Obesity
Category: Abstract Submission
Obesity II
531 - Variables Impacting Obesity Diagnosis Documentation and Comorbidity Screening in Pediatrics
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 531
Publication Number: 531.239
Publication Number: 531.239
Arek Hidirsah, Children's Hospital Los Angeles, CHATSWORTH, CA, United States; Juan C. Espinoza, Children's Hospital Los Angeles, Los Angeles, CA, United States; Yan Chai, Children's Hospital Los Angeles, Los Angeles, CA, United States

Arek Hidirsah, MD
Adolescent Medicine Fellow
Children's Hospital Los Angeles
CHATSWORTH, California, United States
Presenting Author(s)
Background: Obesity continues to be a major health issue in pediatrics. Multiple organizations and societies recommend screening for hyperlipidemia (HLD), nonalcoholic fatty liver disease (NAFLD), and Type 2 Diabetes (DM2) in youth with obesity. Despite these recommendations, the literature shows screening rates are inadequate at 8-63% for DM2, 8-54% for HLD, and 2-63% NAFLD.
Objective: 1) Which patients receive a diagnostic code for obesity?
2) Which are most likely to be screened for for HLD, NAFLD, and DM2?
Design/Methods: A query of the Trinetx database was done on Sep 1 2021. Inclusion criteria included Individuals 14-18 years of age at time of query, ≥3 outpatient encounters between Jan 1 2017 - Mar 1 2020, and BMI 30 or 95th% documented on 3 separate encounters. Exclusion criteria were a diagnostic code for HLD, NAFLD, DM2 prior to Jan 1 2017,and a diagnosis of Type 1 Diabetes. Obesity diagnosis documentation was defined by the presence of any ICD-10 code for obesity. Screening for comorbidities was defined by the presence of lab results for total cholesterol+LDL, ALT, and HgbA1C. Logistic regression models were used to estimate associations between demographics in the population and the likelihood of diagnosis of obesity and screening for comorbidities.
Results: The cohort included 35,898 patients (Table 1). Black, Native Hawaiian or Other Pacific Islander, & Hispanic patients had the highest odds of having a documented diagnosis of obesity (Table 2). Younger age at start of the study period increased odds as well. Documentation of obesity increased the odds of screening for all comorbidities (Table 3). American Indian or Alaska Native & Asian patients had the highest odds of being screened for all comorbidities.Conclusion(s): Documentation of obesity diagnosis and screening for comorbidities continue to fall short of recommendations. Though prior studies have suggested demographic variables impact the likelihood of being diagnosed with obesity and screened for comorbidities, to our knowledge this is the first study utilizing a large, real-world national dataset. Further studies are warranted to explore the causes of demographic variation and overall low documentation and screening rates among youth with obesity.
Arek PAS CVArek PAS CV .pdf
Obesity Documentation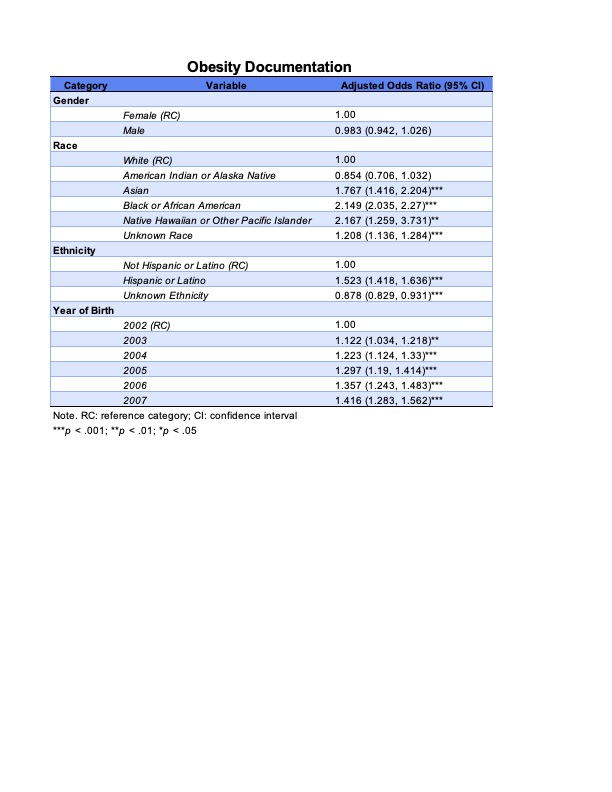 Adjusted odds ratios for the documentation of obesity by category and variable.
Adjusted odds ratios for the documentation of obesity by category and variable.
Objective: 1) Which patients receive a diagnostic code for obesity?
2) Which are most likely to be screened for for HLD, NAFLD, and DM2?
Design/Methods: A query of the Trinetx database was done on Sep 1 2021. Inclusion criteria included Individuals 14-18 years of age at time of query, ≥3 outpatient encounters between Jan 1 2017 - Mar 1 2020, and BMI 30 or 95th% documented on 3 separate encounters. Exclusion criteria were a diagnostic code for HLD, NAFLD, DM2 prior to Jan 1 2017,and a diagnosis of Type 1 Diabetes. Obesity diagnosis documentation was defined by the presence of any ICD-10 code for obesity. Screening for comorbidities was defined by the presence of lab results for total cholesterol+LDL, ALT, and HgbA1C. Logistic regression models were used to estimate associations between demographics in the population and the likelihood of diagnosis of obesity and screening for comorbidities.
Results: The cohort included 35,898 patients (Table 1). Black, Native Hawaiian or Other Pacific Islander, & Hispanic patients had the highest odds of having a documented diagnosis of obesity (Table 2). Younger age at start of the study period increased odds as well. Documentation of obesity increased the odds of screening for all comorbidities (Table 3). American Indian or Alaska Native & Asian patients had the highest odds of being screened for all comorbidities.Conclusion(s): Documentation of obesity diagnosis and screening for comorbidities continue to fall short of recommendations. Though prior studies have suggested demographic variables impact the likelihood of being diagnosed with obesity and screened for comorbidities, to our knowledge this is the first study utilizing a large, real-world national dataset. Further studies are warranted to explore the causes of demographic variation and overall low documentation and screening rates among youth with obesity.
Arek PAS CVArek PAS CV .pdf
Obesity Documentation
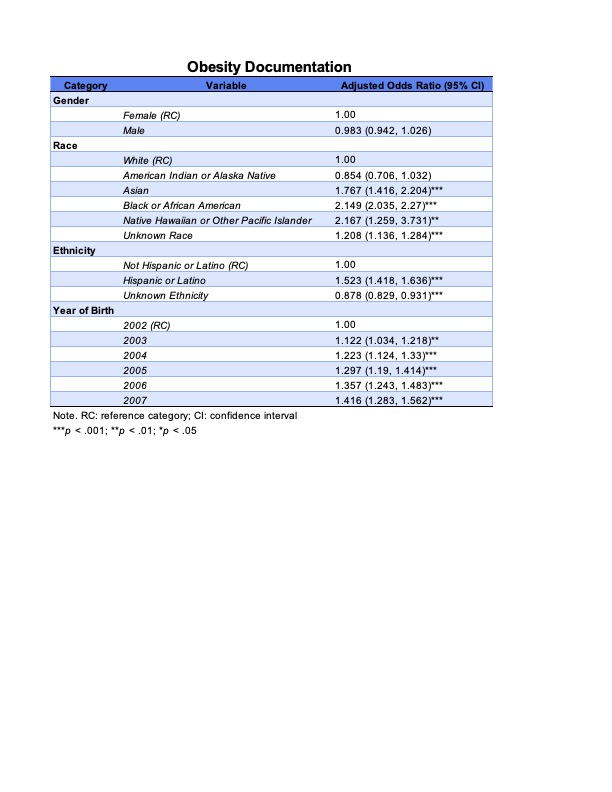 Adjusted odds ratios for the documentation of obesity by category and variable.
Adjusted odds ratios for the documentation of obesity by category and variable.