Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VI
350 - Cardiac Pathology Identified by POCUS in Patients With Presumed Sepsis in a Pediatric ED
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 350
Publication Number: 350.205
Publication Number: 350.205
Jacob Hemberger, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Ethan S. Vorel, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Rachel Rempell, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Brandon Ku, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Fran Balamuth, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States

Jacob Hemberger, MD
Pediatric Emergency Medicine Fellow
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background:
Cardiac point-of-care ultrasound (C-POCUS) is an emerging diagnostic tool in pediatric sepsis and is recommended by the recent Surviving Sepsis Guidelines to guide vasoactive medication choice in children with fluid refractory shock. Prior studies in pediatric ICUs have shown clinical assessment alone unreliably predicts sepsis-related myocardial dysfunction, with rates of dysfunction as high as 37% in children with fluid refractory shock. Prevalence of sepsis-related hemodynamic abnormalities in the pediatric ED is currently poorly described.
Objective:
To describe C-POCUS exams for ED patients treated for suspected sepsis, including prevalence of abnormal findings, image quality, and factors associated with cardiac dysfunction.
Design/Methods:
Retrospective observational study from Nov-2020 to Aug-2021 for ED patients with a C-POCUS exam completed during treatment for suspected sepsis, defined as use of a pediatric ED sepsis order set. We abstracted sonographer documentation of C-POCUS findings and ultrasound image quality from the medical record. We explored treatment factors associated with cardiac dysfunction.
Results:
Clinicians completed C-POCUS exams for 65/174 (37%) of patients treated for suspected sepsis. Pathology in C-POCUS exams included reduced LV systolic function (11%), trace or small pericardial effusion (22%), and flattened IVC (14%) (Table 1). Ultrasound image adequacy was highest for parasternal long axis (91%) and parasternal short axis (83%) views (Table 2). Images could not be interpreted in 5% of exams. The small proportion of patients with cardiac dysfunction limited identification of associated clinical factors beyond simple description (Table 3). Of patients with dysfunction, 5/7 were started on a vasoactive agent, 4/7 were diagnosed with MIS-C, and all received at least two fluid boluses.
Conclusion(s):
Emergency C-POCUS providers can obtain adequate cardiac images and identify pericardial effusion, flattened IVC suggesting hypovolemia, and cardiac dysfunction during resuscitation for presumed sepsis in a large pediatric ED. Highest rates of adequate ultrasound images were obtained for parasternal views. In an exploratory analysis, most patients with cardiac dysfunction identified by C-POCUS ultimately received vasopressors or at least two fluid boluses, which may be a proxy for degree of illness and will be explored in future analysis. Larger studies are needed to further characterize hemodynamic abnormalities on C-POCUS in pediatric emergency medicine, especially for fluid-refractory septic shock.
Table 1: Prevalence of Pathology Identified by Cardiac POCUS Exams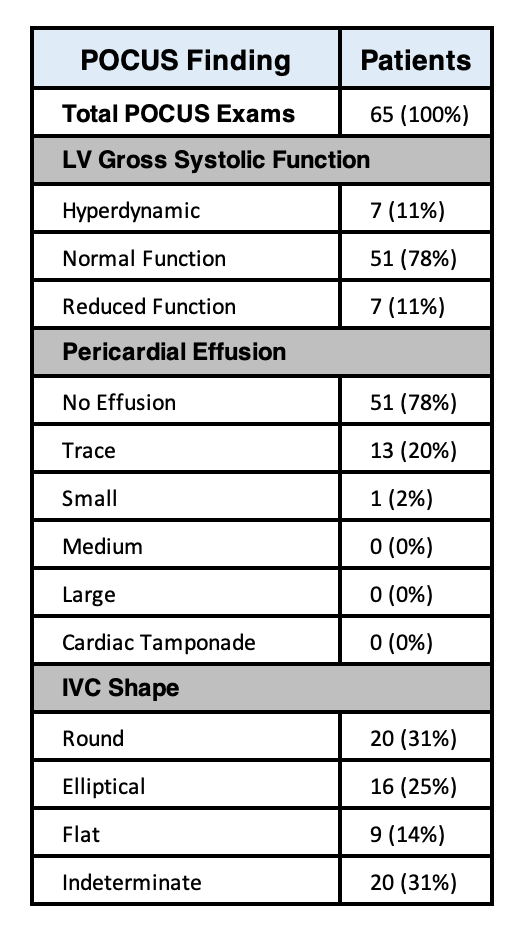 Findings in 65 cardiac POCUS exams. LV = left ventricle. IVC = inferior vena cava.
Findings in 65 cardiac POCUS exams. LV = left ventricle. IVC = inferior vena cava.
Table 2: Quality of Cardiac POCUS Images.png) Image quality for the standard C-POCUS views, including PSLA (parasternal long axis), PSSA (parasternal short axis), A4CH (apical four chamber), subxiphoid, and IVC (inferior vena cava) in either sagittal or transverse axis.
Image quality for the standard C-POCUS views, including PSLA (parasternal long axis), PSSA (parasternal short axis), A4CH (apical four chamber), subxiphoid, and IVC (inferior vena cava) in either sagittal or transverse axis.
Cardiac point-of-care ultrasound (C-POCUS) is an emerging diagnostic tool in pediatric sepsis and is recommended by the recent Surviving Sepsis Guidelines to guide vasoactive medication choice in children with fluid refractory shock. Prior studies in pediatric ICUs have shown clinical assessment alone unreliably predicts sepsis-related myocardial dysfunction, with rates of dysfunction as high as 37% in children with fluid refractory shock. Prevalence of sepsis-related hemodynamic abnormalities in the pediatric ED is currently poorly described.
Objective:
To describe C-POCUS exams for ED patients treated for suspected sepsis, including prevalence of abnormal findings, image quality, and factors associated with cardiac dysfunction.
Design/Methods:
Retrospective observational study from Nov-2020 to Aug-2021 for ED patients with a C-POCUS exam completed during treatment for suspected sepsis, defined as use of a pediatric ED sepsis order set. We abstracted sonographer documentation of C-POCUS findings and ultrasound image quality from the medical record. We explored treatment factors associated with cardiac dysfunction.
Results:
Clinicians completed C-POCUS exams for 65/174 (37%) of patients treated for suspected sepsis. Pathology in C-POCUS exams included reduced LV systolic function (11%), trace or small pericardial effusion (22%), and flattened IVC (14%) (Table 1). Ultrasound image adequacy was highest for parasternal long axis (91%) and parasternal short axis (83%) views (Table 2). Images could not be interpreted in 5% of exams. The small proportion of patients with cardiac dysfunction limited identification of associated clinical factors beyond simple description (Table 3). Of patients with dysfunction, 5/7 were started on a vasoactive agent, 4/7 were diagnosed with MIS-C, and all received at least two fluid boluses.
Conclusion(s):
Emergency C-POCUS providers can obtain adequate cardiac images and identify pericardial effusion, flattened IVC suggesting hypovolemia, and cardiac dysfunction during resuscitation for presumed sepsis in a large pediatric ED. Highest rates of adequate ultrasound images were obtained for parasternal views. In an exploratory analysis, most patients with cardiac dysfunction identified by C-POCUS ultimately received vasopressors or at least two fluid boluses, which may be a proxy for degree of illness and will be explored in future analysis. Larger studies are needed to further characterize hemodynamic abnormalities on C-POCUS in pediatric emergency medicine, especially for fluid-refractory septic shock.
Table 1: Prevalence of Pathology Identified by Cardiac POCUS Exams
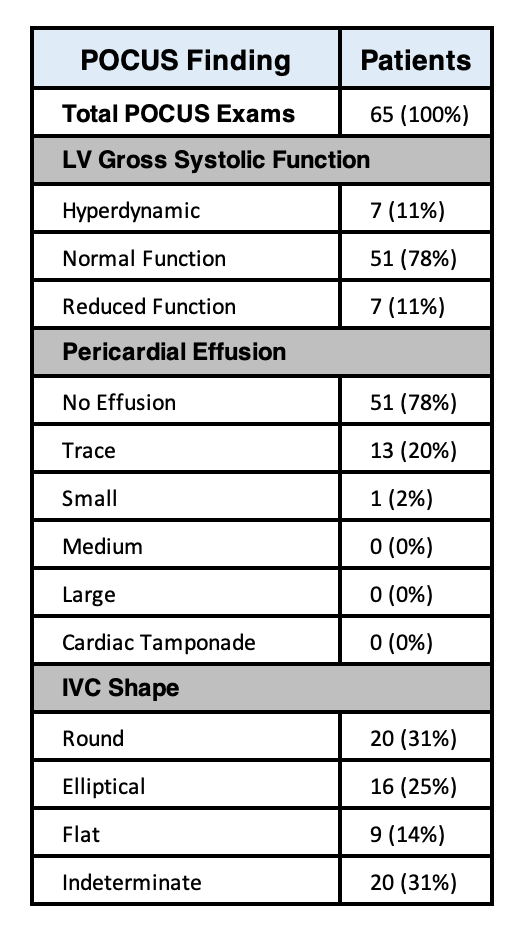 Findings in 65 cardiac POCUS exams. LV = left ventricle. IVC = inferior vena cava.
Findings in 65 cardiac POCUS exams. LV = left ventricle. IVC = inferior vena cava.Table 2: Quality of Cardiac POCUS Images
.png) Image quality for the standard C-POCUS views, including PSLA (parasternal long axis), PSSA (parasternal short axis), A4CH (apical four chamber), subxiphoid, and IVC (inferior vena cava) in either sagittal or transverse axis.
Image quality for the standard C-POCUS views, including PSLA (parasternal long axis), PSSA (parasternal short axis), A4CH (apical four chamber), subxiphoid, and IVC (inferior vena cava) in either sagittal or transverse axis.