Medical Education: Resident
Category: Abstract Submission
Medical Education 7 - Medical Education: Potpourri
149 - EHR Order Metadata Identifies Gaps in Pediatric Trainee Education
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 149
Publication Number: 149.218
Publication Number: 149.218
Andrew Pulfer, University of Rochester School of Medicine and Dentistry, Rochester, NY, United States; Mark Mai, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Naveen Muthu, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Adam Dziorny, University of Rochester School of Medicine, Rochester, NY, United States
- AP
Andrew Pulfer, MD
Resident Physician
University of Rochester School of Medicine and Dentistry
Rochester, New York, United States
Presenting Author(s)
Background: Clinical encounters as experiential learning provide a significant portion of resident education. Quantifying these experiences is vital to identifying education gaps, yet remains challenging. The COVID-19 pandemic has decreased patient volumes across pediatric hospital settings, limiting these learning opportunities for trainee physicians. Paradoxically this decrease was seen specifically among patients with respiratory illnesses.
Objective: EHR metadata including orders placed by residents may provide automated, surrogate measures of clinical experience. We hypothesize that these metadata will demonstrate a decrease in respiratory illness management during the pandemic, compared to prior (non-pandemic) years.
Design/Methods: Retrospective cohort study at the University of Rochester Medical Center (URMC) and the Children’s Hospital of Philadelphia (CHOP). We included first-year pediatrics residents in the exposure cohort (2020) and three control cohorts (2017, 2018, and 2019), one of which (2019) included a mixture exposure and non-exposure cohort. We collected order data from Epic (Epic Systems, Verona WI) Clarity database and limited to those orders placed on inpatient pediatric floors. We quantified total orders, those classified as “respiratory” by the EHR, and those used in management of common respiratory illnesses. Comparison included Kruskal-Wallis testing with Wilcoxon signed rank test, and multivariate regression.
Results: We included 207 residents across two sites, with 1,167,429 orders placed on inpatient units. Total orders placed in 2020 (Figure 1), as well as respiratory orders, showed a statistically significant decrease when compared to all other years (URMC) and to the both control non-pandemic years (CHOP). Orders for albuterol and high flow nasal cannula, as surrogates for asthma and bronchiolitis management, respectively, decreased significantly (all models: p< 0.001) at both sites compared to prior years (Table 1).Conclusion(s): First-year pediatric residents at two institutions placed fewer total and respiratory illness related orders during the COVID-19 pandemic. In this study we focused on two common pediatric respiratory illness, asthma and bronchiolitis, and examined orders related to the management of these illnesses. EHR order metadata, when applied to residents, may be a surrogate for disease management. Metadata analyses can quantify the impact of curricular change on trainees, and may be used to focus non-clinical education.
Figure 1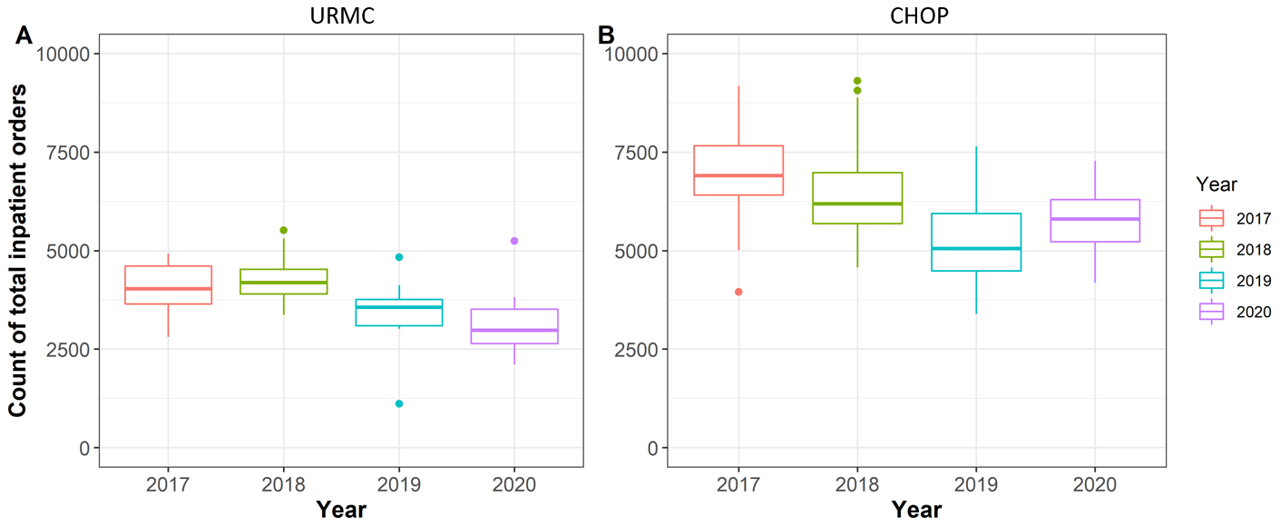 Total number of orders placed by individual residents year by year
Total number of orders placed by individual residents year by year
Table 1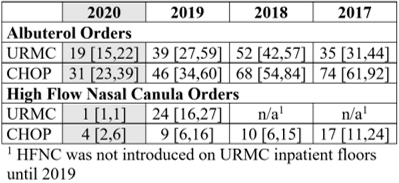 Respiratory orders per resident by site (median, IQR)
Respiratory orders per resident by site (median, IQR)
Objective: EHR metadata including orders placed by residents may provide automated, surrogate measures of clinical experience. We hypothesize that these metadata will demonstrate a decrease in respiratory illness management during the pandemic, compared to prior (non-pandemic) years.
Design/Methods: Retrospective cohort study at the University of Rochester Medical Center (URMC) and the Children’s Hospital of Philadelphia (CHOP). We included first-year pediatrics residents in the exposure cohort (2020) and three control cohorts (2017, 2018, and 2019), one of which (2019) included a mixture exposure and non-exposure cohort. We collected order data from Epic (Epic Systems, Verona WI) Clarity database and limited to those orders placed on inpatient pediatric floors. We quantified total orders, those classified as “respiratory” by the EHR, and those used in management of common respiratory illnesses. Comparison included Kruskal-Wallis testing with Wilcoxon signed rank test, and multivariate regression.
Results: We included 207 residents across two sites, with 1,167,429 orders placed on inpatient units. Total orders placed in 2020 (Figure 1), as well as respiratory orders, showed a statistically significant decrease when compared to all other years (URMC) and to the both control non-pandemic years (CHOP). Orders for albuterol and high flow nasal cannula, as surrogates for asthma and bronchiolitis management, respectively, decreased significantly (all models: p< 0.001) at both sites compared to prior years (Table 1).Conclusion(s): First-year pediatric residents at two institutions placed fewer total and respiratory illness related orders during the COVID-19 pandemic. In this study we focused on two common pediatric respiratory illness, asthma and bronchiolitis, and examined orders related to the management of these illnesses. EHR order metadata, when applied to residents, may be a surrogate for disease management. Metadata analyses can quantify the impact of curricular change on trainees, and may be used to focus non-clinical education.
Figure 1
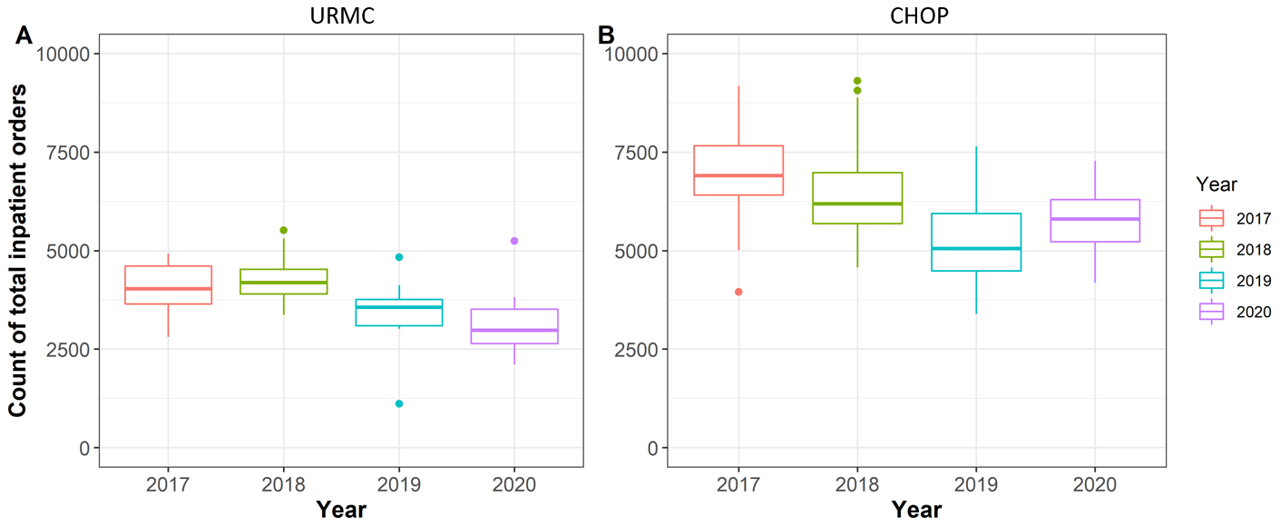 Total number of orders placed by individual residents year by year
Total number of orders placed by individual residents year by yearTable 1
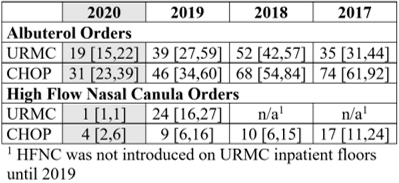 Respiratory orders per resident by site (median, IQR)
Respiratory orders per resident by site (median, IQR)