Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: COVID-19
285 - Impact of SARS-CoV-2 infection during pregnancy on maternal and neonatal outcomes
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 285
Publication Number: 285.226
Publication Number: 285.226
Manoj Biniwale, USC Keck School of Medicine, Los Angeles, CA, United States; Amy Yeh, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States; Allison Bearden, Keck School of Medicine of the University of Southern California, south pasadena, CA, United States; Olivier Pernet, Keck School of Medicine of the University of Southern California, Los Angeles, CA, United States; Rangasamy Ramanathan, Keck School of Medicine of USC, Los Angeles, CA, United States; Andrea A. Kovacs, USC, Los Angeles, CA, United States

Manoj Biniwale, MD
Associate professor of Pediatrics
USC Keck School of Medicine
Los angeles, California, United States
Presenting Author(s)
Background: Pregnant women are at considerable risk for SARS-CoV-2 infection with adverse maternal and neonatal outcomes. Mother-to-child-transmission can occur, in-utero, perinatally or postnatally with significant complications in the newborn.
Objective: To describe maternal and neonatal outcomes among those with and without SARS-CoV-2 infection from 2 urban hospitals.
Design/Methods: Retrospective review of data from two centers with level III NICUs from May 2020 through October 2021. Pregnant women were screened at delivery with PCR and newborns at 24 and 48 hours if PCR+ in mothers.
Results: Among the 2895 pregnant women, 269 (9.3%) were PCR+. Majority were Hispanic (96%) and asymptomatic (89.4%); 7.6% were symptomatic for 0-7 days prior to delivery, and 2.0% required hospitalization for COVID-19 with ventilation support. SARS-CoV-2 exposed infants were live singletons births; 71% were born by vaginal delivery and 29% by C-section. Mean gestational age was 38 weeks; 35 infants (13%) were preterm. Mean birthweight was 3164 grams; 26 infants (9.7%) were low birthweight (LBW). Fifteen infants needed resuscitation with noninvasive ventilation and 3 infants needed intubation in the delivery room. All but 2 infants had PCR tests at 24 hours and 48 hours if still hospitalized and 7 (2.5%) were PCR+: 6 at 24 hours and 1 at 48 hours. Five of the 7 infants were born at term and 2 preterm (29 and 36 weeks). Two of the infants were born to symptomatic COVID-19 women prior to delivery. Among PCR+ 7 infants, 5 developed respiratory distress and 2 required mechanical ventilation. Two infants were treated with remdesivir, dexamethasone and enoxaparin. All infants recovered and went home. PCR- 151/262 infants developed respiratory or other symptoms (Figure 1). Data on 181 infants was analyzed for outcomes in PCR+ infants. Significant outcomes included increased respiratory support, low WBC count and increased length of stay. (Table 1) Overall survival for infants born to mothers with COVID-19 diagnosis was 99%. Two infants died of prematurity related complications and tested negative for SARS-CoV-2.Conclusion(s): SARS-CoV-2 infection was present at delivery in almost 10% of women and 2.5% of their infants. Although majority of women were asymptomatic at the time of delivery, there was significant morbidity among newborns including prematurity, LBW and respiratory distress even in PCR-newborns. Two PCR+ infants were symptomatic requiring mechanical ventilation and antiviral medication. These data emphasize the need of vaccination in pregnant women and close monitoring of mother-infant dyad if infected.
Table 1: Maternal and neonatal characteristics#.jpg) *Median (25th-75th centile)
*Median (25th-75th centile)
#Data available for 181 mothers and infants
CPAP continuous positive airway pressure
WBC white blood cell
AST aspartate aminotransferase
ALT alanine aminotransferase
Figure 1: Study Flow Diagram showing distribution of mothers and infants at 2 centers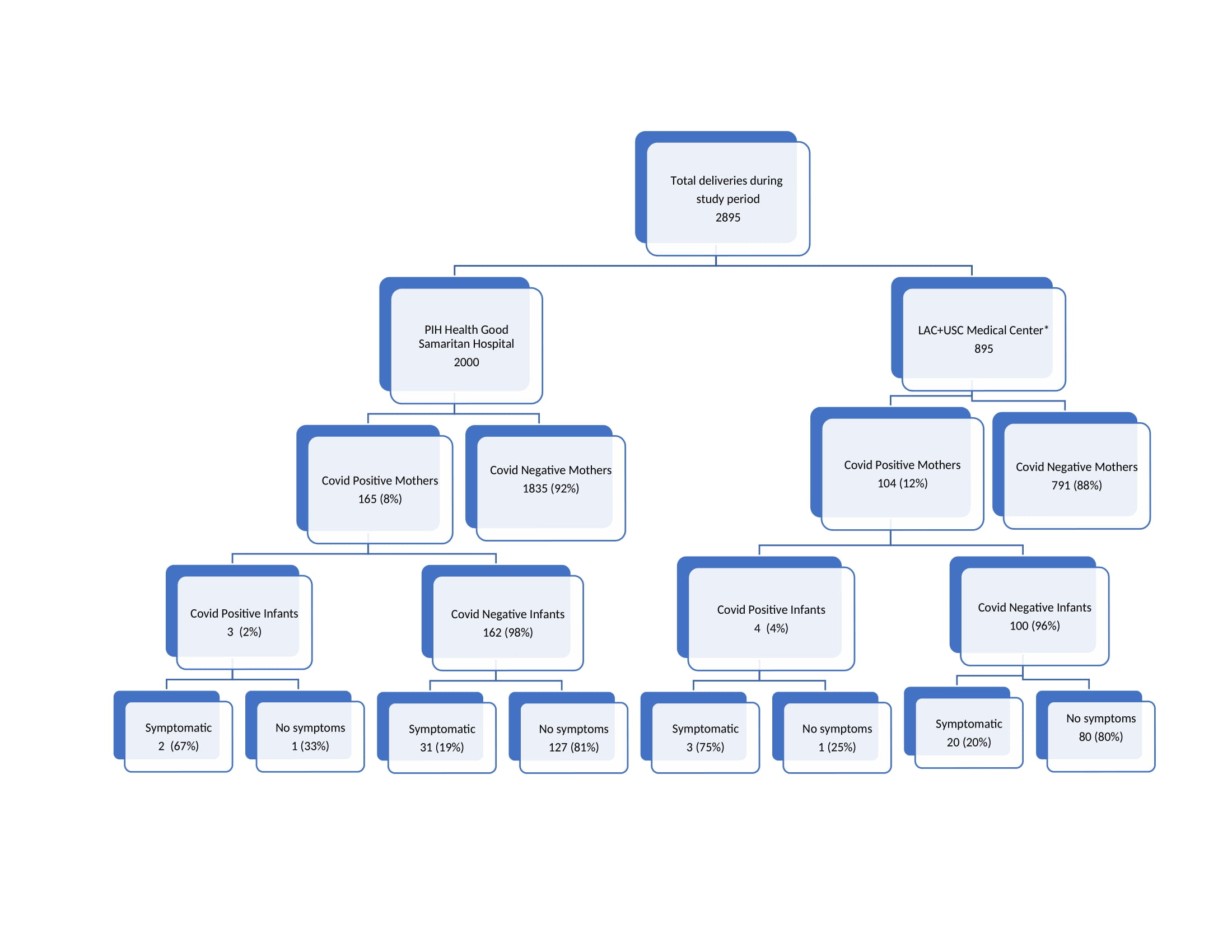 *incomplete data
*incomplete data
Objective: To describe maternal and neonatal outcomes among those with and without SARS-CoV-2 infection from 2 urban hospitals.
Design/Methods: Retrospective review of data from two centers with level III NICUs from May 2020 through October 2021. Pregnant women were screened at delivery with PCR and newborns at 24 and 48 hours if PCR+ in mothers.
Results: Among the 2895 pregnant women, 269 (9.3%) were PCR+. Majority were Hispanic (96%) and asymptomatic (89.4%); 7.6% were symptomatic for 0-7 days prior to delivery, and 2.0% required hospitalization for COVID-19 with ventilation support. SARS-CoV-2 exposed infants were live singletons births; 71% were born by vaginal delivery and 29% by C-section. Mean gestational age was 38 weeks; 35 infants (13%) were preterm. Mean birthweight was 3164 grams; 26 infants (9.7%) were low birthweight (LBW). Fifteen infants needed resuscitation with noninvasive ventilation and 3 infants needed intubation in the delivery room. All but 2 infants had PCR tests at 24 hours and 48 hours if still hospitalized and 7 (2.5%) were PCR+: 6 at 24 hours and 1 at 48 hours. Five of the 7 infants were born at term and 2 preterm (29 and 36 weeks). Two of the infants were born to symptomatic COVID-19 women prior to delivery. Among PCR+ 7 infants, 5 developed respiratory distress and 2 required mechanical ventilation. Two infants were treated with remdesivir, dexamethasone and enoxaparin. All infants recovered and went home. PCR- 151/262 infants developed respiratory or other symptoms (Figure 1). Data on 181 infants was analyzed for outcomes in PCR+ infants. Significant outcomes included increased respiratory support, low WBC count and increased length of stay. (Table 1) Overall survival for infants born to mothers with COVID-19 diagnosis was 99%. Two infants died of prematurity related complications and tested negative for SARS-CoV-2.Conclusion(s): SARS-CoV-2 infection was present at delivery in almost 10% of women and 2.5% of their infants. Although majority of women were asymptomatic at the time of delivery, there was significant morbidity among newborns including prematurity, LBW and respiratory distress even in PCR-newborns. Two PCR+ infants were symptomatic requiring mechanical ventilation and antiviral medication. These data emphasize the need of vaccination in pregnant women and close monitoring of mother-infant dyad if infected.
Table 1: Maternal and neonatal characteristics#
.jpg) *Median (25th-75th centile)
*Median (25th-75th centile) #Data available for 181 mothers and infants
CPAP continuous positive airway pressure
WBC white blood cell
AST aspartate aminotransferase
ALT alanine aminotransferase
Figure 1: Study Flow Diagram showing distribution of mothers and infants at 2 centers
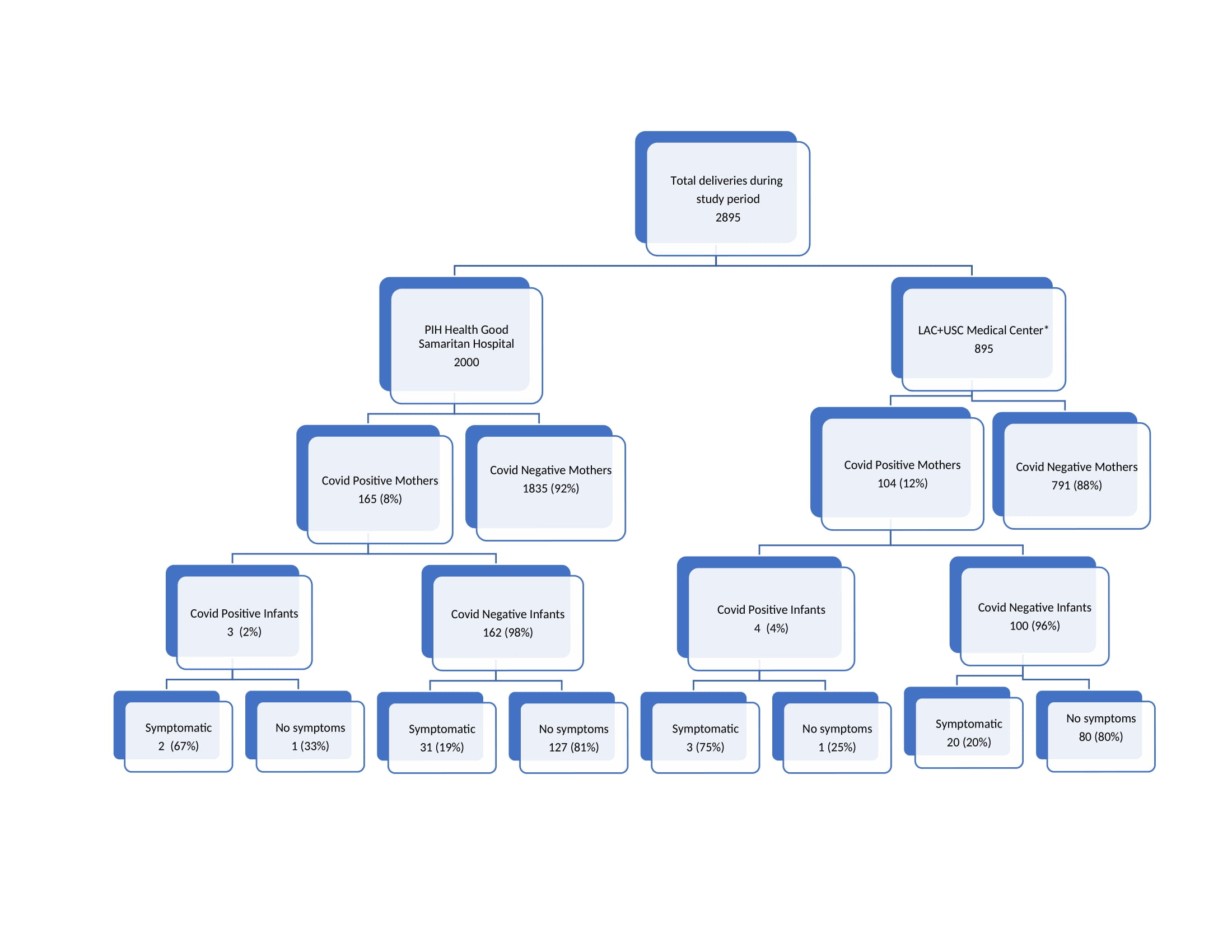 *incomplete data
*incomplete data