General Pediatrics: All Areas
Category: Abstract Submission
General Pediatrics II
608 - Reduction in Hospitalizations and Changing Age Demographics of Respiratory Syncytial Virus Disease during the COVID-19 Pandemic
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 608
Publication Number: 608.209
Publication Number: 608.209
Sidney Zven, Walter Reed National Military Medical Center, Annandale, VA, United States; Madeline Dorr, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, McLean, VA, United States; Allison M. Malloy, USUHS, Bethesda, MD, United States; Cade M. Nylund, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Apryl Susi, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Ian S. Sorensen, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Maxwell Ebert, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Jayasree Krishnamurthy, Uniformed Services University of the Health Sciences F. Edward Hebert School of Medicine, Bethesda, MD, United States; Elizabeth Hisle-Gorman, Uniformed Services University, Bethesda, MD, United States

Sidney Zven, MD
Pediatric Resident
Walter Reed National Military Medical Center Department of Pediatrics
Annandale, Virginia, United States
Presenting Author(s)
Background: Globally, respiratory syncytial virus (RSV) is the most common cause of lower respiratory tract infections in young children. Several international studies have shown reduced infections requiring hospitalization, a delayed peak of infection, and changing age demographics associated with COVID-19 pandemic precautions.
Objective: To define the frequency, and age at RSV hospitalization prior to and during the COVID-19 pandemic in children age < 6 years receiving care.
Design/Methods: A retrospective cross-sectional study using Military Health System data examined RSV hospitalizations in children < 6 years old during the first year of the COVID-19 pandemic (March 2020-Feb 2021) as compared to the year prior (March 2019-Feb 2020). RSV was identified by ICD-10 codes. Children were stratified by age: 0, 1, and 2-5 years. Poisson regression analysis compared hospitalization rates by time period.
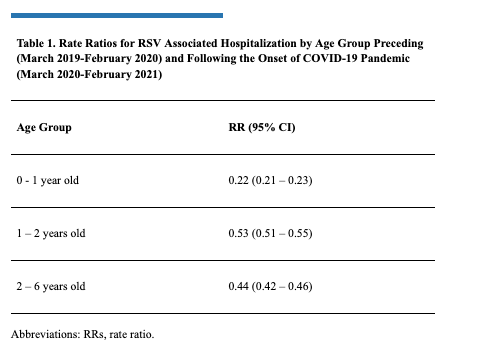
Results: An average of 66,0437 children were included each month. In the pre-COVID-19 period RSV hospitalizations peaked in December 2019 for all ages; per 100,000 children: 2,670 (0), 1,492 (1), and 307 (2-5) were admitted for RSV. In Dec 2020 admissions dropped to 68 (0), 280 (1) and 42 (2-5) per 100,000 children (Figure 1). The COVID-19 period was associated with a 78% decreased rate of hospitalizations for age 0 (p < 0.001), a 47% for age 1 (p < 0.001) and 56% decreased rate for ages 2–5 (p < 0.001; Table 1).Conclusion(s): Results indicate a pronounced decrease in RSV hospitalizations during COVID-19, as compared to the previous year in all age groups. Despite decreases across all age groups, age 1 had a less pronounced drop (Table 1), with an uptick in September 2020, earlier than expected (Figure 1). Results may be related to decreased exposure to RSV for age 0, changes in childcare use patterns, and/or changes in nursing, which is protective. As COVID-19 related precautions are phased out, severe RSV requiring hospitalization may be increased in older children and during atypical seasons. Practitioners should consider testing for RSV in older children and consider the effectiveness of COVID-19 era precautions to prevent respiratory viral diseases other than COVID-19 in infants.
Sidney Zven - CVZven_Sidney_CV.pdf
Table 1. Rate Ratios for RSV Associated Hospitalization by Age Group Preceding (March 2019-February 2020) and Following the Onset of COVID-19 Pandemic (March 2020-February 2021)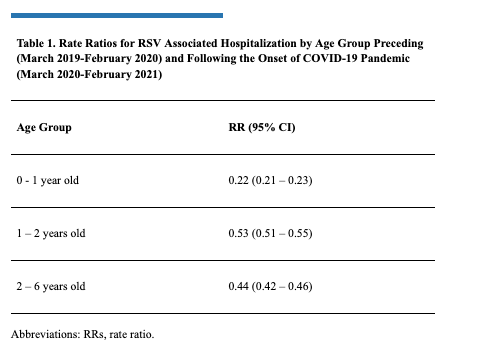
Objective: To define the frequency, and age at RSV hospitalization prior to and during the COVID-19 pandemic in children age < 6 years receiving care.
Design/Methods: A retrospective cross-sectional study using Military Health System data examined RSV hospitalizations in children < 6 years old during the first year of the COVID-19 pandemic (March 2020-Feb 2021) as compared to the year prior (March 2019-Feb 2020). RSV was identified by ICD-10 codes. Children were stratified by age: 0, 1, and 2-5 years. Poisson regression analysis compared hospitalization rates by time period.
Results: An average of 66,0437 children were included each month. In the pre-COVID-19 period RSV hospitalizations peaked in December 2019 for all ages; per 100,000 children: 2,670 (0), 1,492 (1), and 307 (2-5) were admitted for RSV. In Dec 2020 admissions dropped to 68 (0), 280 (1) and 42 (2-5) per 100,000 children (Figure 1). The COVID-19 period was associated with a 78% decreased rate of hospitalizations for age 0 (p < 0.001), a 47% for age 1 (p < 0.001) and 56% decreased rate for ages 2–5 (p < 0.001; Table 1).Conclusion(s): Results indicate a pronounced decrease in RSV hospitalizations during COVID-19, as compared to the previous year in all age groups. Despite decreases across all age groups, age 1 had a less pronounced drop (Table 1), with an uptick in September 2020, earlier than expected (Figure 1). Results may be related to decreased exposure to RSV for age 0, changes in childcare use patterns, and/or changes in nursing, which is protective. As COVID-19 related precautions are phased out, severe RSV requiring hospitalization may be increased in older children and during atypical seasons. Practitioners should consider testing for RSV in older children and consider the effectiveness of COVID-19 era precautions to prevent respiratory viral diseases other than COVID-19 in infants.
Sidney Zven - CVZven_Sidney_CV.pdf
Table 1. Rate Ratios for RSV Associated Hospitalization by Age Group Preceding (March 2019-February 2020) and Following the Onset of COVID-19 Pandemic (March 2020-February 2021)