Hematology/Oncology
Category: Abstract Submission
Hematology/Oncology I
333 - Vulvar and Oral Langerhans Cell Histiocytosis: A Pediatric Case Report
Friday, April 22, 2022
6:15 PM - 8:45 PM US MT
Poster Number: 333
Publication Number: 333.113
Publication Number: 333.113
Jennifer Nestor, The Children's Regional Hospital at Cooper, Philadelphia, PA, United States; Saifuddin T. Mama, Cooper University Health Care, NJ, NJ, United States; Rafat Ahmed, Cooper Medical School of Rowan University, Camden, NJ, United States; Donna Perruzza, Cooper Medical School of Rowan University, Cherry Hill, NJ, United States

Jennifer Nestor, MD
Resident Physician
The Children's Regional Hospital at Cooper
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Langerhans cell histiocytosis (LCH) is an uncommon hematologic condition resulting from neoplastic proliferation of antigen-presenting cells with characteristics of Langerhans cells. Cells can accumulate in many organs including skin, bone, liver, brain and lung. Bone lesions are reported in 80% of cases of LCH. A diagnosis is made via histopathological analysis. LCH may present with single-system or multi-system lesions and may be unifocal or multifocal. It is more common in children than adults. About 5 in 1 million children are diagnosed annually at a mean age of 1.8. Treatment is variable based on system involvement and spans from observation of skin lesions to chemotherapeutic regimens for multisystem disease.
Objective: Discuss a case of pediatric LCH presenting initially as a vulvar lesion
Design/Methods: Single subject case study
Results: A 10 year old Hispanic female presented with several months of swollen labia, scant yellow vaginal discharge and pustular vulvar lesions. She had a remote history of straddle injury to the area with unhealed left periclitoral laceration requiring operative repair. Abnormal vulvar tissue was biopsied intraoperatively by pediatric gynecology. Intraoperative biopsy and immunohistochemical staining revealed CD43, CD1a and S100 positive cells consistent with LCH. Eight months after initial presentation the patient reported lesions on the left hard palate confirmed to be LCH with biopsy. After initiation of steroid cream on vulvar lesions, multifocal mucosal involvement (oral and vulvar lesions) warranted treatment with a 6 month course of methotrexate (MTX) with minimal responsiveness. Adjunct therapy for treatment multifocal disease was not started at the initial institution as the patient was lost to follow-up. Oncologic management was reinstated at a tertiary care center where 6-mercaptopurine treatment was initiated without improvement. Intralesional steroid injections were trialed on hard palate lesions resulting in decrease in size of lesions. The patient returned to gynecologic care for intralesional labial steroid injection with response to treatment.Conclusion(s): LCH commonly presents as disordered growth of dendritic cells in bone or skin, though few reported incidences of vulvar LCH in pediatric cases have been published. LCH should remain on the differential when evaluating pediatric and adolescent patients with vulvar lesions. Biopsy should be utilized when a diagnosis of LCH is considered for confirmation so that treatment pathways can be initiated. Consider limiting chemotherapeutic treatment in patients with focal disease.
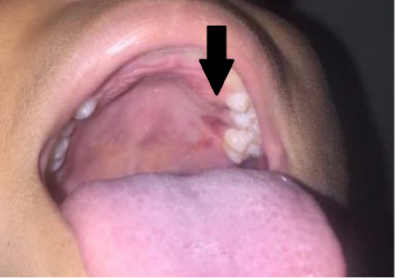
LCH Lesions of Hard Palate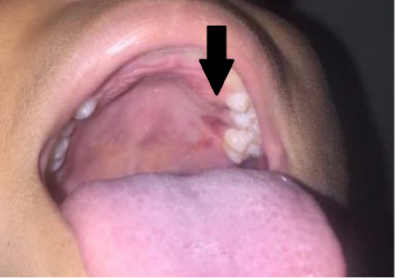
LCH Lesions of Vulva
Objective: Discuss a case of pediatric LCH presenting initially as a vulvar lesion
Design/Methods: Single subject case study
Results: A 10 year old Hispanic female presented with several months of swollen labia, scant yellow vaginal discharge and pustular vulvar lesions. She had a remote history of straddle injury to the area with unhealed left periclitoral laceration requiring operative repair. Abnormal vulvar tissue was biopsied intraoperatively by pediatric gynecology. Intraoperative biopsy and immunohistochemical staining revealed CD43, CD1a and S100 positive cells consistent with LCH. Eight months after initial presentation the patient reported lesions on the left hard palate confirmed to be LCH with biopsy. After initiation of steroid cream on vulvar lesions, multifocal mucosal involvement (oral and vulvar lesions) warranted treatment with a 6 month course of methotrexate (MTX) with minimal responsiveness. Adjunct therapy for treatment multifocal disease was not started at the initial institution as the patient was lost to follow-up. Oncologic management was reinstated at a tertiary care center where 6-mercaptopurine treatment was initiated without improvement. Intralesional steroid injections were trialed on hard palate lesions resulting in decrease in size of lesions. The patient returned to gynecologic care for intralesional labial steroid injection with response to treatment.Conclusion(s): LCH commonly presents as disordered growth of dendritic cells in bone or skin, though few reported incidences of vulvar LCH in pediatric cases have been published. LCH should remain on the differential when evaluating pediatric and adolescent patients with vulvar lesions. Biopsy should be utilized when a diagnosis of LCH is considered for confirmation so that treatment pathways can be initiated. Consider limiting chemotherapeutic treatment in patients with focal disease.
LCH Lesions of Hard Palate
LCH Lesions of Vulva

