Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up III
265 - Functional Outcomes after Therapeutic Hypothermia (TH) for Hypoxic-Ischemic Encephalopathy (HIE) in Rural Settings
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 265
Publication Number: 265.225
Publication Number: 265.225
Melanie P. Parziale, Robert Larner, M.D., College of Medicine at the University of Vermont, Sharon, MA, United States; Deirdre O'Reilly, Robert Larner, M.D., College of Medicine at the University of Vermont, Burlington, VT, United States

Melanie P. Parziale
Medical Student
Robert Larner, M.D., College of Medicine at the University of Vermont
Sharon, Massachusetts, United States
Presenting Author(s)
Background: Infants that receive TH for HIE are at risk for neurodevelopmental deficits such as cerebral palsy (CP) or hearing/vision loss.1 2 Prognostication of long-term outcomes, while important to families3, is limited in the NICU, as neurologic exam and MRI are not sufficient to predict outcomes4. Disability at 18-24 months can be predictive of impairment later in life5, but in our rural state, formal neurodevelopmental follow-up has proven to be difficult.
Objective: We sought to Identify functional and parent-reported outcomes after TH for HIE in a single-center referral hospital, and to identify differences between those inborn compared to those transported across our catchment area throughout Vermont and New York.
Design/Methods: Analyses were conducted on infants receiving TH between 1/1/2010-7/1/2021 via data within a secure RedCap database, approved by our local IRB. We defined functional outcome as infant walking/GMFCS score, talking > 10 words, and feeding orally. Outcomes were recorded by reviewing UVM Health Network’s electronic health record, including standardized NICU follow-up as well as results from sick visits and routine pediatric visits at 20-28 months. Data was analyzed and significance assessed using Independent Sample t-test and Fisher’s Exact test.
Results: Ninety-four infants received TH. Fifty-seven infants were born at UVMMC, compared to 37 at community hospitals. Infants were similar between the 2 groups, except inborn infants had older mothers and started active cooling earlier. There was no difference in diagnosis of seizures, length of stay, or death between the two groups (Table 1). Of the 60 children born before 2020, 47 were seen at age 2. Outborn infants have significantly lower rates of walking and talking at 2 years of age (Table 2). The only infants who were not walking at age 2 were also diagnosed with CP. Bayley Scales of Infant Development-III examination was completed in only 14 of the 60 infants at 2 years of age.Conclusion(s): We identified parent and provider-identified functional outcomes for 78% of infants at age 2. Many infants did not receive early intervention services. Outborn infants had significantly higher rates of motor and speech delay and were assessed less often. Our findings can inform further quality improvement and research efforts to target services for infants, especially those born in rural settings. We will build upon these results to improve follow-up rate and communication between referral and community providers and families of infants affected by HIE.
Parziale CVParziale ERAS CV Aug 2021 (002).pdf
Table 2. Developmental Outcomes at Age 2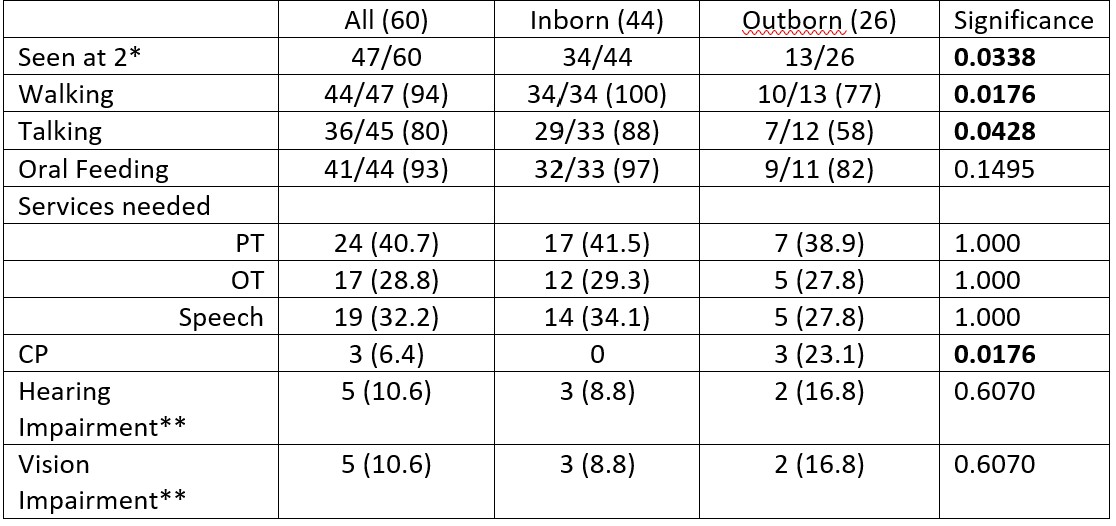 *89 infants survived hospitalization. At the time of submission, 60/89 infants reached 2 years of age and were retrospectively assessed for developmental outcomes between 20 and 28 months of age.
*89 infants survived hospitalization. At the time of submission, 60/89 infants reached 2 years of age and were retrospectively assessed for developmental outcomes between 20 and 28 months of age.
**Hearing impairment was defined as a failed hearing test (non-newborn screen) and vision impairment was defined as visual limitation and need for glasses.
Objective: We sought to Identify functional and parent-reported outcomes after TH for HIE in a single-center referral hospital, and to identify differences between those inborn compared to those transported across our catchment area throughout Vermont and New York.
Design/Methods: Analyses were conducted on infants receiving TH between 1/1/2010-7/1/2021 via data within a secure RedCap database, approved by our local IRB. We defined functional outcome as infant walking/GMFCS score, talking > 10 words, and feeding orally. Outcomes were recorded by reviewing UVM Health Network’s electronic health record, including standardized NICU follow-up as well as results from sick visits and routine pediatric visits at 20-28 months. Data was analyzed and significance assessed using Independent Sample t-test and Fisher’s Exact test.
Results: Ninety-four infants received TH. Fifty-seven infants were born at UVMMC, compared to 37 at community hospitals. Infants were similar between the 2 groups, except inborn infants had older mothers and started active cooling earlier. There was no difference in diagnosis of seizures, length of stay, or death between the two groups (Table 1). Of the 60 children born before 2020, 47 were seen at age 2. Outborn infants have significantly lower rates of walking and talking at 2 years of age (Table 2). The only infants who were not walking at age 2 were also diagnosed with CP. Bayley Scales of Infant Development-III examination was completed in only 14 of the 60 infants at 2 years of age.Conclusion(s): We identified parent and provider-identified functional outcomes for 78% of infants at age 2. Many infants did not receive early intervention services. Outborn infants had significantly higher rates of motor and speech delay and were assessed less often. Our findings can inform further quality improvement and research efforts to target services for infants, especially those born in rural settings. We will build upon these results to improve follow-up rate and communication between referral and community providers and families of infants affected by HIE.
Parziale CVParziale ERAS CV Aug 2021 (002).pdf
Table 2. Developmental Outcomes at Age 2
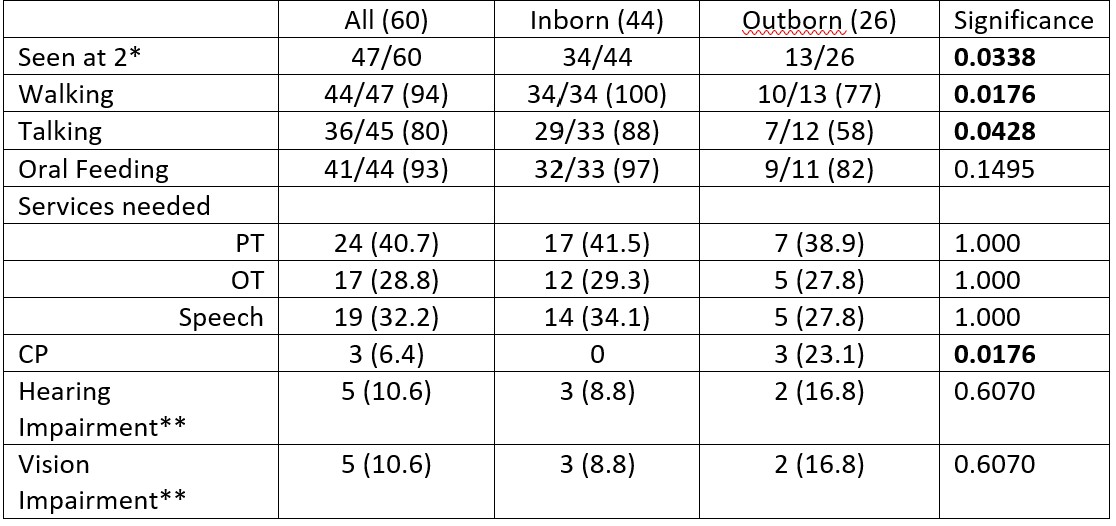 *89 infants survived hospitalization. At the time of submission, 60/89 infants reached 2 years of age and were retrospectively assessed for developmental outcomes between 20 and 28 months of age.
*89 infants survived hospitalization. At the time of submission, 60/89 infants reached 2 years of age and were retrospectively assessed for developmental outcomes between 20 and 28 months of age.**Hearing impairment was defined as a failed hearing test (non-newborn screen) and vision impairment was defined as visual limitation and need for glasses.
