Neonatal Clinical Trials
Category: Abstract Submission
Neonatal Clinical Trials I
423 - Cost-Effectiveness Of Heart Rate Characteristics Monitoring To Improve Survival For Very Low Birth Weight Infants
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 423
Publication Number: 423.223
Publication Number: 423.223
William E. King, MPSC, Charlottesville, VA, United States; Waldemar A. Carlo, University of Alabama at Birmingham, Birmingham, AL, United States; Michael O’Shea, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Robert Schelonka, Doernbecher Children's Hospital at Oregon Health & Science University, Lake Oswego, OR, United States

William E. King, MSEE
CEO
Medical Predictive Science Corporation
Charlottesville, Virginia, United States
Presenting Author(s)
Background: In a randomized controlled trial (RCT) of 3,003 very low birth weight (VLBW) patients, heart rate characteristics (HRC) monitoring (display) in addition to standard monitoring was associated with a 22% reduction in all-cause mortality when compared with standard monitoring alone (non-display).
Objective: We used data on resource utilization and outcomes from the RCT to analyze the cost-effectiveness of heart rate characteristics (HRC) monitoring.
Design/Methods: We performed a secondary analysis of cost-effectiveness from a third-party payer’s perspective where we included the direct medical costs and overhead from birth to NICU discharge, up to 120 days. We estimated each patient’s cost using the resource utilization data that was gathered during the RCT during their initial stay in the NICU and applied those data to per diem rates based on the patient’s postnatal age and level of acuity, as follows: Day 1: $4241 (ventilated) vs $1442 (non-ventilated), Days 2-28: $3562 (ventilated) vs $1164 (non-ventilated), and Days 29+: $3577 (ventilated) vs $1164 (non-ventilated). We included the cost of HRC-monitoring for those patients randomized to HRC-display. We computed the incremental cost-effectiveness ratio by calculating the difference in mean cost between the patients randomized to HRC-display versus non-display and dividing by the difference in survival between the two randomization arms. We used nonparametric boot-strapping to evaluate the uncertainty of these estimates. Costs are presented in 2021 US Dollars.
Results: Total cost of care for patients randomized to HRC-display was $108,834 (SD: $85,454) versus $108,066 (SD: $86,877) for non-display. Survival among HRC-display patients versus non-display patients was 91.7% versus 89.5%, respectively, during the 120-day time interval beginning at birth.
This analysis of cost-effectiveness revealed small increases in both mean cost ($768 / patient) and effectiveness (2.2% absolute increase in survival) for patients randomized to HRC-display. From these figures, we calculated the incremental cost-effectiveness ratio as $34,720 per life saved.
In bootstrapping, we found the median estimate of cost to save one additional life through HRC monitoring was $41,546; and the 95th percentile, corresponding to a traditional confidence interval limit, was $459,840. At a willingness-to-pay threshold of $10M, there was a 99% probability that HRC-monitoring is cost-effective.Conclusion(s): HRC-monitoring is cost-effective for increasing survival among VLBW infants.
Table 1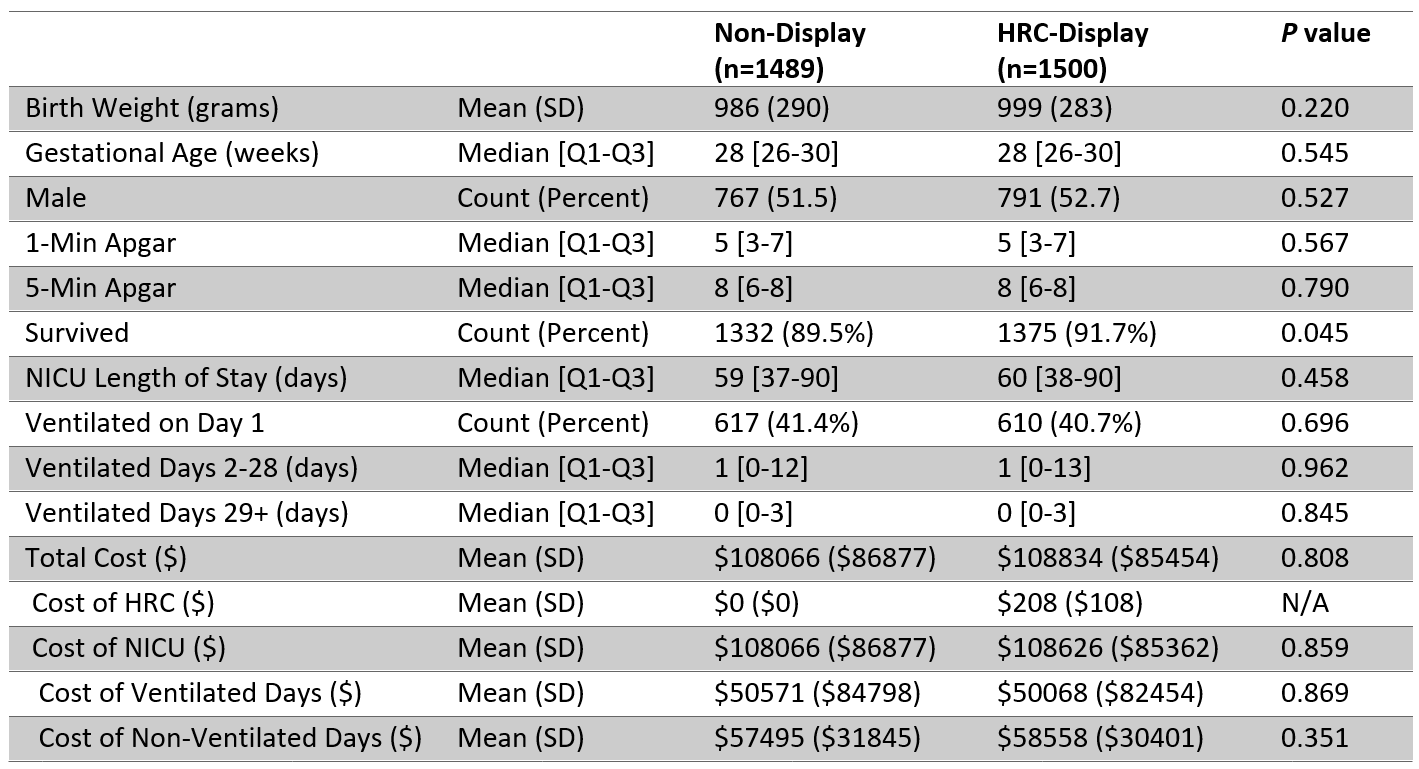 Demographics, Mortality, and Resource Utilization by Randomization Arm. A 2-sided t test is used to assess the significance of continuous variables, a Wilcoxon rank-sum test for ordinal variables, and a test for equality of proportions for categorical variables.
Demographics, Mortality, and Resource Utilization by Randomization Arm. A 2-sided t test is used to assess the significance of continuous variables, a Wilcoxon rank-sum test for ordinal variables, and a test for equality of proportions for categorical variables.
Figure 1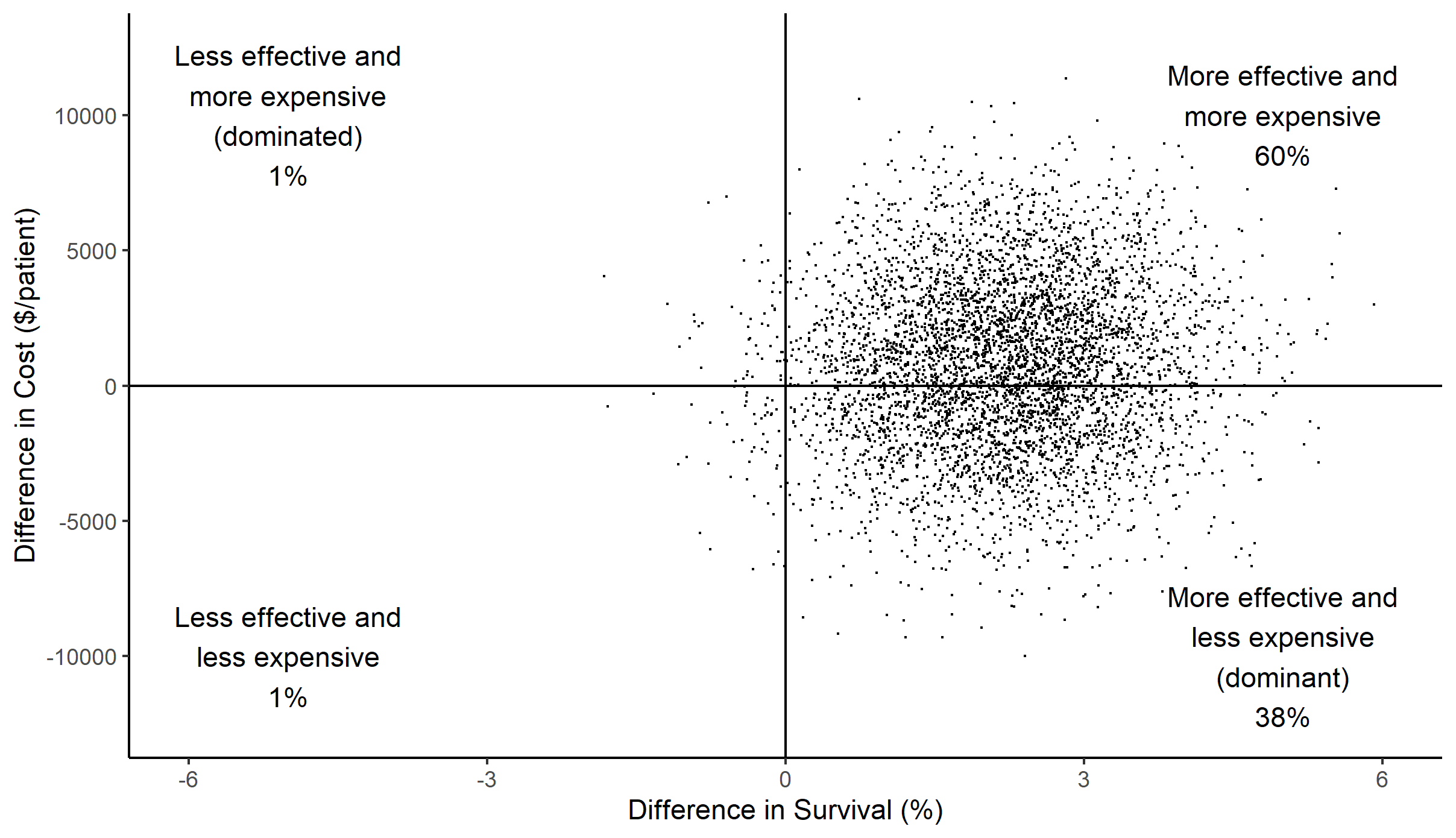 Scatterplot of difference in cost versus difference in effect (survival) between HRC-display and non-display arms for each of 5000 simulations. A large majority of points fall in the right half of the graph, indicating that HRC-monitoring was effective at reducing mortality; the smaller majority of data in the top half indicates that differences in cost were modest.
Scatterplot of difference in cost versus difference in effect (survival) between HRC-display and non-display arms for each of 5000 simulations. A large majority of points fall in the right half of the graph, indicating that HRC-monitoring was effective at reducing mortality; the smaller majority of data in the top half indicates that differences in cost were modest.
Objective: We used data on resource utilization and outcomes from the RCT to analyze the cost-effectiveness of heart rate characteristics (HRC) monitoring.
Design/Methods: We performed a secondary analysis of cost-effectiveness from a third-party payer’s perspective where we included the direct medical costs and overhead from birth to NICU discharge, up to 120 days. We estimated each patient’s cost using the resource utilization data that was gathered during the RCT during their initial stay in the NICU and applied those data to per diem rates based on the patient’s postnatal age and level of acuity, as follows: Day 1: $4241 (ventilated) vs $1442 (non-ventilated), Days 2-28: $3562 (ventilated) vs $1164 (non-ventilated), and Days 29+: $3577 (ventilated) vs $1164 (non-ventilated). We included the cost of HRC-monitoring for those patients randomized to HRC-display. We computed the incremental cost-effectiveness ratio by calculating the difference in mean cost between the patients randomized to HRC-display versus non-display and dividing by the difference in survival between the two randomization arms. We used nonparametric boot-strapping to evaluate the uncertainty of these estimates. Costs are presented in 2021 US Dollars.
Results: Total cost of care for patients randomized to HRC-display was $108,834 (SD: $85,454) versus $108,066 (SD: $86,877) for non-display. Survival among HRC-display patients versus non-display patients was 91.7% versus 89.5%, respectively, during the 120-day time interval beginning at birth.
This analysis of cost-effectiveness revealed small increases in both mean cost ($768 / patient) and effectiveness (2.2% absolute increase in survival) for patients randomized to HRC-display. From these figures, we calculated the incremental cost-effectiveness ratio as $34,720 per life saved.
In bootstrapping, we found the median estimate of cost to save one additional life through HRC monitoring was $41,546; and the 95th percentile, corresponding to a traditional confidence interval limit, was $459,840. At a willingness-to-pay threshold of $10M, there was a 99% probability that HRC-monitoring is cost-effective.Conclusion(s): HRC-monitoring is cost-effective for increasing survival among VLBW infants.
Table 1
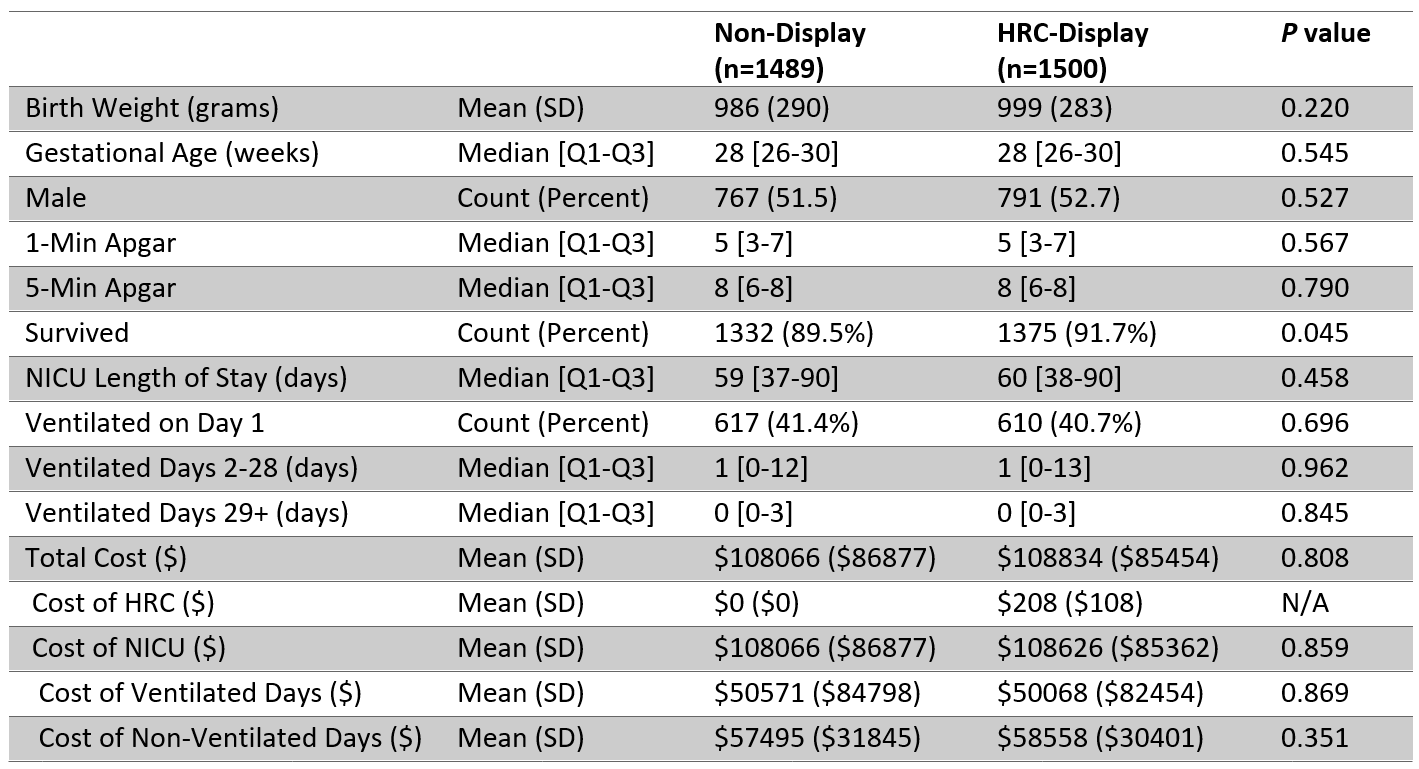 Demographics, Mortality, and Resource Utilization by Randomization Arm. A 2-sided t test is used to assess the significance of continuous variables, a Wilcoxon rank-sum test for ordinal variables, and a test for equality of proportions for categorical variables.
Demographics, Mortality, and Resource Utilization by Randomization Arm. A 2-sided t test is used to assess the significance of continuous variables, a Wilcoxon rank-sum test for ordinal variables, and a test for equality of proportions for categorical variables.Figure 1
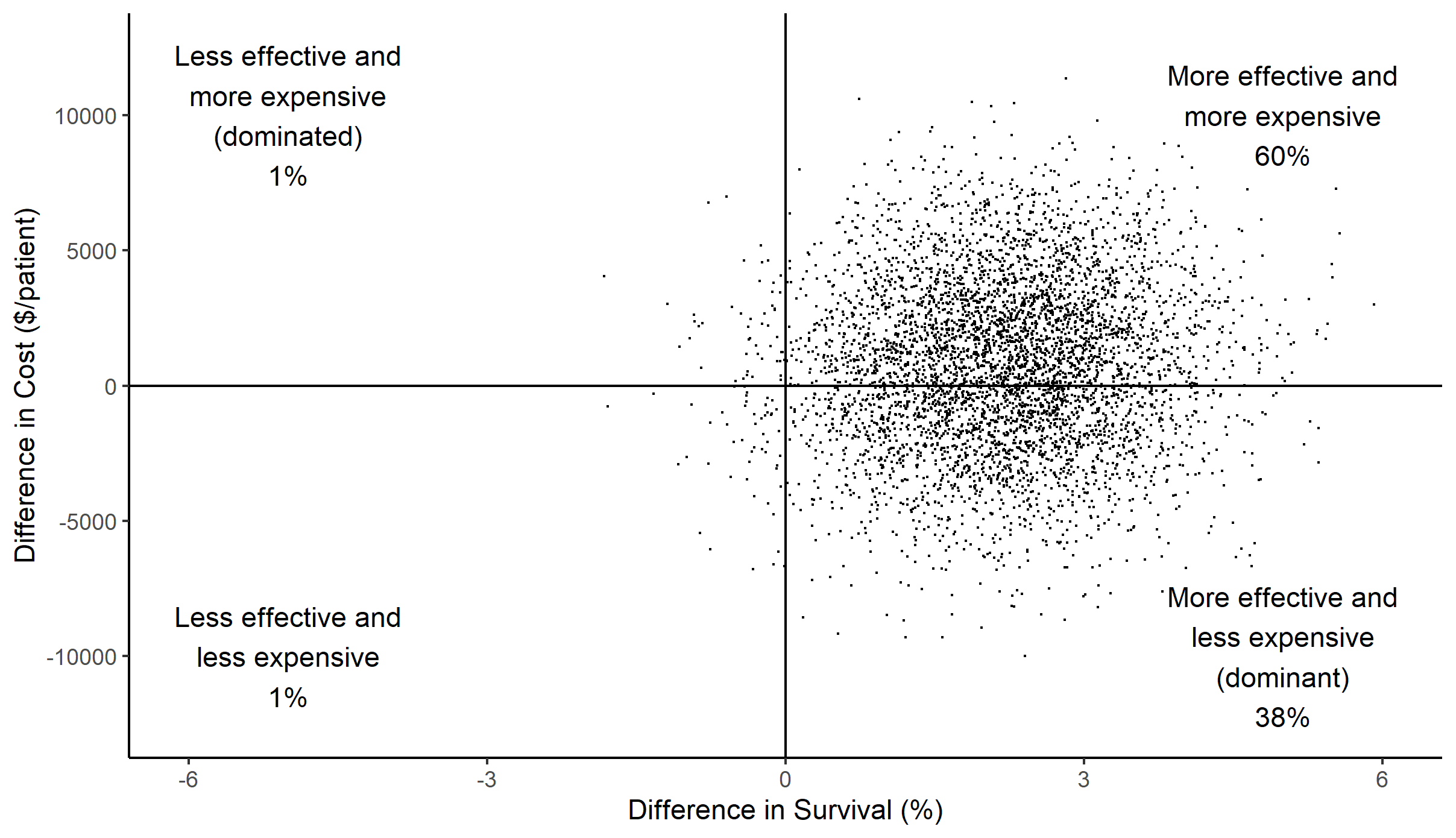 Scatterplot of difference in cost versus difference in effect (survival) between HRC-display and non-display arms for each of 5000 simulations. A large majority of points fall in the right half of the graph, indicating that HRC-monitoring was effective at reducing mortality; the smaller majority of data in the top half indicates that differences in cost were modest.
Scatterplot of difference in cost versus difference in effect (survival) between HRC-display and non-display arms for each of 5000 simulations. A large majority of points fall in the right half of the graph, indicating that HRC-monitoring was effective at reducing mortality; the smaller majority of data in the top half indicates that differences in cost were modest.