Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Clinical NOS
325 - How Routine are Routine Vital Signs?
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 325
Publication Number: 325.214
Publication Number: 325.214
Lauren M. McDaniel, Johns Hopkins Children's Center, Baltimore, MD, United States; Shawn Ralston, University of Washington School of Medicine, Seattle, WA, United States

Lauren M. McDaniel, MD
Assistant Professor of Pediatric Hospital Medicine
Johns Hopkins Children's Center
Baltimore, Maryland, United States
Presenting Author(s)
Background: Frequent measurement of vital signs has been associated with disruptions to sleep and increased risk of alarm fatigue. Attitudes and perceptions concerning the necessity of frequent monitoring can impede quality improvement projects in these areas.
Objective: We sought to understand what hospitalists consider standard practice with respect to the measurement of routine vital signs in hospitalized pediatric patients at academic institutions.
Design/Methods: We surveyed pediatric hospital medicine leadership at AAMC-affiliated medical schools on their knowledge and attitudes about routine vital signs in general medicine inpatients. Respondents had the option to provide free text comments at the end of the survey. The total number of hospital beds at each site was collected from the Children’s Hospital Association (CHA) database. The designation of pediatric level I trauma center was collected from the American College of Surgeons Committee on Trauma database. These metrics were utilized as broad proxies for patient volume and acuity of a hospital.
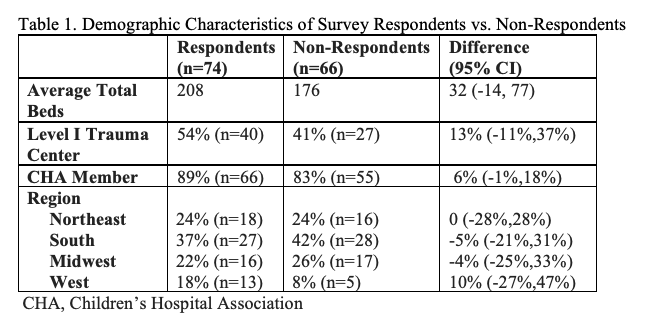
Results: As of 2020, there were 140 unique hospitals affiliated with U.S. medical schools with full AAMC-accreditation. Survey responses were received from 74 hospitalists, representing a 53% response rate. There were no differences in bed size, trauma center designation, CHA membership, or geographic region found between respondents and non-respondents (Table 1). Routine vitals were most commonly characterized as those collected every four hours (78%; 95% CI, 67-87%), though at least one in five hospitalists reported obtaining all or select vital signs (e.g., blood pressure) less frequently (Table 2). Absolute differences in means in bed size, trauma center designation, and CHA membership between hospitalists reporting default vital sign frequency of four hours and those reporting less frequent measurements were not statistically significant. Strategies to decrease vital sign frequency varied (Table 3).Conclusion(s): Our findings suggest that routine vital signs are not a normative concept across all patient populations in pediatrics and that there is some variability in the way hospitalists define routine vitals. This may inform quality improvement leaders attempting to influence attitudes pertaining to necessity of frequent monitoring. The knowledge that other institutions have instituted alternative protocols may be reassuring for those who have concerns about changing routine monitoring frequency. Our report also provides several concrete change ideas for those undertaking quality improvement interventions designed to decrease unnecessary vital signs.
Demographic Characteristics of Survey Respondents vs. Non-Respondents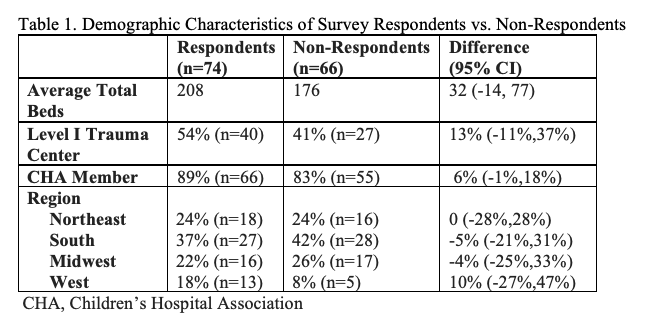
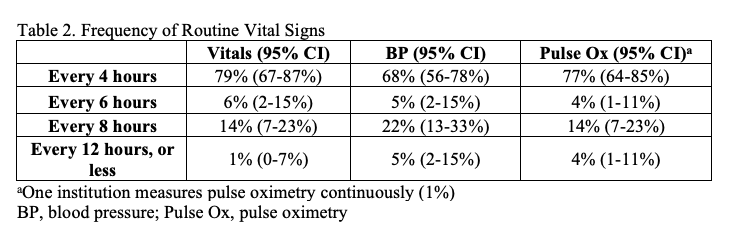
Frequency of Routine Vital Signs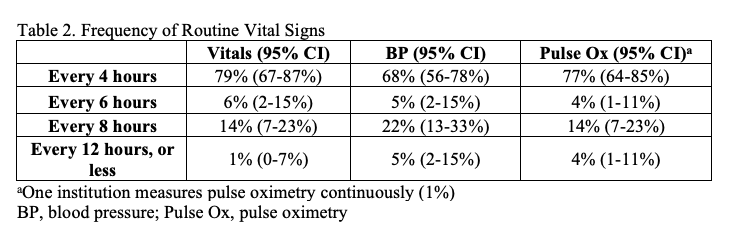
Objective: We sought to understand what hospitalists consider standard practice with respect to the measurement of routine vital signs in hospitalized pediatric patients at academic institutions.
Design/Methods: We surveyed pediatric hospital medicine leadership at AAMC-affiliated medical schools on their knowledge and attitudes about routine vital signs in general medicine inpatients. Respondents had the option to provide free text comments at the end of the survey. The total number of hospital beds at each site was collected from the Children’s Hospital Association (CHA) database. The designation of pediatric level I trauma center was collected from the American College of Surgeons Committee on Trauma database. These metrics were utilized as broad proxies for patient volume and acuity of a hospital.
Results: As of 2020, there were 140 unique hospitals affiliated with U.S. medical schools with full AAMC-accreditation. Survey responses were received from 74 hospitalists, representing a 53% response rate. There were no differences in bed size, trauma center designation, CHA membership, or geographic region found between respondents and non-respondents (Table 1). Routine vitals were most commonly characterized as those collected every four hours (78%; 95% CI, 67-87%), though at least one in five hospitalists reported obtaining all or select vital signs (e.g., blood pressure) less frequently (Table 2). Absolute differences in means in bed size, trauma center designation, and CHA membership between hospitalists reporting default vital sign frequency of four hours and those reporting less frequent measurements were not statistically significant. Strategies to decrease vital sign frequency varied (Table 3).Conclusion(s): Our findings suggest that routine vital signs are not a normative concept across all patient populations in pediatrics and that there is some variability in the way hospitalists define routine vitals. This may inform quality improvement leaders attempting to influence attitudes pertaining to necessity of frequent monitoring. The knowledge that other institutions have instituted alternative protocols may be reassuring for those who have concerns about changing routine monitoring frequency. Our report also provides several concrete change ideas for those undertaking quality improvement interventions designed to decrease unnecessary vital signs.
Demographic Characteristics of Survey Respondents vs. Non-Respondents
Frequency of Routine Vital Signs