Neonatal/Infant Resuscitation
Category: Abstract Submission
Neonatal/Infant Resuscitation II
484 - Neonatal Resuscitation with Laryngeal Mask Airway (LMA) versus Neonatal Facemask among Unskilled Providers
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 484
Publication Number: 484.231
Publication Number: 484.231
Nithya Sivakumar, University of California, Davis, School of Medicine, Fremont, CA, United States; Shoshana Newman-Lindsay, University of California Davis Children's Hospital, Sacramento, CA, United States; Deepika Sankaran, University of California Davis Children's Hospital, Sacramento, CA, United States; Satyan Lakshminrusimha, University of California Davis Children's Hospital, Sacramento, CA, United States; Lee Donohue, University of California, Davis, School of Medicine, Sacramento, CA, United States
- NS
Nithya Sivakumar, BA, MBE (she/her/hers)
Medical Student
UC Davis Children's Hospital
Sacramento, California, United States
Presenting Author(s)
Background:
Effective positive pressure ventilation (PPV) is the single most important component of neonatal resuscitation. The Neonatal Resuscitation Program (NRP) recommends initiating PPV using facemask, and if ineffective despite corrective steps, switching to endotracheal intubation (ETT) or LMA. Pejovic et al (NEJM, 2020) have demonstrated that LMA is safe in the hands of midwives but not superior to facemask in reducing neonatal death or moderate/severe HIE. Time to effective ventilation during simulation by unskilled providers may provide evidence as to whether LMA is superior to facemask as first line ventilation interface in neonatal resuscitation.
Objective: To compare time to effective ventilation and perceived confidence of pre-clinical medical students (MS) in performing adequate ventilation on a neonatal manikin with LMA and facemask.
Design/Methods: Thirty-two pre-clinical MS were recruited and randomized to learning and performing ventilation with either the LMA (Teleflex size 1) or facemask with T-piece resuscitator on a neonatal manikin (Gaumard). Time to effective ventilation was defined as time to ten consecutive breaths reaching preset goal tidal volume in the Gaumard software. Tidal volume was measured by breath-by-breath analysis to assess adequacy and consistency of PPV in 10 consecutive breaths. Perceived confidence was measured by pre- and post-surveys administered prior to and after learning and demonstrating the intervention. The surveys administered utilized a 5-point Likert scale, where 1= “not at all confident” and 5= “very confident”.
Results: Sixteen MS each were randomized to the LMA facemask groups respectively. Average time to achieve effective ventilation was shorter with facemask compared to LMA amongst pre-clinical MS (81 seconds vs 171 seconds, p< 0.01). Figure 1 presents a screenshot of ten consecutive breaths that met the target tidal volume. Pre-clinical MS reported higher perceived confidence post-intervention with use of facemask when compared to use of LMA (4.6 vs 4, p=0.03). No difference was noted in perceived confidence in other parameters.Conclusion(s): Pre-clinical MS demonstrated a shorter time to effective ventilation and reported higher confidence scores after learning and demonstrating PPV using the facemask when compared to LMA. Further research is needed to determine if optimization of learning interventions or device improvements will influence unskilled providers’ confidence or performance with an LMA versus facemask.
CV for Nithya SivakumarCV.pdf
Figure 1: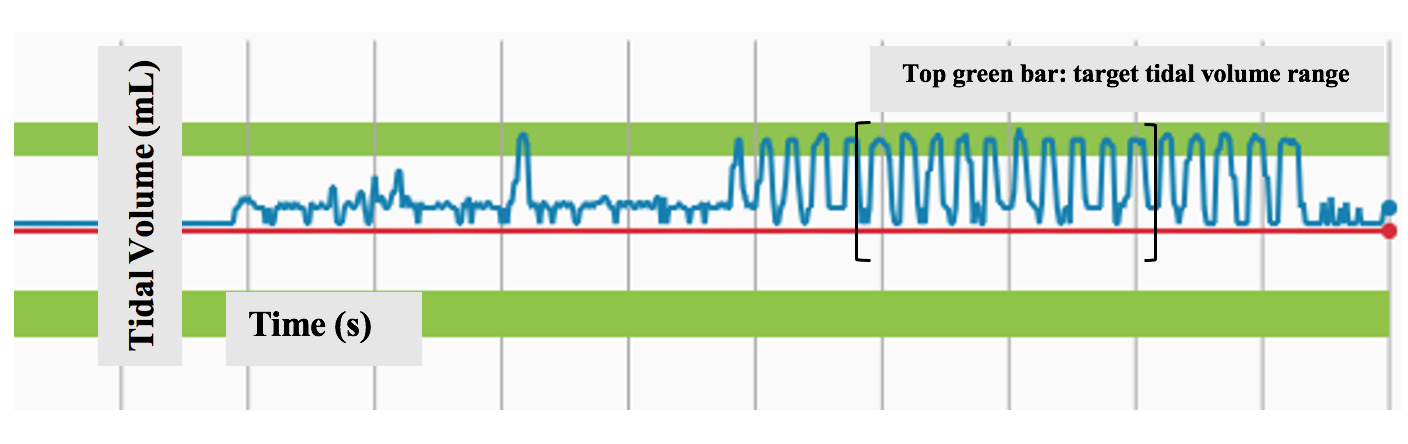 Screenshot of Gaumard software depicting consecutive breaths that meet target tidal volumes. Green bar indicates target tidal volume range, and brackets show ten consecutive breaths of adequate tidal volume.
Screenshot of Gaumard software depicting consecutive breaths that meet target tidal volumes. Green bar indicates target tidal volume range, and brackets show ten consecutive breaths of adequate tidal volume.
Effective positive pressure ventilation (PPV) is the single most important component of neonatal resuscitation. The Neonatal Resuscitation Program (NRP) recommends initiating PPV using facemask, and if ineffective despite corrective steps, switching to endotracheal intubation (ETT) or LMA. Pejovic et al (NEJM, 2020) have demonstrated that LMA is safe in the hands of midwives but not superior to facemask in reducing neonatal death or moderate/severe HIE. Time to effective ventilation during simulation by unskilled providers may provide evidence as to whether LMA is superior to facemask as first line ventilation interface in neonatal resuscitation.
Objective: To compare time to effective ventilation and perceived confidence of pre-clinical medical students (MS) in performing adequate ventilation on a neonatal manikin with LMA and facemask.
Design/Methods: Thirty-two pre-clinical MS were recruited and randomized to learning and performing ventilation with either the LMA (Teleflex size 1) or facemask with T-piece resuscitator on a neonatal manikin (Gaumard). Time to effective ventilation was defined as time to ten consecutive breaths reaching preset goal tidal volume in the Gaumard software. Tidal volume was measured by breath-by-breath analysis to assess adequacy and consistency of PPV in 10 consecutive breaths. Perceived confidence was measured by pre- and post-surveys administered prior to and after learning and demonstrating the intervention. The surveys administered utilized a 5-point Likert scale, where 1= “not at all confident” and 5= “very confident”.
Results: Sixteen MS each were randomized to the LMA facemask groups respectively. Average time to achieve effective ventilation was shorter with facemask compared to LMA amongst pre-clinical MS (81 seconds vs 171 seconds, p< 0.01). Figure 1 presents a screenshot of ten consecutive breaths that met the target tidal volume. Pre-clinical MS reported higher perceived confidence post-intervention with use of facemask when compared to use of LMA (4.6 vs 4, p=0.03). No difference was noted in perceived confidence in other parameters.Conclusion(s): Pre-clinical MS demonstrated a shorter time to effective ventilation and reported higher confidence scores after learning and demonstrating PPV using the facemask when compared to LMA. Further research is needed to determine if optimization of learning interventions or device improvements will influence unskilled providers’ confidence or performance with an LMA versus facemask.
CV for Nithya SivakumarCV.pdf
Figure 1:
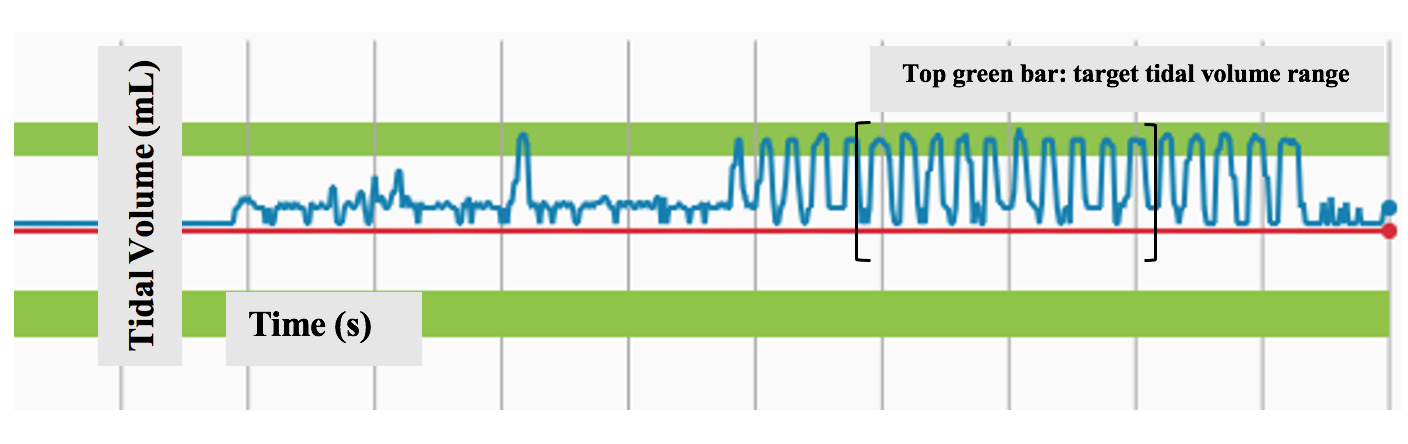 Screenshot of Gaumard software depicting consecutive breaths that meet target tidal volumes. Green bar indicates target tidal volume range, and brackets show ten consecutive breaths of adequate tidal volume.
Screenshot of Gaumard software depicting consecutive breaths that meet target tidal volumes. Green bar indicates target tidal volume range, and brackets show ten consecutive breaths of adequate tidal volume.