Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up III
263 - Cerebral Palsy and Persistent Motor Impairment in Extremely Low Gestational Age Newborns: Associating Risk Factors with Diagnoses at Age 2 and 10 Years
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 263
Publication Number: 263.225
Publication Number: 263.225
Timothy P. Marinelli, Tufts Childrens Hospital, Longmeadow, MA, United States; Joe X. Yi, University of North Carolina at Chapel Hill School of Medicine, Cary, NC, United States; Michael O’Shea, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Robert Joseph, Boston University, Boston, MA, United States; Stephen R. Hooper, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States; Karl Kuban, Boston University School of Medicine, Plymouth, MA, United States; Christina Sakai, Tufts Childrens Hospital, Boston, MA, United States; Michael E. Msal, Comer Children's Hospital at University of Chicago Medical Center, Chicago, IL, United States; Rebecca Fry, UNC-Chapel Hill, Chapel Hill, NC, United States; Rachana Singh, Tufts Childrens Hospital, Boston, MA, United States

Timothy P. Marinelli, DO
Neonatal-Perinatal Medicine Fellow
Tufts Childrens Hospital
Boston, Massachusetts, United States
Presenting Author(s)
Background: Cerebral palsy (CP) and motor impairment (MI) remain the most prevalent neuro-motor disabilities of childhood, with up to 50% of affected individuals born extremely preterm (EP). Despite the well-described relationship between preterm birth and CP/MI, there remains an unstudied interplay of additional risk factors and comorbidities that complicate the clinical prediction of CP/MI in infants born EP.
Objective: To identify perinatal factors in infants born EP that are associated with diagnosis of CP/MI at 2 and 10 years of age to inform the design of a predictive algorithm to estimate the risk, at NICU discharge, of receiving a diagnosis of CP/MI during childhood.
Design/Methods: Participants were enrolled at birth in the Extremely Low Gestational Age Newborn (ELGAN) Study between 2002 and 2004. Based on a standard neurological examination at 2 and the Gross Motor Function Classification System at 10 years of age, 849 participants (71% of survivors) were classified as follows: No CP/MI, CP only at 2 years, MI only at 10 years and CP/MI at both 2 and 10 years. To describe associations, between risk factors and CP/M, odds ratios (OR) and 95% confidence intervals (CI) were estimated using logistic regression, with no CP/MI at age 2 and age 10 as the referent group.
Results: Overall, 849 study participants underwent evaluation for CP/MI at 2 and 10 years of age. Of these, 64 (7.5%) had a diagnosis of CP/MI at both 2 and 10 years, while an additional 63 (7.4%) participants had a diagnosis of CP/MI at one visit but not the other (Table 1). Of 22 total risk factors queried, the strongest association with diagnosis of CP/MI at 2 and 10 years of age was seen with ventriculomegaly (OR 22.2, CI 12.0-41.2), periventricular leukomalacia (PVL), (OR 14.1, CI 7.7 - 25.8) and echogenicity on head ultrasound (OR 8.1, CI 4.5 – 14.5.) (Table 2).Conclusion(s): In the ELGAN cohort, the diagnosis of CP at 2 years did not always predict a diagnosis of MI at 10 years. We identified multiple clinical risk factors predictive of CP/MI, that are currently being used to compare individuals with a persistent diagnoses of CP/MI and those whose MI resolved, as well as to construct a predictive algorithm to estimate the risk.
Table 1. Baseline prenatal, perinatal and postnatal factors for CP/MI diagnosis at 2 and/or 10 years of age.png) CP: Cerebral Palsy, MI: Motor Impairment, SIP: Spontaneous intestinal Perforation, HUS: Head Ultrasound, SNAP: Score for Neonatal Acute Physiology
CP: Cerebral Palsy, MI: Motor Impairment, SIP: Spontaneous intestinal Perforation, HUS: Head Ultrasound, SNAP: Score for Neonatal Acute Physiology
*(weight z-score at discharge – weight z-score at birth)
# (weight z-score at discharge – weight z-score at DOL 28)
Table 2. Associated odds ratio for diagnosis of CP/MI by subgroups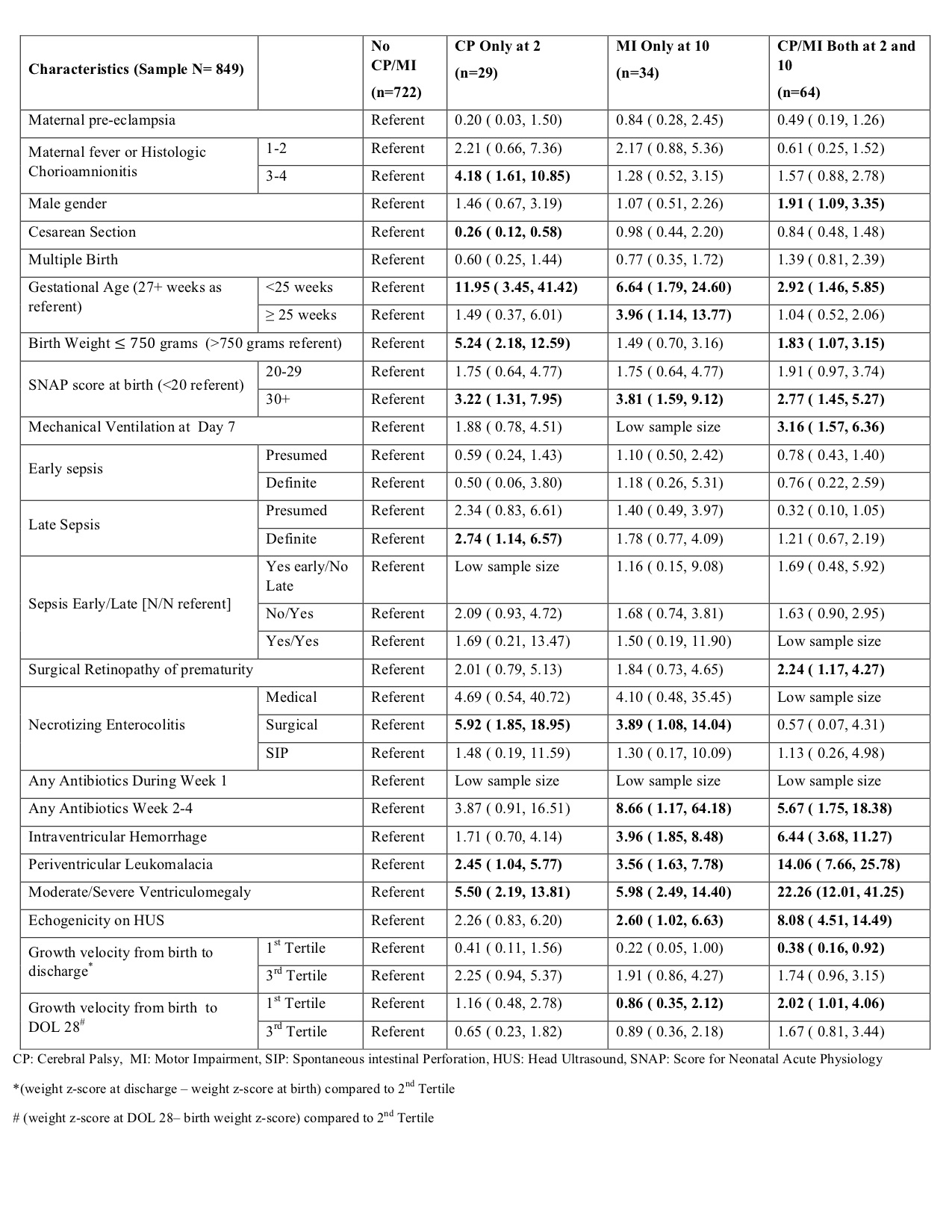 CP: Cerebral Palsy, MI: Motor Impairment, SIP: Spontaneous intestinal Perforation, HUS: Head Ultrasound, SNAP: Score for Neonatal Acute Physiology
CP: Cerebral Palsy, MI: Motor Impairment, SIP: Spontaneous intestinal Perforation, HUS: Head Ultrasound, SNAP: Score for Neonatal Acute Physiology
*(weight z-score at discharge – weight z-score at birth) compared to 2nd Tertile
# (weight z-score at DOL 28– birth weight z-score) compared to 2nd Tertile
Objective: To identify perinatal factors in infants born EP that are associated with diagnosis of CP/MI at 2 and 10 years of age to inform the design of a predictive algorithm to estimate the risk, at NICU discharge, of receiving a diagnosis of CP/MI during childhood.
Design/Methods: Participants were enrolled at birth in the Extremely Low Gestational Age Newborn (ELGAN) Study between 2002 and 2004. Based on a standard neurological examination at 2 and the Gross Motor Function Classification System at 10 years of age, 849 participants (71% of survivors) were classified as follows: No CP/MI, CP only at 2 years, MI only at 10 years and CP/MI at both 2 and 10 years. To describe associations, between risk factors and CP/M, odds ratios (OR) and 95% confidence intervals (CI) were estimated using logistic regression, with no CP/MI at age 2 and age 10 as the referent group.
Results: Overall, 849 study participants underwent evaluation for CP/MI at 2 and 10 years of age. Of these, 64 (7.5%) had a diagnosis of CP/MI at both 2 and 10 years, while an additional 63 (7.4%) participants had a diagnosis of CP/MI at one visit but not the other (Table 1). Of 22 total risk factors queried, the strongest association with diagnosis of CP/MI at 2 and 10 years of age was seen with ventriculomegaly (OR 22.2, CI 12.0-41.2), periventricular leukomalacia (PVL), (OR 14.1, CI 7.7 - 25.8) and echogenicity on head ultrasound (OR 8.1, CI 4.5 – 14.5.) (Table 2).Conclusion(s): In the ELGAN cohort, the diagnosis of CP at 2 years did not always predict a diagnosis of MI at 10 years. We identified multiple clinical risk factors predictive of CP/MI, that are currently being used to compare individuals with a persistent diagnoses of CP/MI and those whose MI resolved, as well as to construct a predictive algorithm to estimate the risk.
Table 1. Baseline prenatal, perinatal and postnatal factors for CP/MI diagnosis at 2 and/or 10 years of age
.png) CP: Cerebral Palsy, MI: Motor Impairment, SIP: Spontaneous intestinal Perforation, HUS: Head Ultrasound, SNAP: Score for Neonatal Acute Physiology
CP: Cerebral Palsy, MI: Motor Impairment, SIP: Spontaneous intestinal Perforation, HUS: Head Ultrasound, SNAP: Score for Neonatal Acute Physiology*(weight z-score at discharge – weight z-score at birth)
# (weight z-score at discharge – weight z-score at DOL 28)
Table 2. Associated odds ratio for diagnosis of CP/MI by subgroups
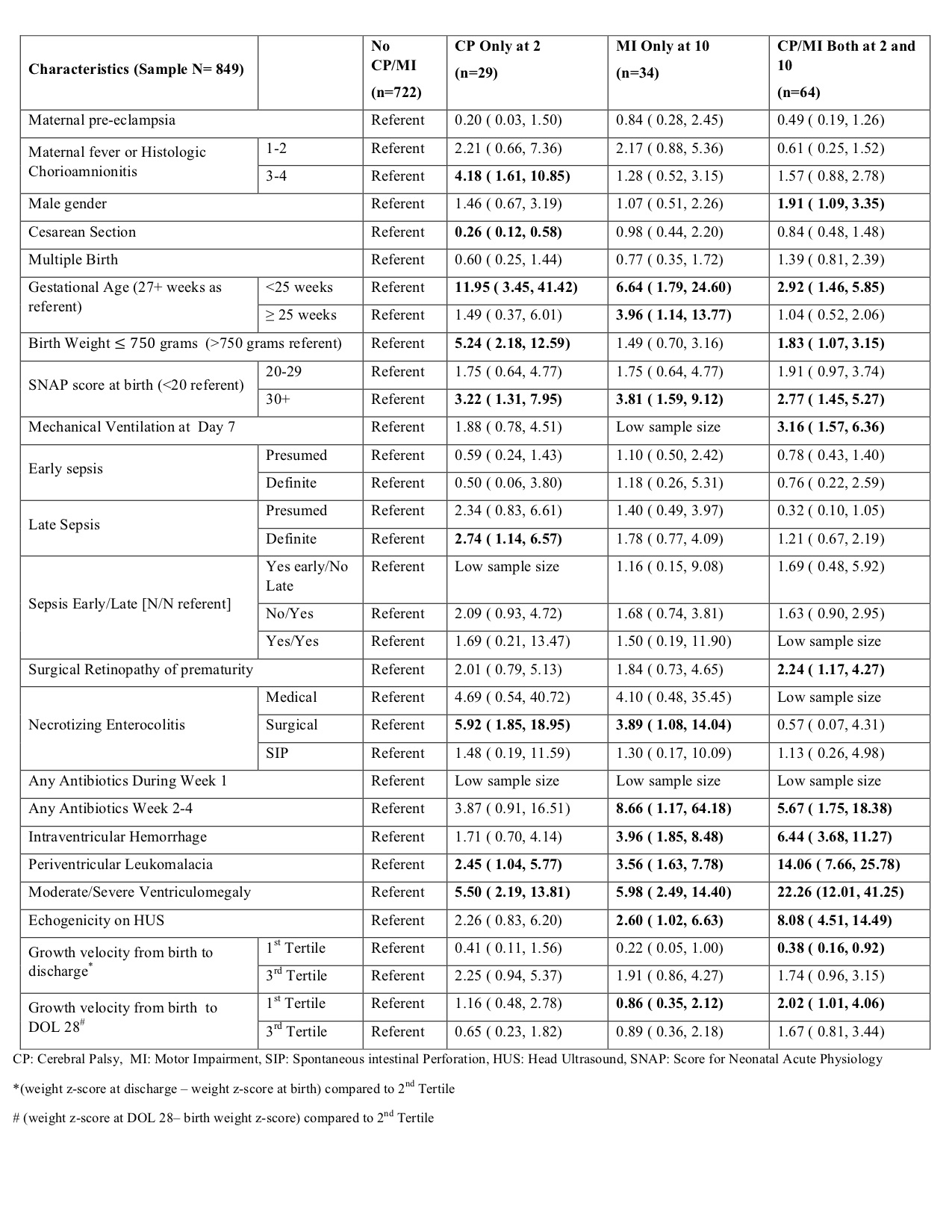 CP: Cerebral Palsy, MI: Motor Impairment, SIP: Spontaneous intestinal Perforation, HUS: Head Ultrasound, SNAP: Score for Neonatal Acute Physiology
CP: Cerebral Palsy, MI: Motor Impairment, SIP: Spontaneous intestinal Perforation, HUS: Head Ultrasound, SNAP: Score for Neonatal Acute Physiology*(weight z-score at discharge – weight z-score at birth) compared to 2nd Tertile
# (weight z-score at DOL 28– birth weight z-score) compared to 2nd Tertile
