Critical Care
Category: Abstract Submission
Critical Care II
23 - Inhaled Epoprostenol Improves Right Ventricle Pressure in Critically Ill Children with Pulmonary Hypertension
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 23
Publication Number: 23.201
Publication Number: 23.201
Disi Chen, Golisano Children's Hospital at The University of Rochester Medical Center, Rochester, NY, United States; Rajiv Devanagondi, Golisano Children's Hospital at The University of Rochester Medical Center, Rochester, NY, United States

Disi Chen, MD
Resident
Golisano Children's Hospital at The University of Rochester Medical Center
Rochester, New York, United States
Presenting Author(s)
Background: Pulmonary hypertension (PH) is associated with 5-10% mortality due to congestive heart failure or respiratory failure in children. While small studies have shown improved oxygenation in children treated with inhaled epoprostenol (iPGI2), studies describing oxygenation and echocardiographic markers of PH are lacking.
Objective: Describe the effect of iPGI2on oxygenation and echocardiographic markers of PH in a retrospective cohort study.
Design/Methods: All patients between 3 weeks and 18 years old diagnosed with PH and treated with iPGI2 in the intensive care units at our center from 1/1/2015 to 10/31/2020 were included. Patients treated with another prostanoid or ECMO were excluded. Categorical variables were described as n (%) and continuous variables as mean (range). SpO2, PaO2 and FiO2 were compared at baseline (prior to iPGI2), 2h after and 12h after iPGI2initiation using repeated measure ANOVA. Echocardiographic data pre and post iPGI2 initiation were compared using the paired t-test and Wilson’s test. Outcome variables with highly skewed distributions were log transformed. P < 0.05 was considered statistically significant.
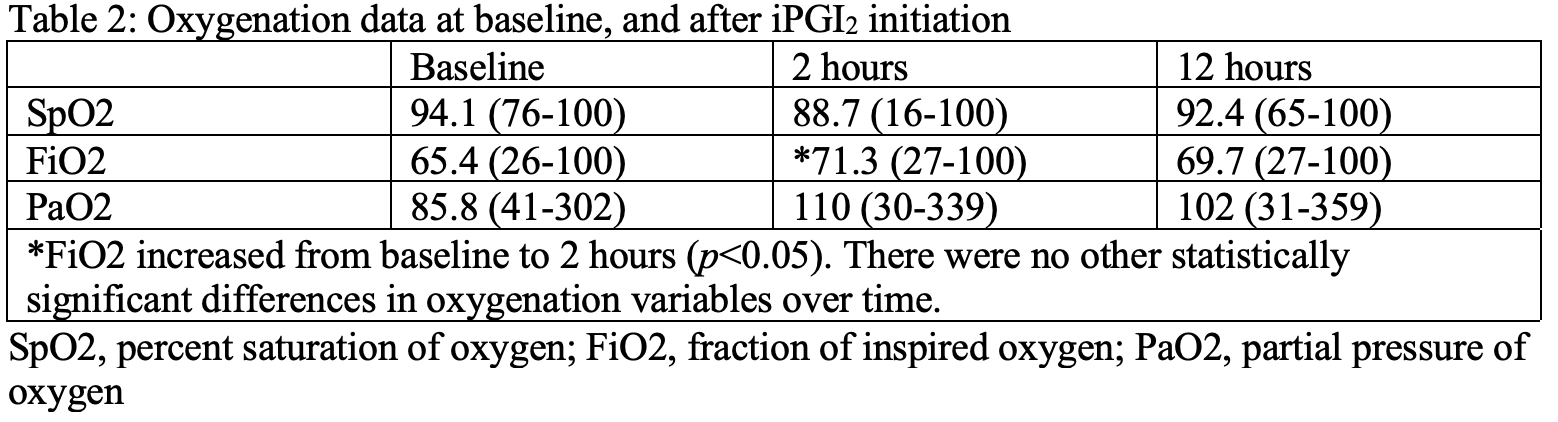
Results: 28 patients were treated with iPGI2 at mean age 28 (3-78) weeks. 11 (39%) were premature and 22 (79%) had congenital heart disease. The mean iPGI2 dose was 142 (25-200) ng/kg/min and duration of therapy 41.9 (1-148) hours. There was iPGI2 significant reduction in FiO2, or increase in SpO2 or PaO2 after iPGI2 initiation (Table 2). There was a significant reduction in tricuspid regurgitation peak gradient from (76 [33-105] to 55 [19-92] mmHg, p < 0.05) by echocardiogram. There was a trend towards improvement in echocardiographic markers of right ventricle (RV) function after iPGI2 initiation. 4 patients (16%) had improved RV size, 3 (12%) had improved RV hypertrophy, 6 (24%) had improved RV function, 8 (32%) had improved tricuspid valve regurgitation, and 6 (24%) had improved pulmonary valve regurgitation after initiation of iPGI2. In this critically ill population, mortality was 25%.Conclusion(s): iPGI2 treatment leads to significant reductions in tricuspid regurgitation peak gradient indicating improvements in RV pressure, despite the absence of improvement in clinical markers of oxygenation. A prospective trial may better define the effectiveness of iPGI2 and relationship between right ventricle pressure and oxygenation in children with PH and hypoxemic respiratory failure.
Table 1: Demographics.png)
Table 2: Oxygenation data at baseline, and after iPGI2 initiation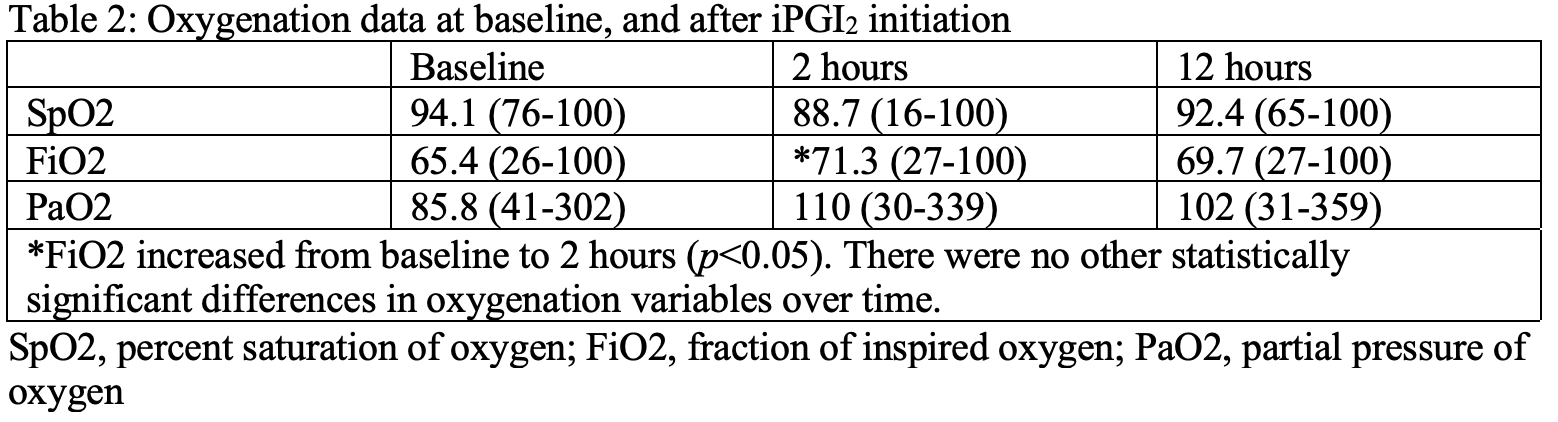
Objective: Describe the effect of iPGI2on oxygenation and echocardiographic markers of PH in a retrospective cohort study.
Design/Methods: All patients between 3 weeks and 18 years old diagnosed with PH and treated with iPGI2 in the intensive care units at our center from 1/1/2015 to 10/31/2020 were included. Patients treated with another prostanoid or ECMO were excluded. Categorical variables were described as n (%) and continuous variables as mean (range). SpO2, PaO2 and FiO2 were compared at baseline (prior to iPGI2), 2h after and 12h after iPGI2initiation using repeated measure ANOVA. Echocardiographic data pre and post iPGI2 initiation were compared using the paired t-test and Wilson’s test. Outcome variables with highly skewed distributions were log transformed. P < 0.05 was considered statistically significant.
Results: 28 patients were treated with iPGI2 at mean age 28 (3-78) weeks. 11 (39%) were premature and 22 (79%) had congenital heart disease. The mean iPGI2 dose was 142 (25-200) ng/kg/min and duration of therapy 41.9 (1-148) hours. There was iPGI2 significant reduction in FiO2, or increase in SpO2 or PaO2 after iPGI2 initiation (Table 2). There was a significant reduction in tricuspid regurgitation peak gradient from (76 [33-105] to 55 [19-92] mmHg, p < 0.05) by echocardiogram. There was a trend towards improvement in echocardiographic markers of right ventricle (RV) function after iPGI2 initiation. 4 patients (16%) had improved RV size, 3 (12%) had improved RV hypertrophy, 6 (24%) had improved RV function, 8 (32%) had improved tricuspid valve regurgitation, and 6 (24%) had improved pulmonary valve regurgitation after initiation of iPGI2. In this critically ill population, mortality was 25%.Conclusion(s): iPGI2 treatment leads to significant reductions in tricuspid regurgitation peak gradient indicating improvements in RV pressure, despite the absence of improvement in clinical markers of oxygenation. A prospective trial may better define the effectiveness of iPGI2 and relationship between right ventricle pressure and oxygenation in children with PH and hypoxemic respiratory failure.
Table 1: Demographics
.png)
Table 2: Oxygenation data at baseline, and after iPGI2 initiation