General Pediatrics: All Areas
Category: Abstract Submission
General Pediatrics II
610 - Respiratory Syncytial Virus Infection and Risk of Apnea in Full Term Healthy Infants: Apprehension Alone or Justified Hospitalization?
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 610
Dyana Picache, The Children’s Medical Center at NYU Winthrop Hospital, Upper Saddle River, NJ, United States; Diana Kogan, The Children’s Medical Center at NYU Winthrop Hospital, Mineola, NY, United States; Asif Noor, The Children’s Medical Center at NYU Winthrop Hospital, Mineola, NY, United States; Jill A. Leavens-Maurer, New York University Long Island School of Medicine, Mineola, NY, United States; Theresa Fiorito, The Children’s Medical Center at NYU Winthrop Hospital, Mineola, NY, United States; Leonard R. Krilov, The Children’s Medical Center at NYU Winthrop Hospital, Mineola, NY, United States; Meredith Akerman, The Children’s Medical Center at NYU Winthrop Hospital, Mineola, NY, United States; Brooke Senken, Indiana University School of Medicine/Riley Hospital for Children, Indianapolis, IN, United States

Dyana Picache, BS, DO
Resident Physicial
NYU Langone Long Island Department of Pediatrics
Upper Saddle River, New Jersey, United States
Presenting Author(s)
Background: Respiratory Syncytial Virus (RSV) is the leading cause of lower respiratory tract illness in infants, accounting for 3.4 million hospitalizations worldwide. Apnea is a complication that has long been associated with RSV, particularly for premature infants and those < 3 months old. However risk of apnea is not exclusive to RSV and admission based only on RSV diagnosis may be misguided. There is little data available to recommend admission criteria for RSV in infants without risk factors.
Objective: We studied the risk of apnea in otherwise healthy infants < 6 mo based on severity of illness at presentation. We also compared clinical courses between mild and severe disease groups.
Design/Methods: This is a retrospective chart review of infants evaluated in the emergency department (ED) over 3 consecutive RSV seasons: 2017-2018, 2018-2019, and 2019-2020. We included infants < 6 mo with RSV diagnosed using multiplex PCR assay. Infants with history of prematurity (≤ 37 weeks), past apnea, chronic lung disease, heart disease, airway anomalies, neuromuscular diseases, and genetic disorders were excluded. Clinical data were reviewed to separate patients into mild or severe cases. Infants with respiratory rate (RR) ≥ 60, retractions, oxygen saturation < 90%, poor oral intake, or dehydration were classified as severe.
Results: A total of 161 infants met study criteria: 52 mild and 109 severe. There was no risk of apnea in mild cases and low risk in severe cases. Significant differences included length of stay (LOS), oxygen requirement, ICU admission, and hospital readmission (Table 1). About 59% of severe cases required oxygen support, the majority of which received high flow nasal cannula, while 29% of mild cases required support and most were placed on regular nasal cannula (Table 2). Twenty-seven severe cases required ICU and LOS was 1 day longer than mild. Forty-two severe cases were readmitted after initial discharge compared to 2 mild cases.Conclusion(s): There was a low incidence of apnea in full term infants < 6 mo with RSV regardless of severity of disease, suggesting that risk of apnea is not a reliable factor when considering hospital admission. Conversely, high RR, retractions, hypoxia on presentation, poor PO intake, and dehydration were specific to severe RSV disease. The differences in oxygen support, ICU admission, and readmission emphasize the importance of identifying mild versus severe RSV to anticipate clinical courses. Further studies are needed to standardize and validate characteristics of RSV that require hospitalization.
Table 1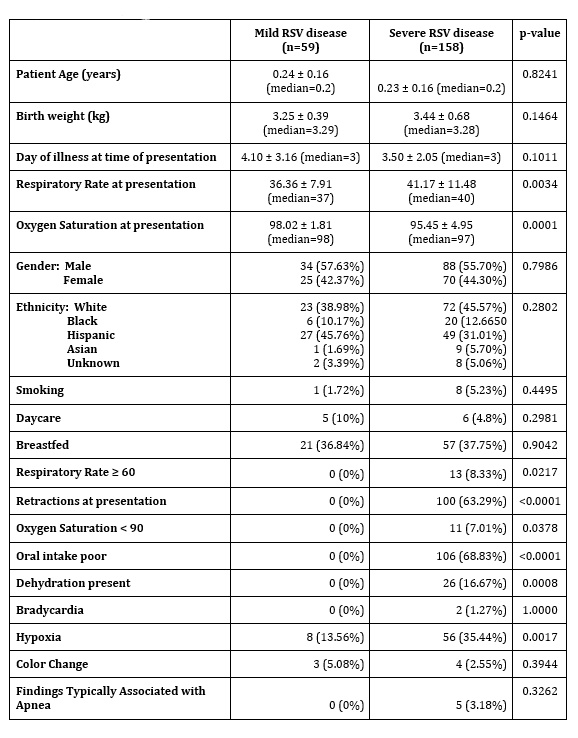 Patient Characteristics
Patient Characteristics
Table 2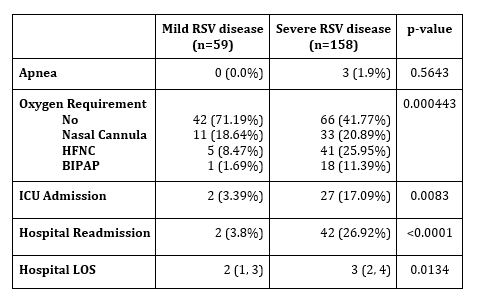 Outcomes
Outcomes
Objective: We studied the risk of apnea in otherwise healthy infants < 6 mo based on severity of illness at presentation. We also compared clinical courses between mild and severe disease groups.
Design/Methods: This is a retrospective chart review of infants evaluated in the emergency department (ED) over 3 consecutive RSV seasons: 2017-2018, 2018-2019, and 2019-2020. We included infants < 6 mo with RSV diagnosed using multiplex PCR assay. Infants with history of prematurity (≤ 37 weeks), past apnea, chronic lung disease, heart disease, airway anomalies, neuromuscular diseases, and genetic disorders were excluded. Clinical data were reviewed to separate patients into mild or severe cases. Infants with respiratory rate (RR) ≥ 60, retractions, oxygen saturation < 90%, poor oral intake, or dehydration were classified as severe.
Results: A total of 161 infants met study criteria: 52 mild and 109 severe. There was no risk of apnea in mild cases and low risk in severe cases. Significant differences included length of stay (LOS), oxygen requirement, ICU admission, and hospital readmission (Table 1). About 59% of severe cases required oxygen support, the majority of which received high flow nasal cannula, while 29% of mild cases required support and most were placed on regular nasal cannula (Table 2). Twenty-seven severe cases required ICU and LOS was 1 day longer than mild. Forty-two severe cases were readmitted after initial discharge compared to 2 mild cases.Conclusion(s): There was a low incidence of apnea in full term infants < 6 mo with RSV regardless of severity of disease, suggesting that risk of apnea is not a reliable factor when considering hospital admission. Conversely, high RR, retractions, hypoxia on presentation, poor PO intake, and dehydration were specific to severe RSV disease. The differences in oxygen support, ICU admission, and readmission emphasize the importance of identifying mild versus severe RSV to anticipate clinical courses. Further studies are needed to standardize and validate characteristics of RSV that require hospitalization.
Table 1
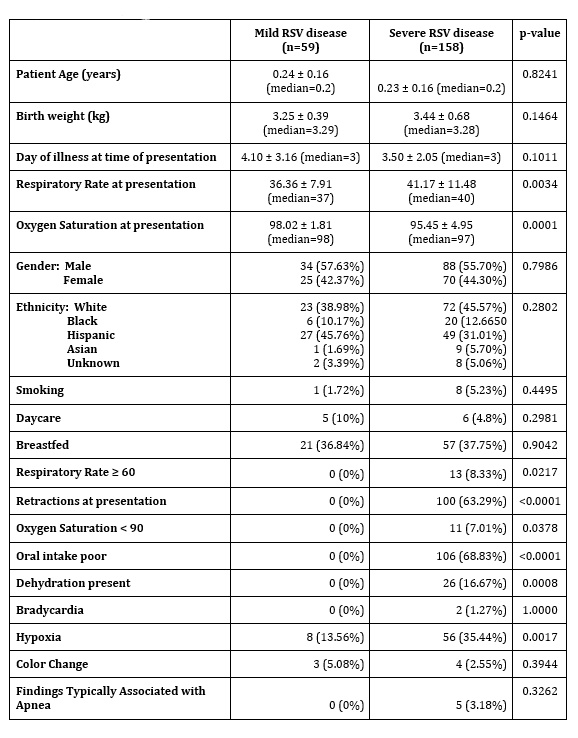 Patient Characteristics
Patient CharacteristicsTable 2
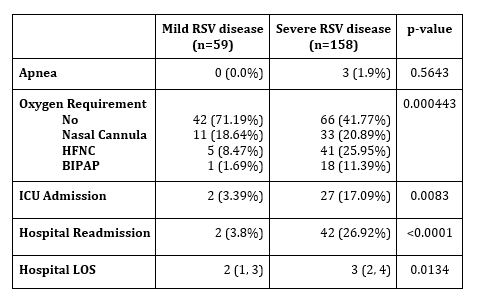 Outcomes
Outcomes