Neonatal Respiratory Assessment/Support/Ventilation
Category: Abstract Submission
Neonatal Respiratory I: RDS and Surfactant
440 - Frequency of Hypercarbia Following Non-Emergent Neonatal Tracheal Intubation
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 440
Publication Number: 440.227
Publication Number: 440.227
Rebecca Shay, University of Colorado Hospital, Denver, CO, United States; Blair W. Weikel, University of Colorado Anschutz Medical Campus, Aurora, CO, United States; Theresa Grover, University of Colorado School of Medicine, Aurora, CO, United States; James S. Barry, University of Colorado, centennial, CO, United States

Rebecca Shay, MD, MAS
Neonatologist
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Hypercarbia and acute changes in partial pressure of carbon dioxide (pCO2) concentrations have been associated with increased pulmonary vascular resistance, increased cerebral blood flow, and reduced muscle contractility. The effect of sedation, analgesia, and paralysis on ventilation during and after neonatal intubation is unknown.
Objective: The objective of this retrospective, observational study, as part of a larger quality improvement initiative, was to document the frequency of hypercarbia following non-emergent neonatal TI at University of Colorado (UCH) and Children’s Hospital Colorado (CHCO) NICU. Secondary objectives were to identify predictors of neonatal hypercarbia related to premedication and infant characteristics.
Design/Methods: A retrospective chart review was completed from January to June 2021. For each non-emergent neonatal TI, pre-intubation and post-intubation blood gases we compared. Frequency of rising pCO2, rising pCO2 to a value > 65 mmHg, and pCO2 that rose > 10 mmHg were recorded. Clinical variables and outcomes were compared using the Student’s t-tests for continuous parametric data, Mann-Whitney-Wilcoxon test for continuous nonparametric data, and Fisher’s exact tests for categorical variables.
Results: 202 neonatal TI were studied over a six-month period. Day-of-life (DOL), gestational age (GA), post-menstrual age (PMA), and weight at the time of the procedure were documented. At UCH, pCO2 rose in 46.9%, pCO2 rose to a value ≥ 65 mmHg in 19.8%, and pCO2 rose ≥ 10 mmHg in 27.2% of the TI. At CHCO, pCO2 rose in 34.7%, pCO2 rose to a value ≥ 65 mmHg in 18.2%, and pCO2 rose ≥ 10 mmHg in 14.9% of the TI. There were no statistically significant differences between premedication regimens. (Table 1, Table 2). The same outcome variables were compared across infant characteristics. At UCH, infants that had a pCO2 that rose to a value ≥ 65 mmHg were more likely to have a lower PMA. At CHCO, infants that had a pCO2 that rose ≥ 10 mmHg were more likely to have a lower GA. Otherwise, there were no significant differences between the groups (Table 3).Conclusion(s): Post-intubation hypercarbia occurred frequently and was independent of premedication provided in our cohort. With current momentum to improve neonatal intubation safety, evaluating the effect of patient and practice variables on ventilation should be an important goal. Larger data sets can be studied to assess for associations to plan for improvement initiatives addressing this component of intubation practice.
Table 1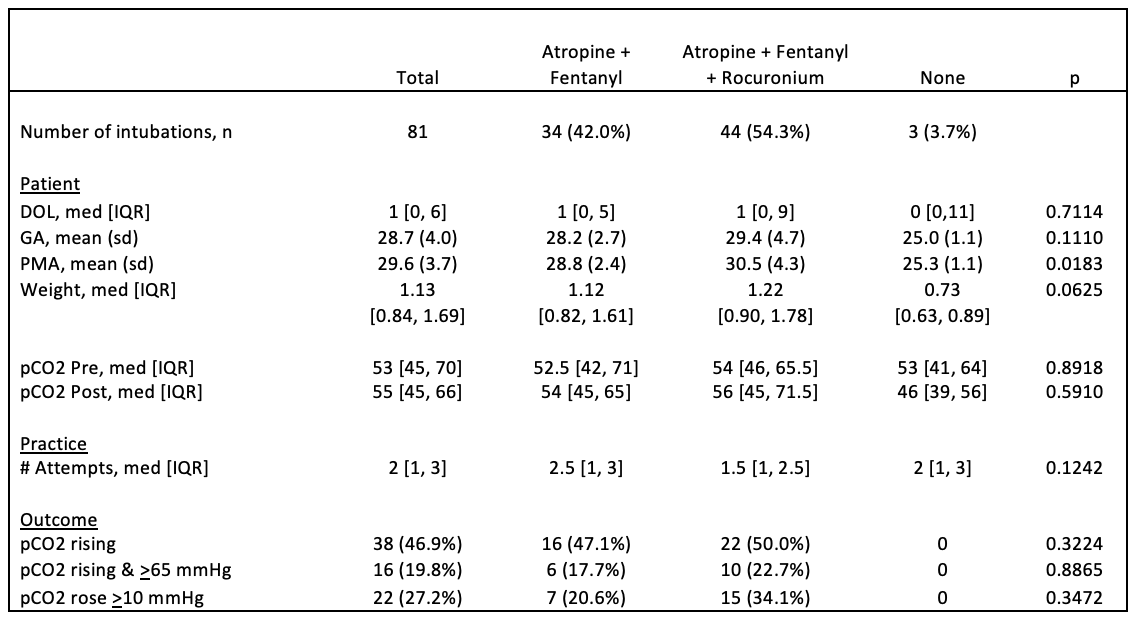 UCH Intubation Characteristics and Post-intubation Blood Gas Outcomes by Premedication Regimen
UCH Intubation Characteristics and Post-intubation Blood Gas Outcomes by Premedication Regimen
Table 2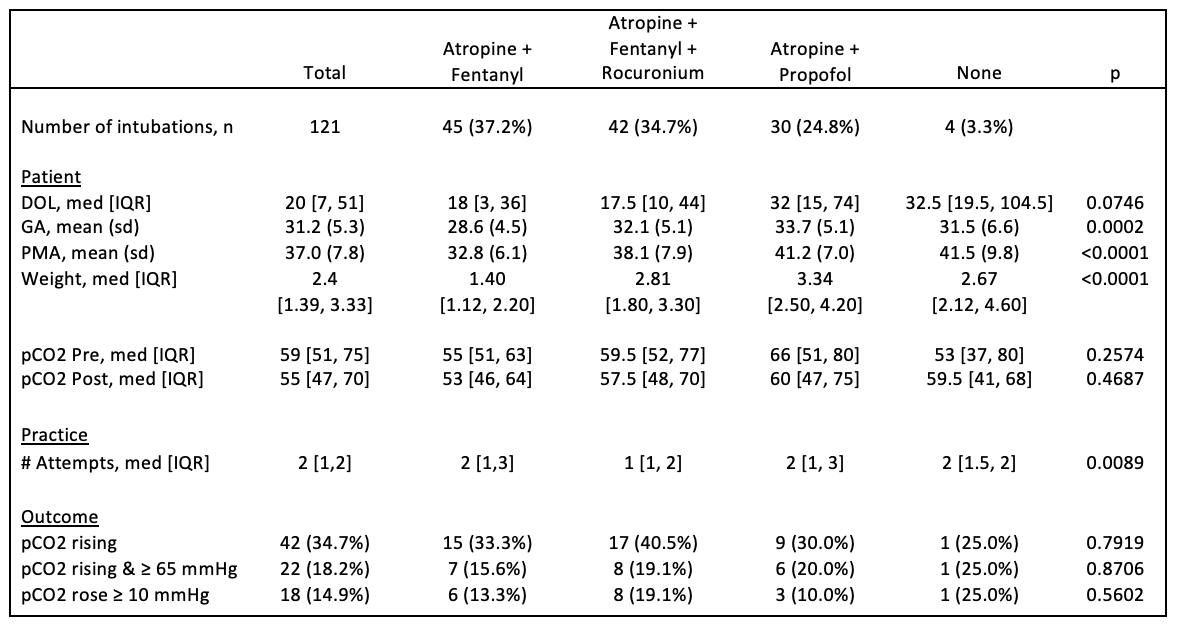 CHCO Intubation Characteristics and Post-intubation Blood Gas Outcomes by Premedication Regimen
CHCO Intubation Characteristics and Post-intubation Blood Gas Outcomes by Premedication Regimen
Objective: The objective of this retrospective, observational study, as part of a larger quality improvement initiative, was to document the frequency of hypercarbia following non-emergent neonatal TI at University of Colorado (UCH) and Children’s Hospital Colorado (CHCO) NICU. Secondary objectives were to identify predictors of neonatal hypercarbia related to premedication and infant characteristics.
Design/Methods: A retrospective chart review was completed from January to June 2021. For each non-emergent neonatal TI, pre-intubation and post-intubation blood gases we compared. Frequency of rising pCO2, rising pCO2 to a value > 65 mmHg, and pCO2 that rose > 10 mmHg were recorded. Clinical variables and outcomes were compared using the Student’s t-tests for continuous parametric data, Mann-Whitney-Wilcoxon test for continuous nonparametric data, and Fisher’s exact tests for categorical variables.
Results: 202 neonatal TI were studied over a six-month period. Day-of-life (DOL), gestational age (GA), post-menstrual age (PMA), and weight at the time of the procedure were documented. At UCH, pCO2 rose in 46.9%, pCO2 rose to a value ≥ 65 mmHg in 19.8%, and pCO2 rose ≥ 10 mmHg in 27.2% of the TI. At CHCO, pCO2 rose in 34.7%, pCO2 rose to a value ≥ 65 mmHg in 18.2%, and pCO2 rose ≥ 10 mmHg in 14.9% of the TI. There were no statistically significant differences between premedication regimens. (Table 1, Table 2). The same outcome variables were compared across infant characteristics. At UCH, infants that had a pCO2 that rose to a value ≥ 65 mmHg were more likely to have a lower PMA. At CHCO, infants that had a pCO2 that rose ≥ 10 mmHg were more likely to have a lower GA. Otherwise, there were no significant differences between the groups (Table 3).Conclusion(s): Post-intubation hypercarbia occurred frequently and was independent of premedication provided in our cohort. With current momentum to improve neonatal intubation safety, evaluating the effect of patient and practice variables on ventilation should be an important goal. Larger data sets can be studied to assess for associations to plan for improvement initiatives addressing this component of intubation practice.
Table 1
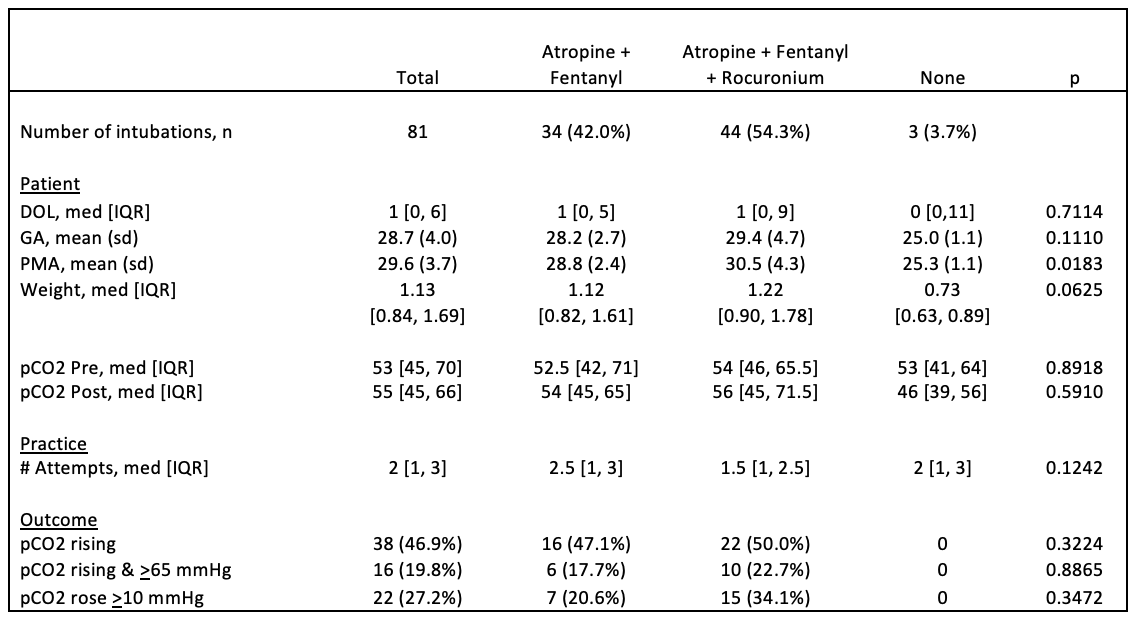 UCH Intubation Characteristics and Post-intubation Blood Gas Outcomes by Premedication Regimen
UCH Intubation Characteristics and Post-intubation Blood Gas Outcomes by Premedication RegimenTable 2
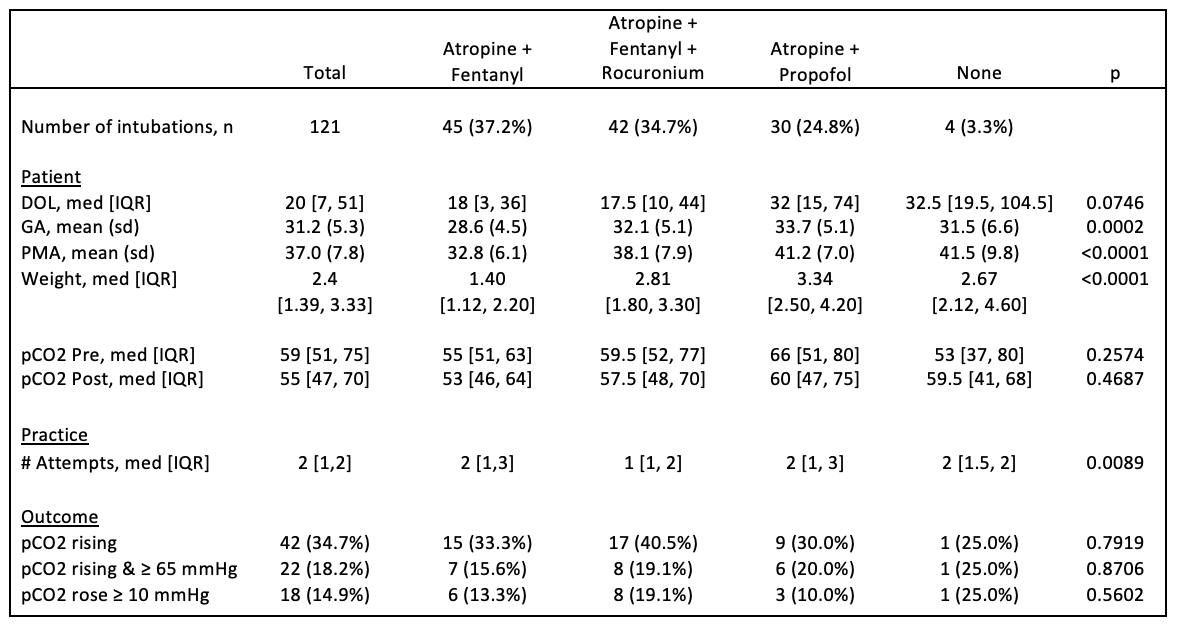 CHCO Intubation Characteristics and Post-intubation Blood Gas Outcomes by Premedication Regimen
CHCO Intubation Characteristics and Post-intubation Blood Gas Outcomes by Premedication Regimen