Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up II
253 - HeRO scores, HIE, and developmental outcome: is there an association?
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 253
Publication Number: 253.224
Publication Number: 253.224
Megan A. Derrer, University of Wisconsin School of Medicine and Public Health, Deerfield, WI, United States; Janet M. Legare, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States

Megan A. Derrer, MD
Neonatal-Perinatal Medicine Fellow
University of Wisconsin School of Medicine and Public Health
Deerfield, Wisconsin, United States
Presenting Author(s)
Background: Heart rate variability falls during illness due to fewer microsecond alterations in sympathetic/parasympathetic input. Fetal heart rate monitoring of variability, accelerations, and decelerations reflect fetal distress. The NICU HeRO monitors generate a heart rate index, or HeRO score, with higher score predicting risk for deterioration from sepsis in preterm, ELBW infants. Scores >2 are abnormal. Intracranial abnormalities increase HeRO scores, with emerging work supporting that higher HeRO scores predict abnormal EEG, MRI, and death, or abnormal imaging and outcomes in ELBW infants. Clinicians struggle with interpreting HeRO scores in term infants with neurological conditions.
Objective: To determine baseline HeRO scores, examine influencing factors, and to investigate whether HeRO scores are associated with neurodevelopmental outcome in hypoxic encephalopathy (HIE).
Design/Methods: Retrospective cohort study was performed between May 2014-March 2021, manually reviewing electronic records of infants >35 weeks gestation with HIE undergoing therapeutic hypothermia. We excluded other encephalopathy, any genetic or metabolic disorder, or if cooled at other institutions. Data collection included maternal-child demographics, delivery mode, CPR at delivery, maternal history, infant lab values, HeRO scores (averaged over 12 hour blocks), imaging data, seizures, sepsis, other diagnoses and procedures, and cumulative sedative medications. Developmental outcomes with respect to feeding, communication, cognition, and motor skills were assessed. Descriptive data are summarized and mild-moderate-severe are determined with HIE staging criteria.
Results: 46 infants met criteria. Severity of HIE and demographics are summarized in Table 1. Only 50% had mean score >2 at any time and only 15% had mean score >5. 14/21 with mean HeRO score >2 were also diagnosed with clinical sepsis. 28/32 patients who attended follow up had concerns for abnormal development. Comparison of HIE severity and developmental outcomes is shown in Table 2.Conclusion(s): Although retrospective, a small population, and decreased ability to obtain true formal developmental scores due to the COVID pandemic, this study found more severe HIE had higher HeRO scores. Not all patients had elevated scores, but those who did had elevated scores until 60 hours post warming. Mean scores did not differ between groups at discharge. Further analysis is needed to investigate elevated scores. Our finding of most children with concerns at developmental follow-up shows that HeRO scores may be less sensitive to long-term issues than short term, such as sepsis.
Table 1.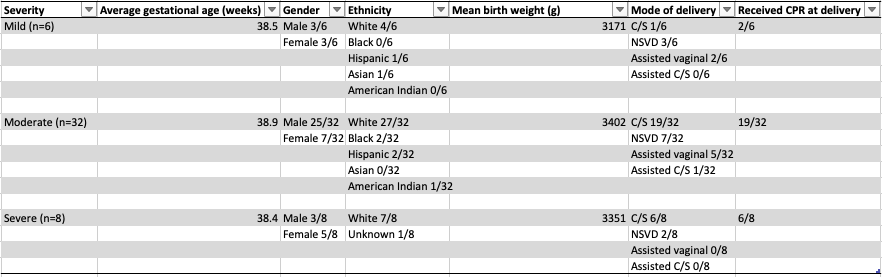 HIE severity, infant demographics, mode of delivery, and CPR performance at delivery
HIE severity, infant demographics, mode of delivery, and CPR performance at delivery
Figure 1.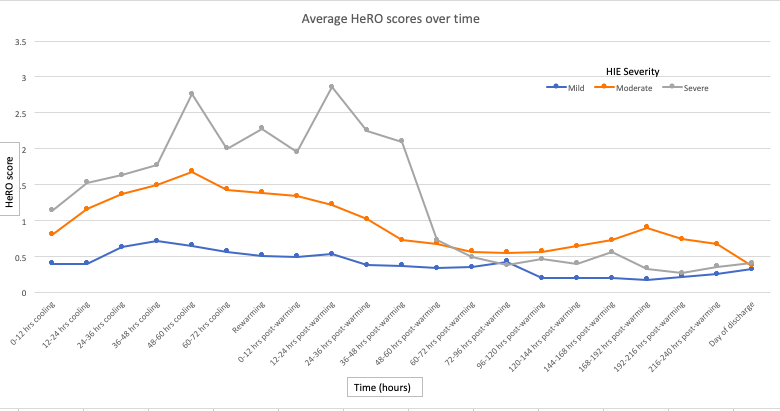 Comparison of mean HeRO score averaged over 12 hour period by HIE severity
Comparison of mean HeRO score averaged over 12 hour period by HIE severity
Objective: To determine baseline HeRO scores, examine influencing factors, and to investigate whether HeRO scores are associated with neurodevelopmental outcome in hypoxic encephalopathy (HIE).
Design/Methods: Retrospective cohort study was performed between May 2014-March 2021, manually reviewing electronic records of infants >35 weeks gestation with HIE undergoing therapeutic hypothermia. We excluded other encephalopathy, any genetic or metabolic disorder, or if cooled at other institutions. Data collection included maternal-child demographics, delivery mode, CPR at delivery, maternal history, infant lab values, HeRO scores (averaged over 12 hour blocks), imaging data, seizures, sepsis, other diagnoses and procedures, and cumulative sedative medications. Developmental outcomes with respect to feeding, communication, cognition, and motor skills were assessed. Descriptive data are summarized and mild-moderate-severe are determined with HIE staging criteria.
Results: 46 infants met criteria. Severity of HIE and demographics are summarized in Table 1. Only 50% had mean score >2 at any time and only 15% had mean score >5. 14/21 with mean HeRO score >2 were also diagnosed with clinical sepsis. 28/32 patients who attended follow up had concerns for abnormal development. Comparison of HIE severity and developmental outcomes is shown in Table 2.Conclusion(s): Although retrospective, a small population, and decreased ability to obtain true formal developmental scores due to the COVID pandemic, this study found more severe HIE had higher HeRO scores. Not all patients had elevated scores, but those who did had elevated scores until 60 hours post warming. Mean scores did not differ between groups at discharge. Further analysis is needed to investigate elevated scores. Our finding of most children with concerns at developmental follow-up shows that HeRO scores may be less sensitive to long-term issues than short term, such as sepsis.
Table 1.
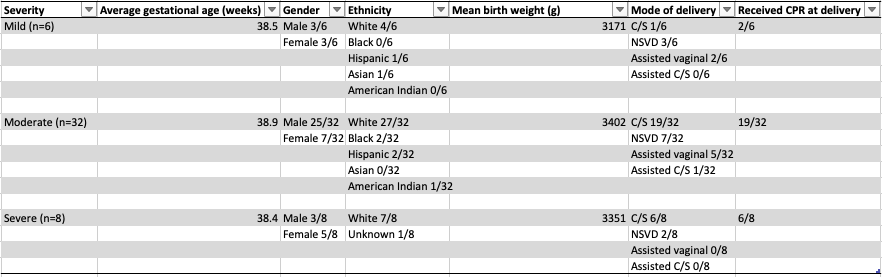 HIE severity, infant demographics, mode of delivery, and CPR performance at delivery
HIE severity, infant demographics, mode of delivery, and CPR performance at deliveryFigure 1.
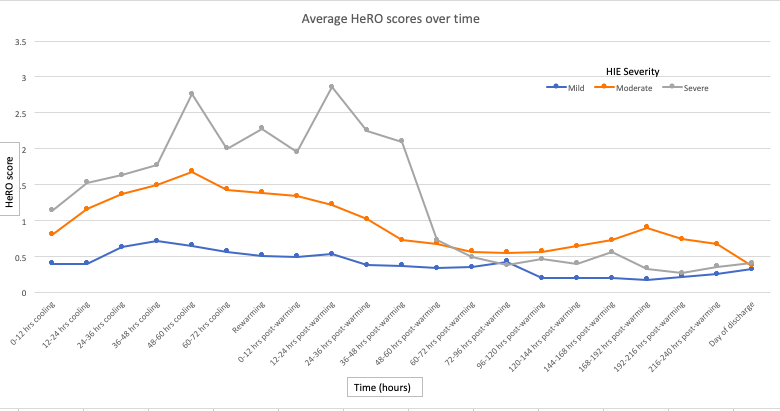 Comparison of mean HeRO score averaged over 12 hour period by HIE severity
Comparison of mean HeRO score averaged over 12 hour period by HIE severity