Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine V
348 - Variation in Emergency Department Use of Racemic Epinephrine and Associated Outcomes for Croup
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 348
Publication Number: 348.204
Publication Number: 348.204
Patrick S. Walsh, Cincinnati Children's Hospital Medical Center, Ludlow, KY, United States; Yin Zhang, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Matthew J. Lipshaw, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States

Patrick S. Walsh, MD
Clinical Fellow
Cincinnati Children's Hospital Medical Center
Ludlow, Kentucky, United States
Presenting Author(s)
Background: Racemic epinephrine (RE) is commonly administered for croup in the emergency department (ED), but there are no national guidelines for its administration. Administration of multiple doses of RE can be the basis for hospitalization.
Objective: Our objectives were to examine variation in RE use between EDs, to assess whether ED-level variation is due to hospital or patient factors, and to assess the association between hospital RE use and patient outcomes.
Design/Methods: We performed a retrospective cohort study of children aged 3-months to 10-years with croup in the ED in 2016 – 2020 using the Pediatric Heath Information System. We used mixed-effects regression to evaluate patient and hospital factors associated with RE use, to calculate risk-standardized proportions of patients receiving RE in each ED and to analyze the relationship between risk-standardized RE use and patient outcomes of hospitalization, ICU admission and ED revisits.
Results: We analyzed 231,683 patient visits from 39 hospitals. ED administration of RE varied from 14%-48% of visits (median 24.5%; IQR 20.0%-27.8%) at each site. 8.6% of patients were hospitalized, 1% were admitted to the ICU, and 5.3% had a return visit to the ED within 3 days. We found increased odds of RE use in patients with male sex (odds ratio [OR] 1.39, 95% confidence interval [CI]: 1.36-1.42), white race (OR 1.38, 95% CI: 1.33-1.42), privately insured (OR 1.51, 95% CI: 1.48-1.54), with previous croup (OR 1.26, 95% CI: 1.22-1.29), presenting in the fall season (OR 1.39, 95% CI: 1.35-1.43), and arriving overnight (OR 1.35, 95% CI: 1.32-1.38) in our multivariable model adjusting for site as random effect. Hospital effects predicted institutional RE use more closely than case mix (Figure 1). After standardizing for case mix and adjusting for site effects, increasing ED use of RE per site was associated with increasing odds of hospital admission (OR 1.39, 95% CI: 1.01-1.91), but not ICU admission (OR 1.39, 95% CI: 0.99-1.97) or ED revisit (OR 1.00, 95% CI: 0.92-1.09). This means that for every 10% increase in site-specific rate of RE use, we found 39% greater odds of hospitalization. The relationships between institutional RE use and outcomes are shown in Figure 2.Conclusion(s): In this large observational study, RE administration varied widely across EDs. Increasing ED-level RE use was associated with hospital admission but not ICU admission or ED revisit. Standardization of RE use may reduce hospital admission in children with croup.
CV for Patrick Walsh MDPatrickWalshCV--12.22.21.pdf
Figure 2: Risk-standardized racemic epinephrine use and outcomes by hospital.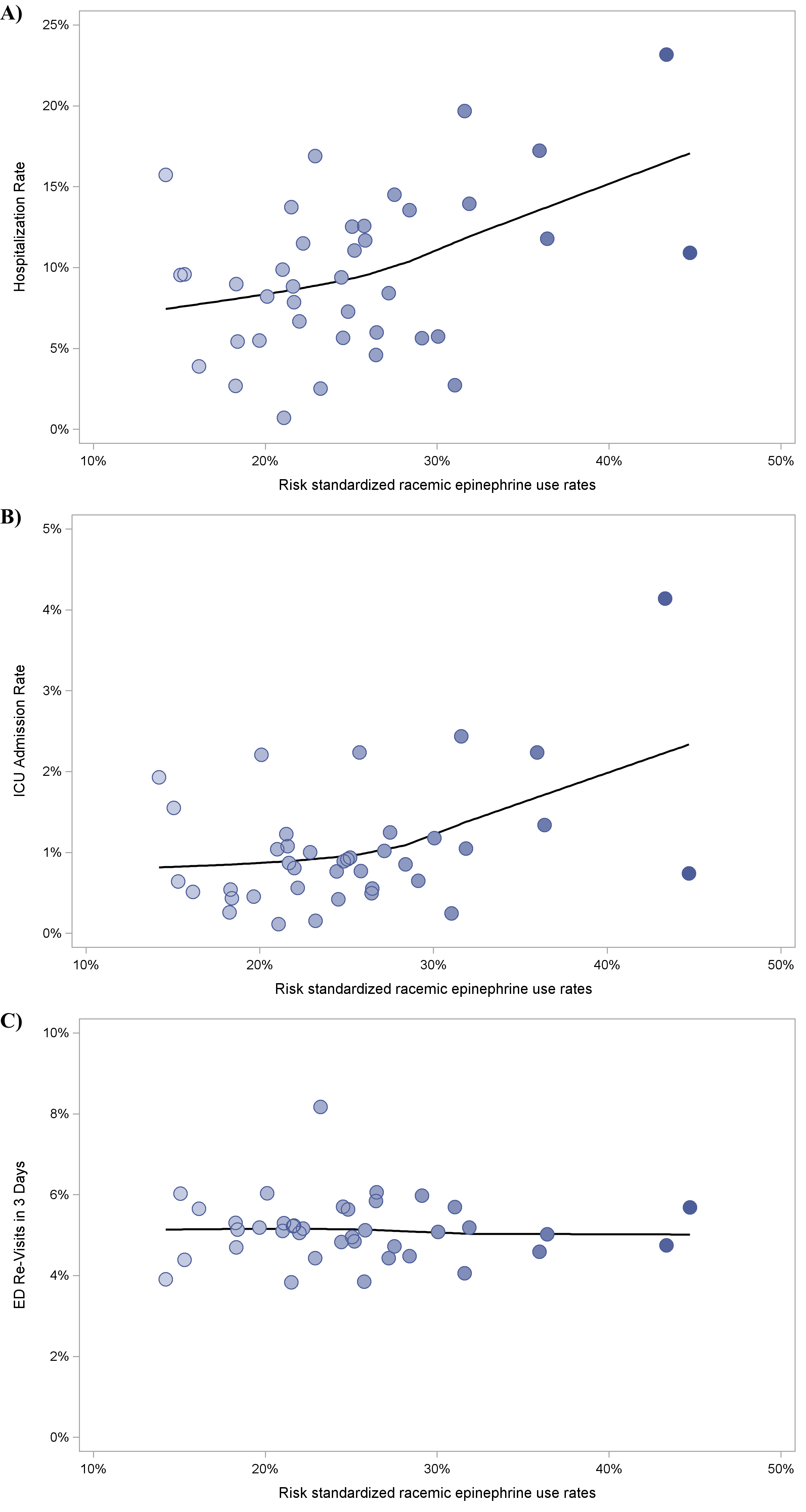 Individual hospitals are represented by points and the trend is shown by the regression line. A, Hospitalization rate by racemic epinephrine use. B, ICU admission rate by racemic epinephrine use. C, 3-day ED revisit rate by racemic epinephrine use.
Individual hospitals are represented by points and the trend is shown by the regression line. A, Hospitalization rate by racemic epinephrine use. B, ICU admission rate by racemic epinephrine use. C, 3-day ED revisit rate by racemic epinephrine use.
Objective: Our objectives were to examine variation in RE use between EDs, to assess whether ED-level variation is due to hospital or patient factors, and to assess the association between hospital RE use and patient outcomes.
Design/Methods: We performed a retrospective cohort study of children aged 3-months to 10-years with croup in the ED in 2016 – 2020 using the Pediatric Heath Information System. We used mixed-effects regression to evaluate patient and hospital factors associated with RE use, to calculate risk-standardized proportions of patients receiving RE in each ED and to analyze the relationship between risk-standardized RE use and patient outcomes of hospitalization, ICU admission and ED revisits.
Results: We analyzed 231,683 patient visits from 39 hospitals. ED administration of RE varied from 14%-48% of visits (median 24.5%; IQR 20.0%-27.8%) at each site. 8.6% of patients were hospitalized, 1% were admitted to the ICU, and 5.3% had a return visit to the ED within 3 days. We found increased odds of RE use in patients with male sex (odds ratio [OR] 1.39, 95% confidence interval [CI]: 1.36-1.42), white race (OR 1.38, 95% CI: 1.33-1.42), privately insured (OR 1.51, 95% CI: 1.48-1.54), with previous croup (OR 1.26, 95% CI: 1.22-1.29), presenting in the fall season (OR 1.39, 95% CI: 1.35-1.43), and arriving overnight (OR 1.35, 95% CI: 1.32-1.38) in our multivariable model adjusting for site as random effect. Hospital effects predicted institutional RE use more closely than case mix (Figure 1). After standardizing for case mix and adjusting for site effects, increasing ED use of RE per site was associated with increasing odds of hospital admission (OR 1.39, 95% CI: 1.01-1.91), but not ICU admission (OR 1.39, 95% CI: 0.99-1.97) or ED revisit (OR 1.00, 95% CI: 0.92-1.09). This means that for every 10% increase in site-specific rate of RE use, we found 39% greater odds of hospitalization. The relationships between institutional RE use and outcomes are shown in Figure 2.Conclusion(s): In this large observational study, RE administration varied widely across EDs. Increasing ED-level RE use was associated with hospital admission but not ICU admission or ED revisit. Standardization of RE use may reduce hospital admission in children with croup.
CV for Patrick Walsh MDPatrickWalshCV--12.22.21.pdf
Figure 2: Risk-standardized racemic epinephrine use and outcomes by hospital.
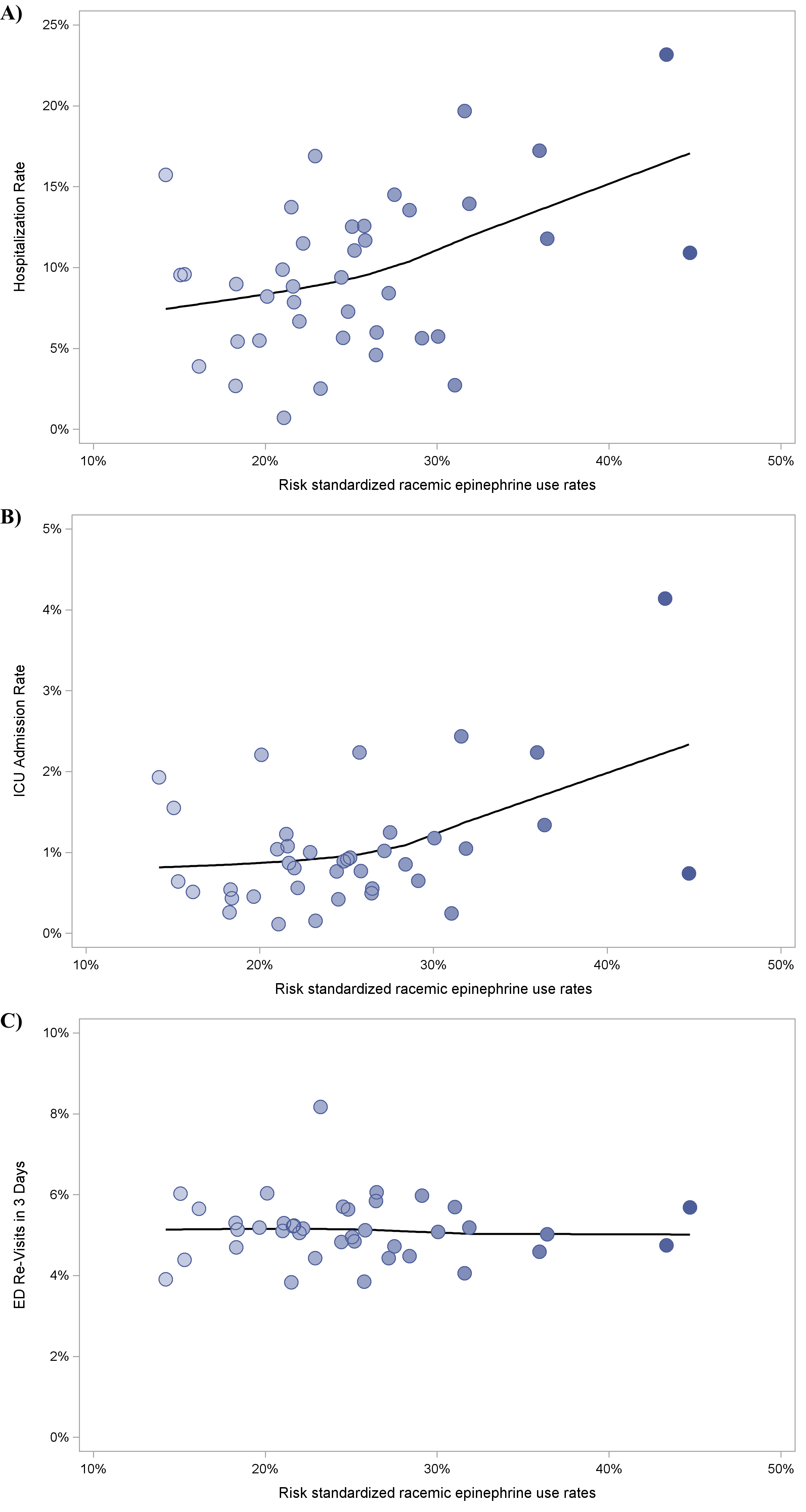 Individual hospitals are represented by points and the trend is shown by the regression line. A, Hospitalization rate by racemic epinephrine use. B, ICU admission rate by racemic epinephrine use. C, 3-day ED revisit rate by racemic epinephrine use.
Individual hospitals are represented by points and the trend is shown by the regression line. A, Hospitalization rate by racemic epinephrine use. B, ICU admission rate by racemic epinephrine use. C, 3-day ED revisit rate by racemic epinephrine use.