Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up II
258 - Prospective associations of sleep with diet and adiposity among toddlers born preterm
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 258
Publication Number: 258.224
Publication Number: 258.224
Samrawit F. Yisahak, Nationwide Children’s Hospital, Columbus, OH, United States; Kelly M. Boone, Nationwide Children's Hospital, Columbus, OH, United States; Sarah Keim, Nationwide Children’s Hospital / Ohio State University, Columbus, OH, United States
- SY
Samrawit F. Yisahak, PhD (she/her/hers)
Research Scientist
Nationwide Children's Hospital
Columbus, Ohio, United States
Presenting Author(s)
Background: Suboptimal sleep is a risk factor for poor diet and obesity. However, associations of sleep with these outcomes are understudied during toddlerhood when lifestyle habits and taste preferences establish. Prior studies focused on total sleep duration, though day and nighttime sleep could have different associations due to circadian regulation of appetite/metabolism. Further, studies mostly focused on short sleep, rather than examining the entire range of sleep duration.
Objective: In a secondary analysis of a randomized controlled trial of toddlers born preterm, we examined prospective associations of sleep duration and timing with dietary and anthropometric measures.
Design/Methods: Children born at < 35 weeks’ gestation were randomized at corrected age 10-17 months to placebo or fatty acid supplementation for 180 days. Caregivers reported toddlers’ sleep habits at baseline using the Brief Infant Sleep Questionnaire. We defined short and long sleep per American Academy of Sleep Medicine recommendations ( < 12 hrs./day and >16 hrs./day for children < 1 year, and < 11 hrs./day and >14 hrs./day for children 1-2 years, respectively). After 180 days, caregivers reported the child’s past month diet in a food frequency questionnaire, and child’s anthropometry was measured using standardized protocols. We used World Health Organization growth standards to calculate weight-for-height, triceps skinfold, and subscapular skinfold z-scores. We used linear and logistic regression to assess associations with outcomes in 284 toddlers with sleep and plausible dietary data. Covariates, measured at baseline, were child’s sex, race, ethnicity, pre-maturity corrected age (in months), birthweight, breastfeeding history, as well as maternal education, marital status, annual household income, and treatment arm.
Results: Nearly 30% of toddlers had long or short sleep (Table 1). Sleep duration and timing were not associated with total energy intake (Table 2) or measures of adiposity (Table 3). However, more nighttime sleep (per hour) was associated with higher intake of fiber (beta= 0.87 grams (95% CI: 0.20, 1.54)). Shorter than recommended sleep was associated with lower fiber intake (beta= -3.37 grams (95% CI: -6.11, -0.63)) (Table 2). Conclusion(s): Longer nighttime, but not daytime sleep, was associated with higher intake of fiber suggesting that sleep timing maybe important for diet quality. Contrary to our expectations, higher than recommended sleep showed no associations with unfavorable diet or adiposity.
Table 1: Baseline characteristics of toddlers born preterm by sleep duration, Omega Tots trial (2012-2017, n=284, Columbus, Ohio)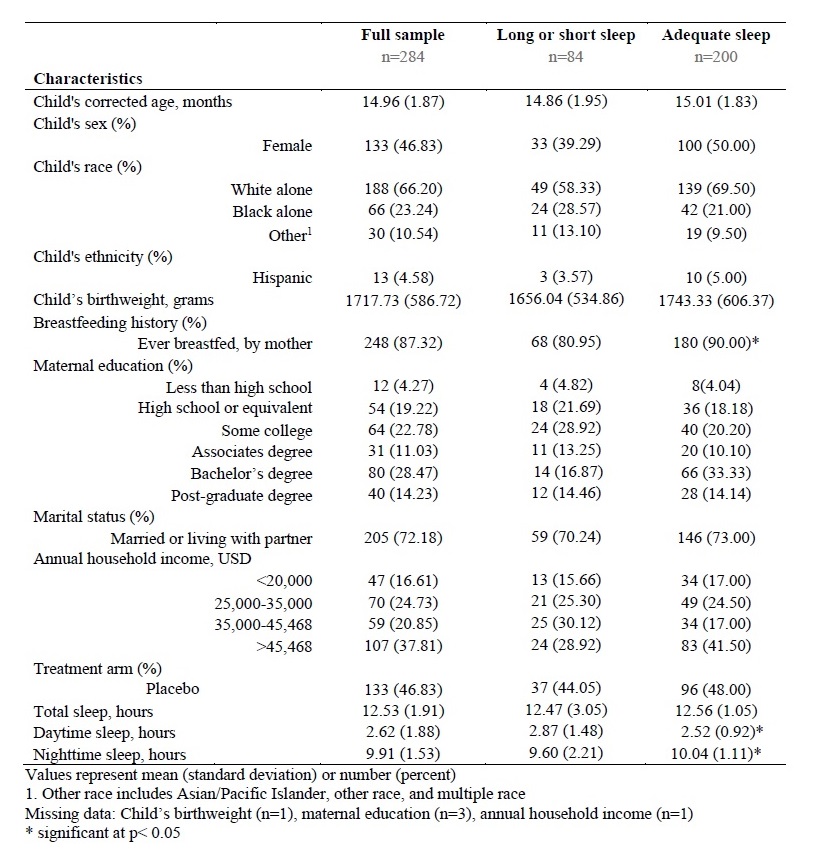
Table 2: Prospective associations of sleep with dietary components, Omega Tots trial (2012-2017, n=284, Columbus, Ohio).jpg)
Objective: In a secondary analysis of a randomized controlled trial of toddlers born preterm, we examined prospective associations of sleep duration and timing with dietary and anthropometric measures.
Design/Methods: Children born at < 35 weeks’ gestation were randomized at corrected age 10-17 months to placebo or fatty acid supplementation for 180 days. Caregivers reported toddlers’ sleep habits at baseline using the Brief Infant Sleep Questionnaire. We defined short and long sleep per American Academy of Sleep Medicine recommendations ( < 12 hrs./day and >16 hrs./day for children < 1 year, and < 11 hrs./day and >14 hrs./day for children 1-2 years, respectively). After 180 days, caregivers reported the child’s past month diet in a food frequency questionnaire, and child’s anthropometry was measured using standardized protocols. We used World Health Organization growth standards to calculate weight-for-height, triceps skinfold, and subscapular skinfold z-scores. We used linear and logistic regression to assess associations with outcomes in 284 toddlers with sleep and plausible dietary data. Covariates, measured at baseline, were child’s sex, race, ethnicity, pre-maturity corrected age (in months), birthweight, breastfeeding history, as well as maternal education, marital status, annual household income, and treatment arm.
Results: Nearly 30% of toddlers had long or short sleep (Table 1). Sleep duration and timing were not associated with total energy intake (Table 2) or measures of adiposity (Table 3). However, more nighttime sleep (per hour) was associated with higher intake of fiber (beta= 0.87 grams (95% CI: 0.20, 1.54)). Shorter than recommended sleep was associated with lower fiber intake (beta= -3.37 grams (95% CI: -6.11, -0.63)) (Table 2). Conclusion(s): Longer nighttime, but not daytime sleep, was associated with higher intake of fiber suggesting that sleep timing maybe important for diet quality. Contrary to our expectations, higher than recommended sleep showed no associations with unfavorable diet or adiposity.
Table 1: Baseline characteristics of toddlers born preterm by sleep duration, Omega Tots trial (2012-2017, n=284, Columbus, Ohio)
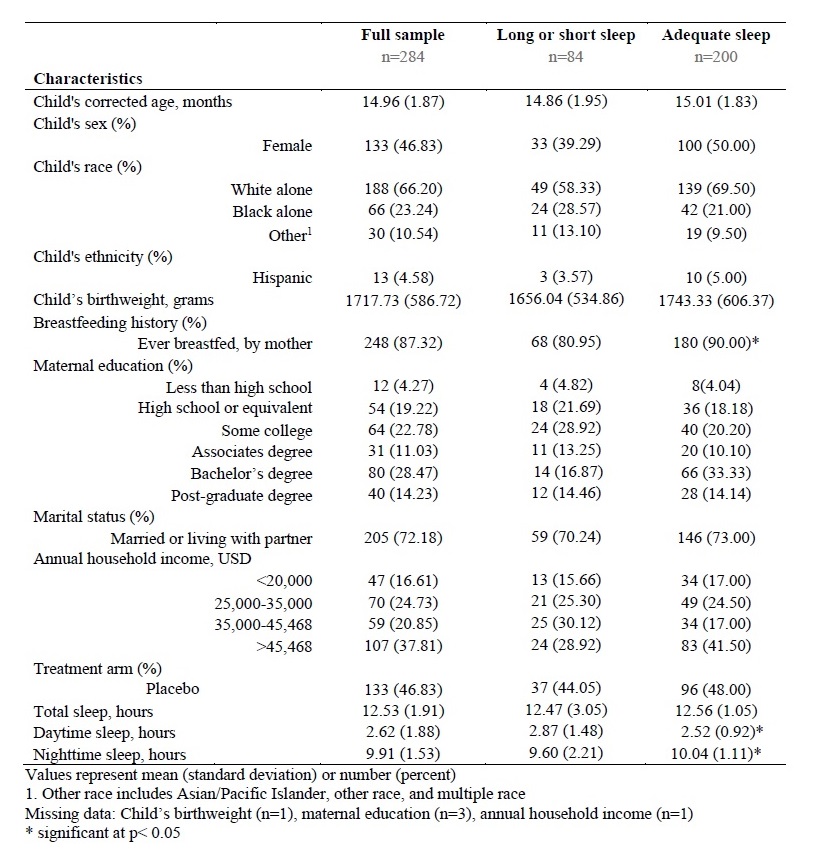
Table 2: Prospective associations of sleep with dietary components, Omega Tots trial (2012-2017, n=284, Columbus, Ohio)
.jpg)
