Medical Education: Resident
Category: Abstract Submission
Medical Education 9 - Medical Education: Resident II
241 - “TEACH”ing: Evaluation of Year 1 & 2 of a Multimodal Child Poverty Curriculum
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 241
Publication Number: 241.333
Publication Number: 241.333
Jessica Weisz, Children's National Health System, Washington, DC, United States; Dale Coddington, Children's National Health System/The George Washington University, Washington, DC, United States; Lin Chun-Seeley, Children's National Hospital, Laurel, MD, United States; Cara Lichtenstein, Children's National Hospital, Washington, DC, United States; Mary C. Ottolini, Tufts University School of Medicine, Portland, ME, United States; Olanrewaju O. Falusi, Children's National Hospital, Washington, DC, United States

Jessica Weisz, MD
Assistant Professor
Children's National Health System
Washington, District of Columbia, United States
Presenting Author(s)
Background: Understanding and addressing child poverty is critical for equitable care. Few curricula discussing poverty exist and even fewer include multimodal teaching coupled with robust evaluation.
Objective: To evaluate the effect of Years 1 & 2 of a three-year e-learning child poverty curriculum on resident knowledge and attitudes.
Design/Methods: The goal of the Trainee Education in Advocacy and Community Health (TEACH) curriculum is to train pediatric residents to recognize and address the effects of child poverty, with learning objectives modified from the US Child Poverty Curriculum (Chamberlain, 2016). The first 2 years of the curriculum included interactive e-learning modules with case simulations, pre/post knowledge questions, and reflection questions. Year 1 (Epidemiology of Child Poverty) involved completing a government benefits application, an online housing insecurity activity, and a debrief with study staff. Year 2 (Population Health & Social Determinants of Health and Biomedical Influences of Child Poverty) involved partnership with community-based organizations for in-person (prior to COVID-19)/virtual home visits. Reflection questions prompted residents to consider their assumptions and biases regarding poverty. Residents’ reflective writings were reviewed for themes.
Results: Residents demonstrated improved knowledge comparing pre- and post-test responses in each set of modules (Table 1). Post-participation Year 1 and Year 2 residents self-reported they felt more prepared to address social needs (p < 0.001) and more effective in assisting families (p < 0.001). Other attitudes showed statistical interval change in Year 1 but not Year 2 (Table 2). Themes from resident reflections showed an increased importance of continuous reflection on their biases and a recognition of their role in identifying social determinants of health during clinic visits. Conclusion(s): Residents showed increase in knowledge and change in preparedness and perceived effectiveness after participation in the curriculum. The e-learning modules, simulations, home visit activities, and reflections were key elements of the learning experience. Next steps include assessment of Year 3 and evaluation of resident application of learning objectives during a clinic visit.
Table 1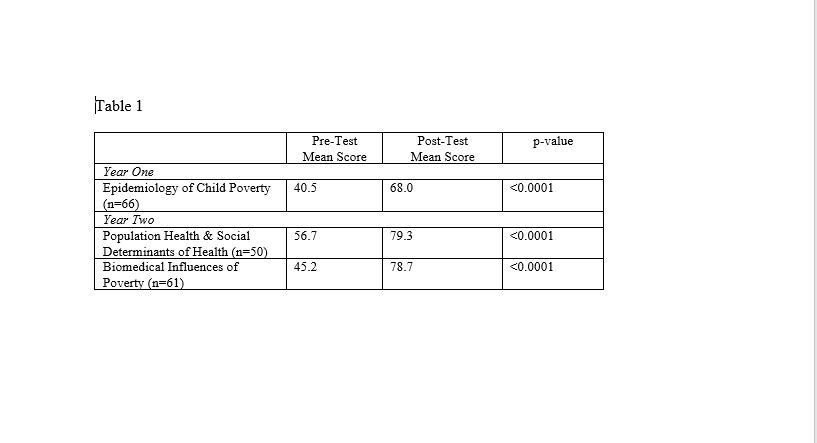
Table 2.jpg)
Objective: To evaluate the effect of Years 1 & 2 of a three-year e-learning child poverty curriculum on resident knowledge and attitudes.
Design/Methods: The goal of the Trainee Education in Advocacy and Community Health (TEACH) curriculum is to train pediatric residents to recognize and address the effects of child poverty, with learning objectives modified from the US Child Poverty Curriculum (Chamberlain, 2016). The first 2 years of the curriculum included interactive e-learning modules with case simulations, pre/post knowledge questions, and reflection questions. Year 1 (Epidemiology of Child Poverty) involved completing a government benefits application, an online housing insecurity activity, and a debrief with study staff. Year 2 (Population Health & Social Determinants of Health and Biomedical Influences of Child Poverty) involved partnership with community-based organizations for in-person (prior to COVID-19)/virtual home visits. Reflection questions prompted residents to consider their assumptions and biases regarding poverty. Residents’ reflective writings were reviewed for themes.
Results: Residents demonstrated improved knowledge comparing pre- and post-test responses in each set of modules (Table 1). Post-participation Year 1 and Year 2 residents self-reported they felt more prepared to address social needs (p < 0.001) and more effective in assisting families (p < 0.001). Other attitudes showed statistical interval change in Year 1 but not Year 2 (Table 2). Themes from resident reflections showed an increased importance of continuous reflection on their biases and a recognition of their role in identifying social determinants of health during clinic visits. Conclusion(s): Residents showed increase in knowledge and change in preparedness and perceived effectiveness after participation in the curriculum. The e-learning modules, simulations, home visit activities, and reflections were key elements of the learning experience. Next steps include assessment of Year 3 and evaluation of resident application of learning objectives during a clinic visit.
Table 1
Table 2
.jpg)
