Neonatal Follow-up
Category: Abstract Submission
Neonatal Follow-up II
259 - Small for Gestational Age Status Affects Growth and Neurodevelopmental Outcomes in Very Low Birth Weight Infants
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 259
Publication Number: 259.224
Publication Number: 259.224
Raechel Irons, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Katherine E. Chetta, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Myla Ebeling, Northeast Ohio Medical University, Charleston, SC, United States; Carol L. Wagner, Medical University of South Carolina College of Medicine, Charleston, SC, United States; Lakshmi D. Katikaneni, MUSC Children's Hospital, Charleston, SC, United States

Raechel Irons, MD
Neonatal-Perinatal Medicine Fellow
Medical University of South Carolina College of Medicine
Charleston, South Carolina, United States
Presenting Author(s)
Background: SGA status infants may fail to catch up to their AGA peers in NICU and after discharge. SGA status may also be associated with worse neurodevelopmental outcomes.
Objective: To study the effect of SGA status on long-term consequences. A cohort of 270 singleton infants born at < 1500g between 2008-2017 who were SGA were compared to 900 AGA infants who were matched for PMA. We hypothesized that the SGA cohort would have inferior neurodevelopmental outcomes when compared to the AGA group.
Design/Methods: We reviewed the MUSC EMR, and included infants from 2008-2017 who were singletons and < 1500 grams. After discharge, infants returned to an outpatient clinic which completed medical and neurodevelopmental assessments, also included in this study. During this time, our unit provided early parenteral nutrition, and a rapid enteral feeding protocol. Multivariate linear regression was used to evaluate variables associated with neurodevelopment was adjusted for gender, birth GA, age in months at follow-up, and gains in length, head circumference, and weight from discharge to visit. Significance was defined as p-value < 0.05.
Results: 23.1% of infants < 1500 grams were SGA. SGA infants grew similarly to AGA infants in weight, length, and head circumference at discharge (p= < 0.001). Both groups were predominately black (n=718) followed by white (n=386). SGA group had z-scores below the AGA group. SGA head circumference at birth and discharge z-scores were -1.07 and -1.67, compared to AGA which was 0.27 and -0.59 respectively. This was in the setting of worse Grade 3/4 IVH and BPD outcomes in the AGA group (p=0.02 and < 0.001 respectively). Between 5-15 months of chronologic age, 58.1% of AGA infants and 62.2% of SGA infants returned to clinic. There were no changes in demographics between hospital and clinic. There was no difference in length and weight gain/kg/day. AGA follow up patients grew more appropriately in all parameters with z-scores consistently higher than SGA infants. SGA catch up growth did not occur in the NICU or the follow up period in this study. Adjusting for variables including sex, birth GA, age at visit, and growth from discharge to visit, lower adjusted language and gross motor raw scores were associated with SGA (p=0.005 and p=0.006).Conclusion(s): Despite current strategies, SGA infants are at high risk of neurodevelopmental impairment in language and gross motor domains. Expected SGA weight gain exceeding AGA infants was not seen. This may explain worse neurodevelopmental outcomes. Novel care strategies may be needed to improve outcomes in both catch up growth and development.
Anthropometric Z-scores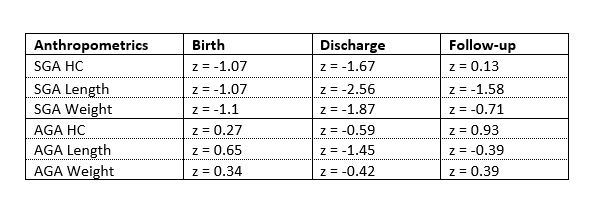 Anthropometric z-scores for infants at birth, NICU discharge, and follow-up
Anthropometric z-scores for infants at birth, NICU discharge, and follow-up
Objective: To study the effect of SGA status on long-term consequences. A cohort of 270 singleton infants born at < 1500g between 2008-2017 who were SGA were compared to 900 AGA infants who were matched for PMA. We hypothesized that the SGA cohort would have inferior neurodevelopmental outcomes when compared to the AGA group.
Design/Methods: We reviewed the MUSC EMR, and included infants from 2008-2017 who were singletons and < 1500 grams. After discharge, infants returned to an outpatient clinic which completed medical and neurodevelopmental assessments, also included in this study. During this time, our unit provided early parenteral nutrition, and a rapid enteral feeding protocol. Multivariate linear regression was used to evaluate variables associated with neurodevelopment was adjusted for gender, birth GA, age in months at follow-up, and gains in length, head circumference, and weight from discharge to visit. Significance was defined as p-value < 0.05.
Results: 23.1% of infants < 1500 grams were SGA. SGA infants grew similarly to AGA infants in weight, length, and head circumference at discharge (p= < 0.001). Both groups were predominately black (n=718) followed by white (n=386). SGA group had z-scores below the AGA group. SGA head circumference at birth and discharge z-scores were -1.07 and -1.67, compared to AGA which was 0.27 and -0.59 respectively. This was in the setting of worse Grade 3/4 IVH and BPD outcomes in the AGA group (p=0.02 and < 0.001 respectively). Between 5-15 months of chronologic age, 58.1% of AGA infants and 62.2% of SGA infants returned to clinic. There were no changes in demographics between hospital and clinic. There was no difference in length and weight gain/kg/day. AGA follow up patients grew more appropriately in all parameters with z-scores consistently higher than SGA infants. SGA catch up growth did not occur in the NICU or the follow up period in this study. Adjusting for variables including sex, birth GA, age at visit, and growth from discharge to visit, lower adjusted language and gross motor raw scores were associated with SGA (p=0.005 and p=0.006).Conclusion(s): Despite current strategies, SGA infants are at high risk of neurodevelopmental impairment in language and gross motor domains. Expected SGA weight gain exceeding AGA infants was not seen. This may explain worse neurodevelopmental outcomes. Novel care strategies may be needed to improve outcomes in both catch up growth and development.
Anthropometric Z-scores
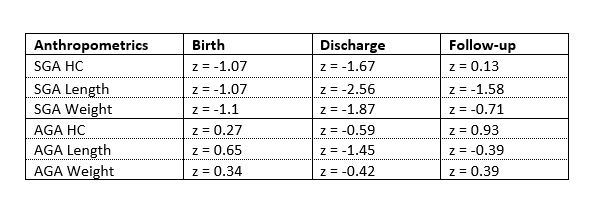 Anthropometric z-scores for infants at birth, NICU discharge, and follow-up
Anthropometric z-scores for infants at birth, NICU discharge, and follow-up