Neonatal Respiratory Assessment/Support/Ventilation
Category: Abstract Submission
Neonatal Respiratory II: Respiratory Physiology and Devices
449 - End tidal carbon dioxide monitoring in neonates receiving therapeutic hypothermia for hypoxic- ischemic encephalopathy
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 449
Publication Number: 449.228
Publication Number: 449.228
Enikő Szakmár, Semmelweis University, Budapest, Budapest, Hungary; Marianna Dobi, Semmelweis University, Budapest, Budapest, Hungary; Kata Kovacs, Semmelweis University, Budapest, Pest, Hungary; Vera Balog, Semmelweis University, Budapest, Budapest, Hungary; Mate Detar, 1st Department of Pediatrics, Semmelweis University, Vésztö, Bekes, Hungary; Miklós Szabó, Division of Neonatology Ist Dept. of Pediatrics Semmelweis University, Budapest, Budapest, Hungary; Agnes Jermendy, Semmelweis University, Budapest, Budapest, Hungary

Eniko Szakmar, MD, PhD
Pediatric Resident
Semmelweis University
Budapest, Hungary
Presenting Author(s)
Background: The consistent findings of the association between hypocapnia and adverse outcomes in infants with hypoxic-ischemic encephalopathy (HIE) suggest that the continuous carbon dioxide (CO2) monitoring should be encouraged. End tidal CO2 (etCO2) monitoring enables the prevention of undesired PCO2 levels by facilitating immediate intervention.
Objective: The primary aim was to evaluate the agreement between etCO2 and temperature corrected PCO2 values in patients with HIE receiving therapeutic hypothermia (TH). Secondary, to assess the percentage of time spent in hypocapnia ( <35 mmHg) based on the continuous etCO2 monitoring.
Design/Methods: In this prospective observational single center trial, infants receiving TH for HIE at the 1st Department of Pediatrics, Semmelweis University between December 2020 to October 2021 were enrolled. Neonates during TH are mechanically ventilated as per local protocol. The level of etCO2 was monitored via Capnostream 35 portable respiratory monitor using sidestream end tidal capnography with 20/s sampling rate. The mean etCO2 was determined over 10 min periods preceding the time of the blood gases. The agreement between etCO2 and temperature corrected arterial and capillary PCO2 was analyzed by using the Bland- Altman plots.
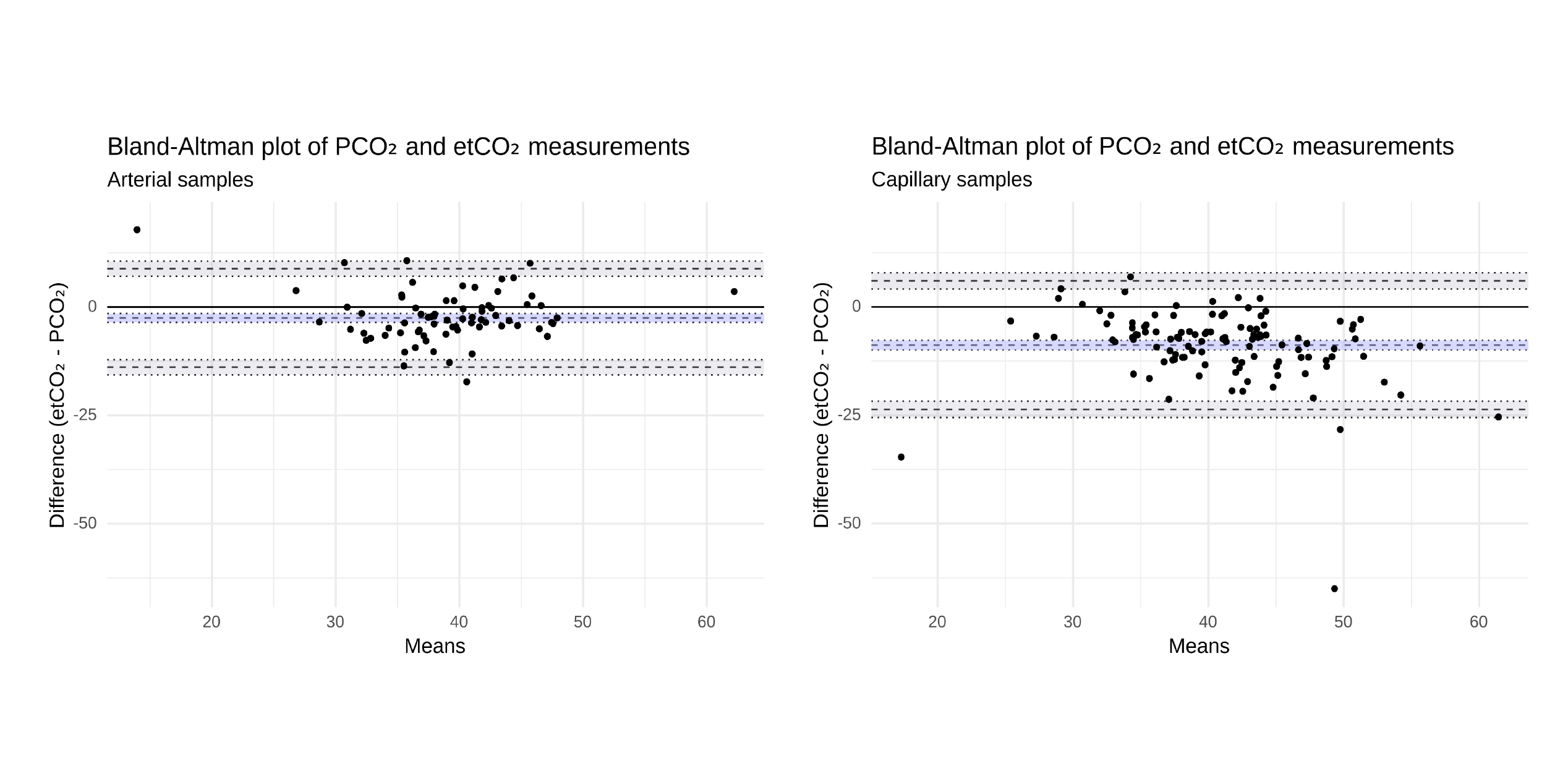
Results: Twenty-six mechanically ventilated infants with HIE were assigned to the trial, and were monitored for etCO2 for a median 70 [IQR 63; 78] hours, starting from a median 12 [IQR 7; 23] hours of life until 85 [IQR 78; 97] hours of life corresponding to hypothermia and rewarming. A total of 315 paired etCO2 and temperature corrected PCO2 measurements were analyzed including 130 arterial and 185 capillary samples. The etCO2 was closely related to the arterial PCO2 with the average difference of -2.5 mmHg (limits of agreement -13.9; 8.9 mmHg), whereas etCO2 underestimated capillary PCO2 values by -8.8 mmHg on average with -23.6; 6.0 mmHg limits of agreement (Figure 1). After the exclusion of 7 patients with pulmonary morbidities, the agreements did not improve. Neonates spent a median 31% [IQR 14; 44] of time below 35 mmHg. Conclusion(s): There was a strong level of agreement between the gold standard arterial PCO2 and etCO2 values. Hypocapnia was frequent based on continuous etCO2 measurements in mechanically ventilated infants during hypothermia. The routine use of continuous etCO2 monitoring has the potential to improve the intensive care of newborns with HIE by avoiding hypocapnia.
Bland- Altman plots of PCO2 and etCO2 measurements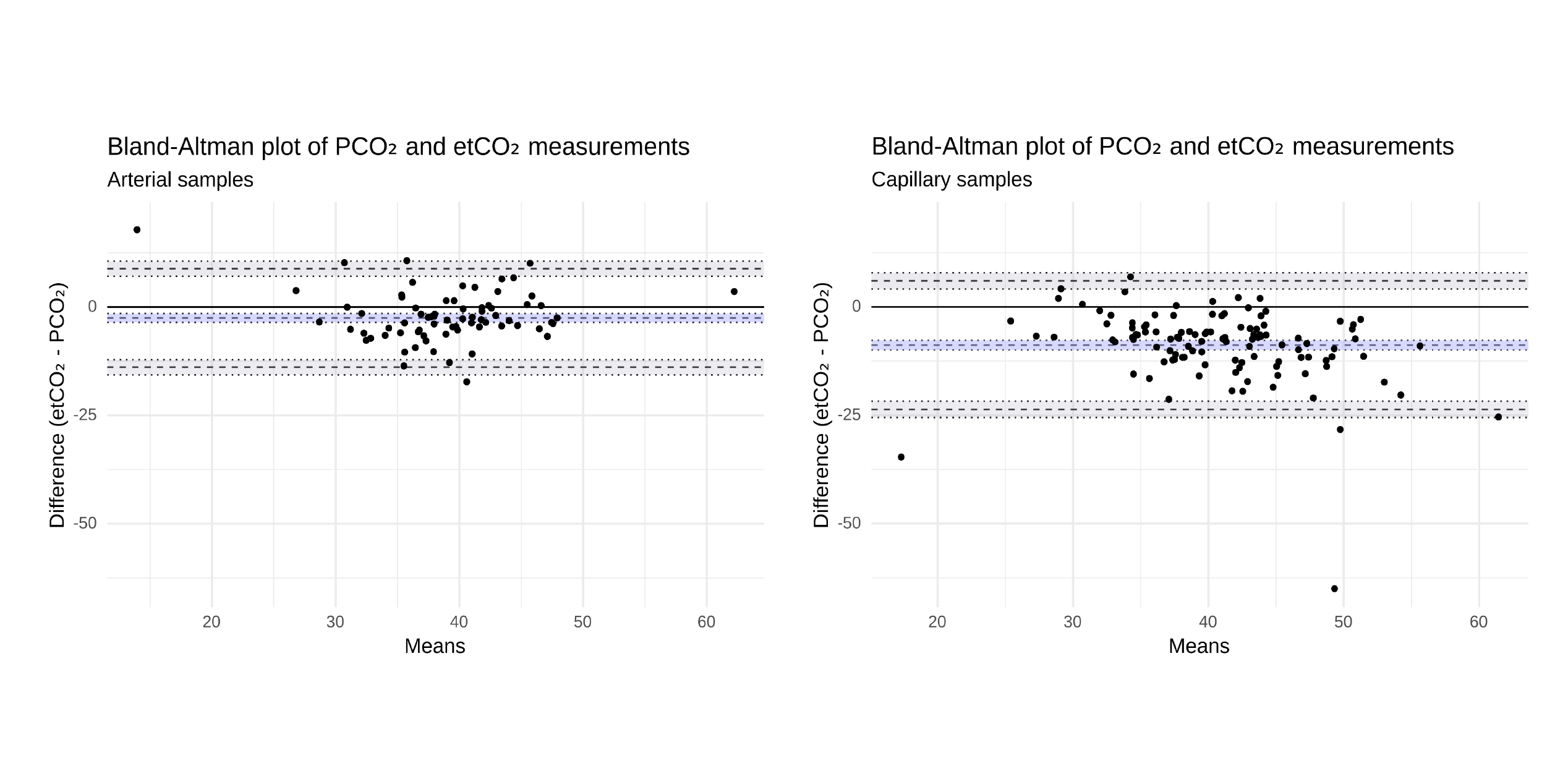
Objective: The primary aim was to evaluate the agreement between etCO2 and temperature corrected PCO2 values in patients with HIE receiving therapeutic hypothermia (TH). Secondary, to assess the percentage of time spent in hypocapnia ( <35 mmHg) based on the continuous etCO2 monitoring.
Design/Methods: In this prospective observational single center trial, infants receiving TH for HIE at the 1st Department of Pediatrics, Semmelweis University between December 2020 to October 2021 were enrolled. Neonates during TH are mechanically ventilated as per local protocol. The level of etCO2 was monitored via Capnostream 35 portable respiratory monitor using sidestream end tidal capnography with 20/s sampling rate. The mean etCO2 was determined over 10 min periods preceding the time of the blood gases. The agreement between etCO2 and temperature corrected arterial and capillary PCO2 was analyzed by using the Bland- Altman plots.
Results: Twenty-six mechanically ventilated infants with HIE were assigned to the trial, and were monitored for etCO2 for a median 70 [IQR 63; 78] hours, starting from a median 12 [IQR 7; 23] hours of life until 85 [IQR 78; 97] hours of life corresponding to hypothermia and rewarming. A total of 315 paired etCO2 and temperature corrected PCO2 measurements were analyzed including 130 arterial and 185 capillary samples. The etCO2 was closely related to the arterial PCO2 with the average difference of -2.5 mmHg (limits of agreement -13.9; 8.9 mmHg), whereas etCO2 underestimated capillary PCO2 values by -8.8 mmHg on average with -23.6; 6.0 mmHg limits of agreement (Figure 1). After the exclusion of 7 patients with pulmonary morbidities, the agreements did not improve. Neonates spent a median 31% [IQR 14; 44] of time below 35 mmHg. Conclusion(s): There was a strong level of agreement between the gold standard arterial PCO2 and etCO2 values. Hypocapnia was frequent based on continuous etCO2 measurements in mechanically ventilated infants during hypothermia. The routine use of continuous etCO2 monitoring has the potential to improve the intensive care of newborns with HIE by avoiding hypocapnia.
Bland- Altman plots of PCO2 and etCO2 measurements