days. PCT= Procalcitonin; IBI= Invasive bacterial infection; SD= Standard deviation; AUC= Area under the curve.
PCT and IBI in febrile infants ages 8-60 days. PCT= Procalcitonin; IBI= Invasive bacterial infection; SD= Standard deviation; AUC= Area under the curve.
Figure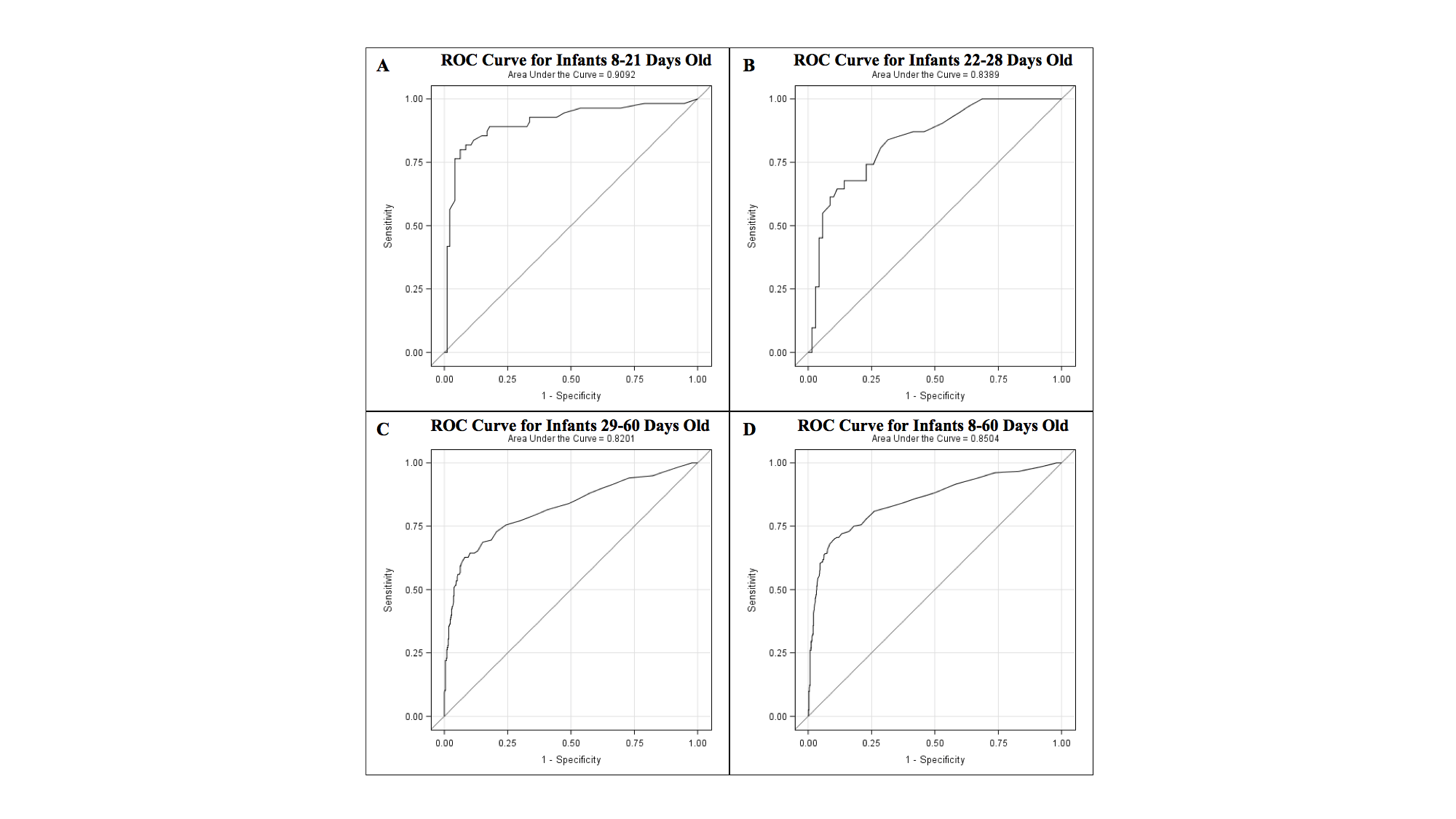 The ROC curves of PCT for febrile infants A. 8-21 days old, B. 22-28 days old, C. 29-60 days old, and D. 8-60 days old for the diagnosis of IBI. ROC= Receiver operating characteristics; PCT= Procalcitonin; IBI= Invasive bacterial infection.
The ROC curves of PCT for febrile infants A. 8-21 days old, B. 22-28 days old, C. 29-60 days old, and D. 8-60 days old for the diagnosis of IBI. ROC= Receiver operating characteristics; PCT= Procalcitonin; IBI= Invasive bacterial infection.
Objective: 1) Compare mean PCT levels in infants presenting with fever with an IBI versus those without bacterial infection; 2) Assess the ability of PCT to predict IBI in febrile infants ages 8-21, 22-28, and 29-60-days.
Design/Methods: This retrospective cohort study examined infants ages 8-60 days presenting with fever to the emergency department of a tertiary children’s hospital from 2018-2020. Exclusion criteria: prematurity ( < 37 weeks), previous intensive care stay, previous hospitalization for infectious etiology, current or prior antibiotic use, immunosuppression, and chronic comorbid conditions. Patients were identified via ICD-10 codes for fever, bacteremia, UTI, pyelonephritis, and meningitis; data was extracted via manual chart review of the electronic medical record. Data collected included demographics, PCT, bacterial culture results, and viral testing results. Mean PCT levels were compared between patients with and without IBI using the Wilcoxon rank sum test. Logistic regression models were fit to estimate the receiver operative characteristic (ROC) curve and the corresponding area under the curve (AUC). Sensitivity and specificity were estimated using a PCT threshold value set at the Youden index.
Results: A total of 894 patients were included: 17% 8-21 days old, 11% 22-28 days old, and 72% 29-60 days old. 204 patients (22.9%) were diagnosed with an IBI. Mean PCT levels for infants with IBI were 3.1 ng/mL compared to 0.3 ng/mL for infants without IBI (p-value < 0.001). Similar associations between PCT levels and IBIs were detected within each age group. Overall, PCT predictive ability was AUC=0.85, with 69% sensitivity and 90% specificity based on a PCT level 0.24ng/mL cutoff value. The youngest infants, ages 8-21 days, had the highest AUC=0.91, with 80% sensitivity and 92% specificity based on PCT level 0.47 ng/mL cutoff (Table and Figure).Conclusion(s): PCT remains a strong predictor of IBI in infants ages 8-60 days with fever especially among those ages 8-21 days. Further study is warranted to specifically examine PCT in relation to bacteremia, UTI, and meningitis.
Table
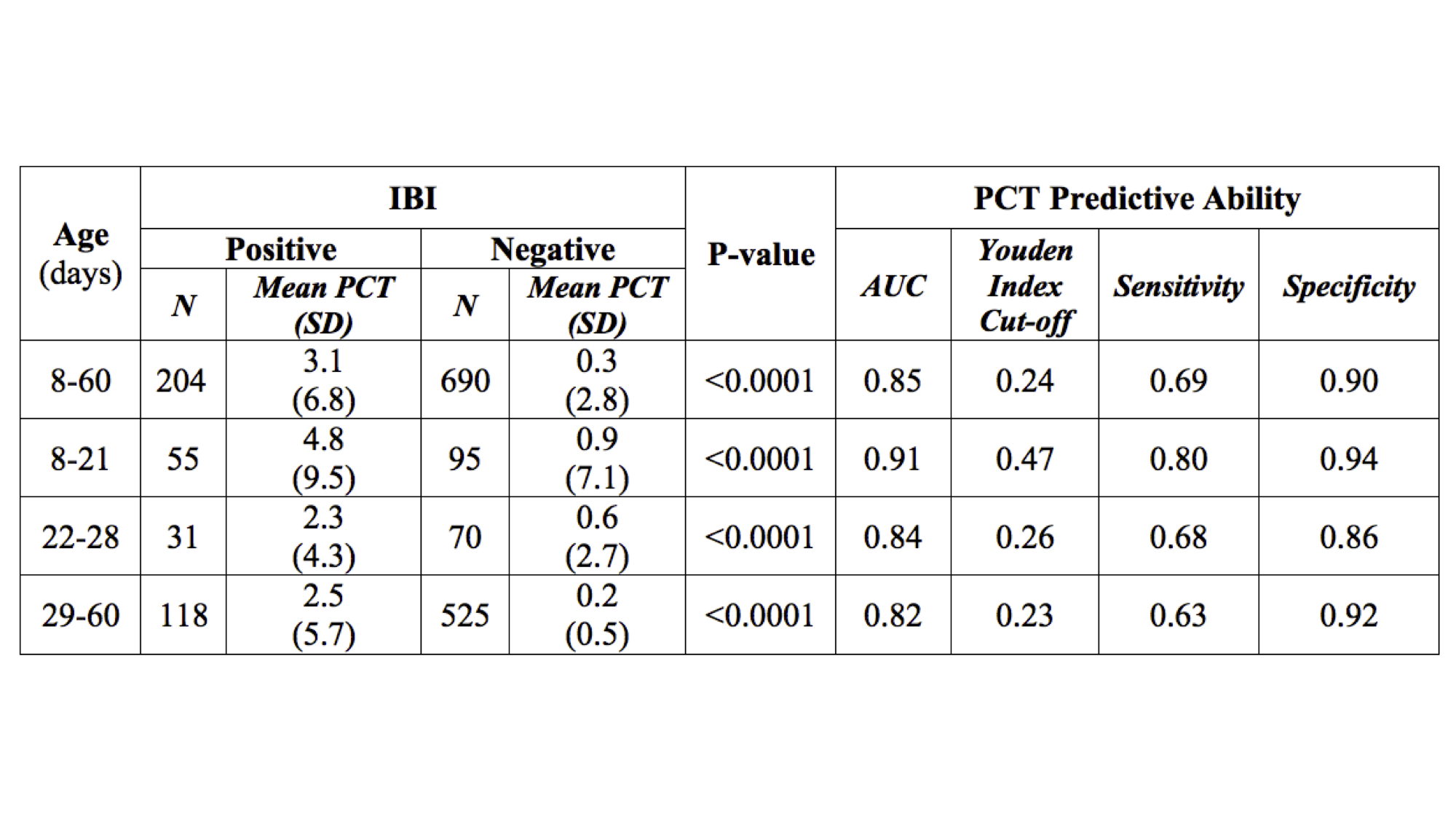 PCT and IBI in febrile infants ages 8-60 days. PCT= Procalcitonin; IBI= Invasive bacterial infection; SD= Standard deviation; AUC= Area under the curve.
PCT and IBI in febrile infants ages 8-60 days. PCT= Procalcitonin; IBI= Invasive bacterial infection; SD= Standard deviation; AUC= Area under the curve.Figure
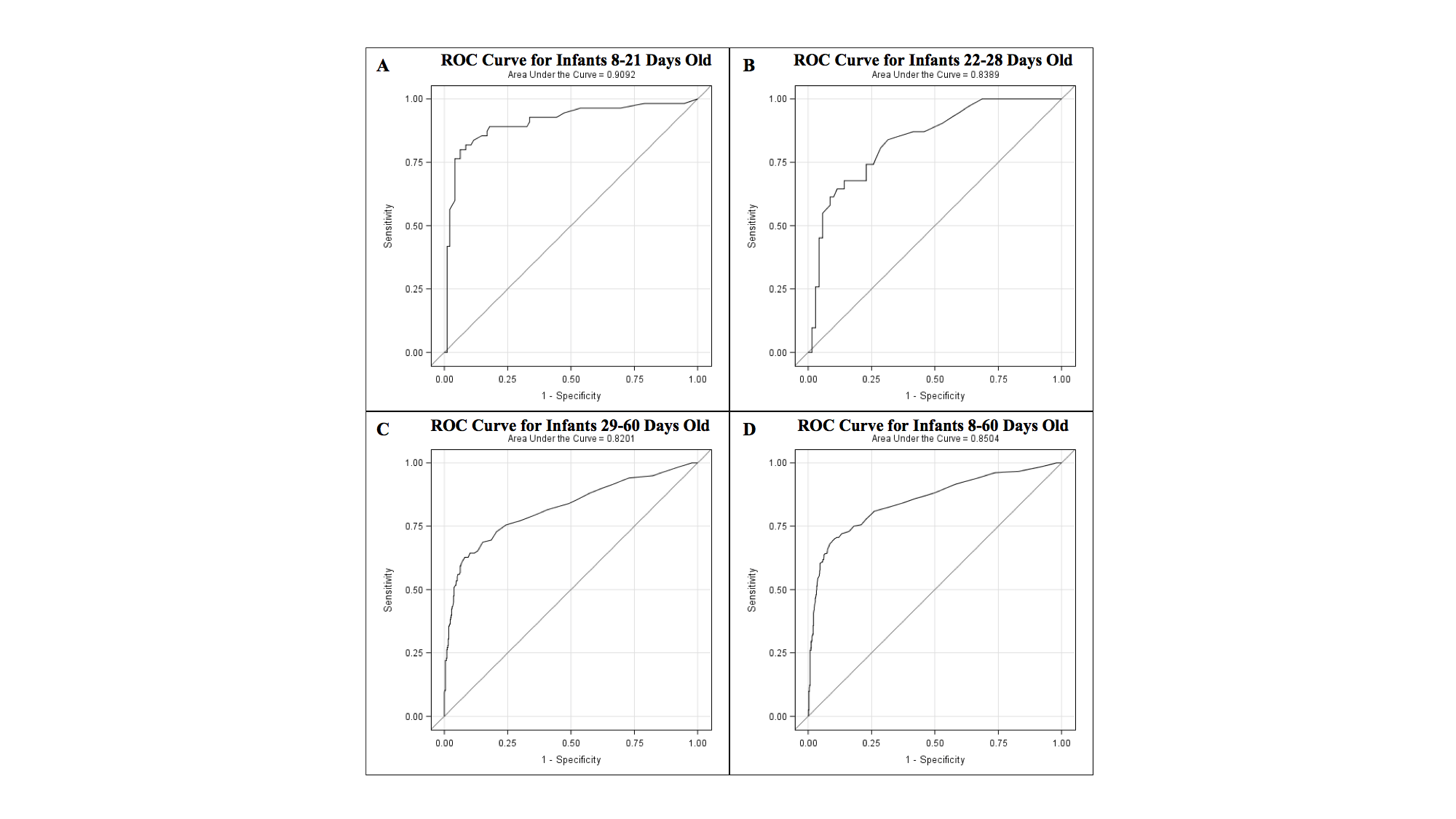 The ROC curves of PCT for febrile infants A. 8-21 days old, B. 22-28 days old, C. 29-60 days old, and D. 8-60 days old for the diagnosis of IBI. ROC= Receiver operating characteristics; PCT= Procalcitonin; IBI= Invasive bacterial infection.
The ROC curves of PCT for febrile infants A. 8-21 days old, B. 22-28 days old, C. 29-60 days old, and D. 8-60 days old for the diagnosis of IBI. ROC= Receiver operating characteristics; PCT= Procalcitonin; IBI= Invasive bacterial infection.