Neonatal General
Category: Abstract Submission
Neonatology General 8: Health Disparities - Health Services Research
213 - Area Deprivation Index as an indicator of socioeconomic disadvantage: Does it predict VLBW infant outcomes?
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 213
Publication Number: 213.339
Publication Number: 213.339
Brynne Sullivan, University of Virginia School of Medicine, KESWICK, VA, United States; Ayush B. Doshi, University of Virginia School of Medicine, Charlottesville, VA, United States; Pavel Chernyavskiy, University of Virginia School of Medicine, Charlottesville, VA, United States; Rakesh Sahni, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Karen D. Fairchild, University of Virginia School of Medicine, Charlottesville, VA, United States; Joseph Isler, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Colm P. Travers, University of Alabama at Birmingham, Birmingham, AL, United States; Zachary A. Vesoulis, Washington University School of Medicine, St. Louis, MO, United States
Brynne A. Sullivan, MD, MSCR (she/her/hers)
Assistant Professor
University of Virginia
Charlottesville, Virginia, United States
Presenting Author(s)
Background: Socioeconomic status and race impact health outcomes. The Area Deprivation Index (ADI) estimates socioeconomic disadvantage using Census data on income, education, employment, and housing quality. Researchers have modified and validated the ADI to generate ranked national percentiles at the neighborhood level to provide a single quantitative metric of disadvantage.
Objective: To evaluate associations of ADI as an independent predictor of NICU mortality or in-hospital comorbidities in extremely premature infants from NICUs in different US regions.
Design/Methods: For all infants < 29 weeks gestational age admitted to 4 level IV NICUs from 2012-2019, we used Federal Information Processing Series (FIPS) codes and Neighborhood Atlas data (https://www.neighborhoodatlas.medicine.wisc.edu) to determine the National ADI percentile of all Non-Hispanic White and Black infants. We analyzed the relationship between ADI and NICU mortality using Bayesian logistic regression adjusted for site, race, birth weight, and sex. A predictor was considered significant if the posterior 95% Credible Intervals (CrI) did not include zero. We also modeled the effect of ADI on secondary outcomes, including a) having late-onset sepsis or necrotizing enterocolitis (NEC) and b) severe (grade 3-4) intraventricular hemorrhage (IVH).
Results: At 4 NICUs, data were available for 2,399 infants and demonstrated inter-center differences in patient characteristics and ADI (Table 1, Figure 1). At each NICU, Black infants lived in areas with higher ADI percentiles than White (Figure 1a, median ADI 72 vs. 55), indicating lower socioeconomic status. While there was no significant association between ADI and mortality (Figure 1b) after adjustment for demographics and site, the posterior probability of a positive association between ADI and mortality was 90%. ADI was not a significant predictor of sepsis/NEC or severe IVH. In a Bayesian multivariable model, birth weight and male sex were significant predictors of mortality, but race and center were not (Table 2). Conclusion(s): Among preterm infants < 29 weeks’ gestation admitted to four NICUs, the association between ADI percentile and mortality was not significant after adjusting for demographics and site. However, Bayesian posterior probabilities indicate that ADI may be an independent risk factor for NICU mortality.
Figure 1. Distributions of ranked national Area Deprivation index percentiles by race and mortality at each of four NICUs.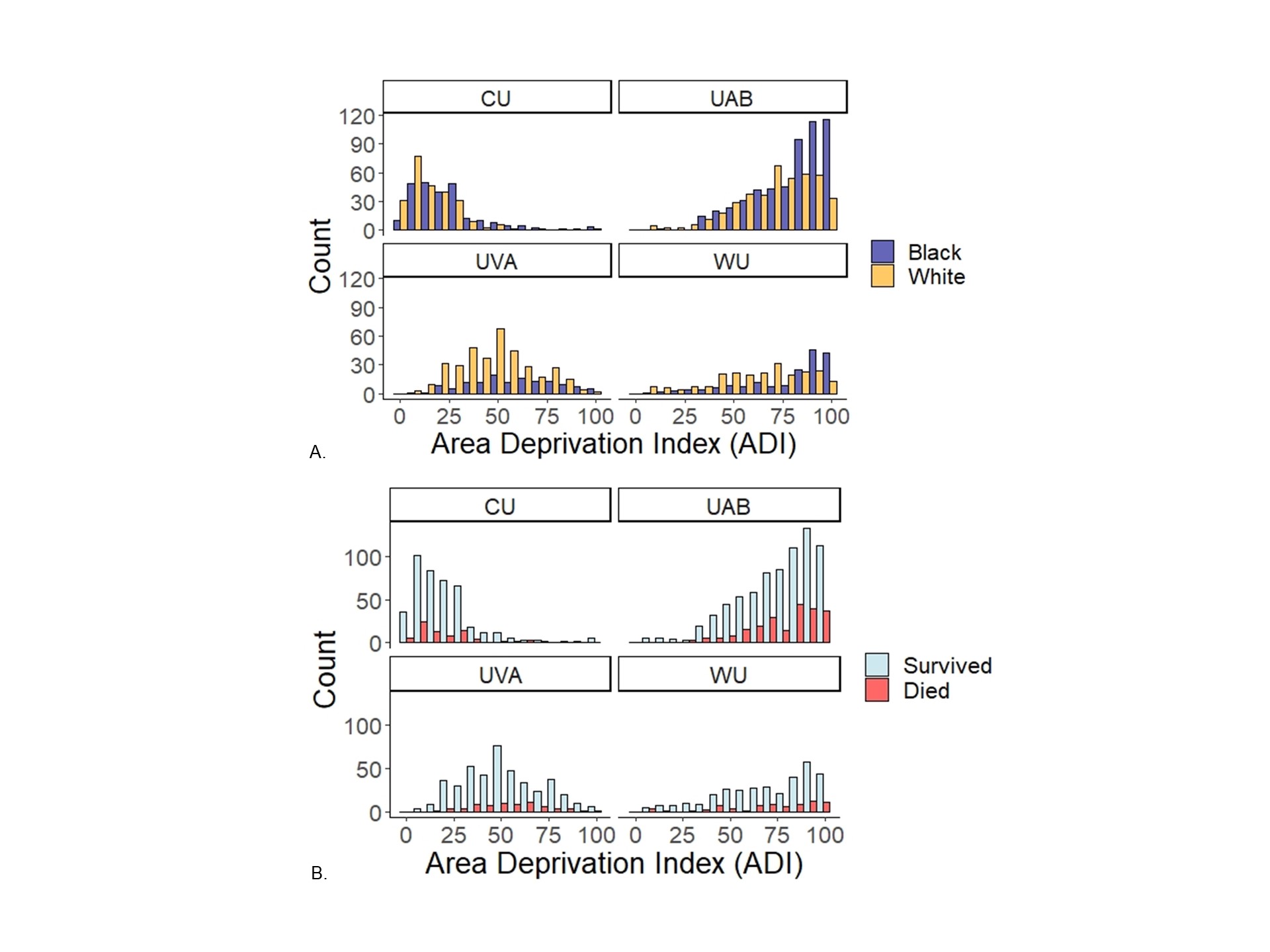 National ranked Area Deprivation Index percentiles in infants < 29 weeks gestational age at four NICUs. Panel A compares ADI between Black and White infants and Panel B compares ADI between survivors and non-survivors. ADI distributions were similar by survival status at each site but differed by race at each site, with higher ADI percentiles in Black infants compared to White. UVA = University of Virginia, WU = Washington University in St. Louis, CU = Columbia University, UAB = University of Alabama
National ranked Area Deprivation Index percentiles in infants < 29 weeks gestational age at four NICUs. Panel A compares ADI between Black and White infants and Panel B compares ADI between survivors and non-survivors. ADI distributions were similar by survival status at each site but differed by race at each site, with higher ADI percentiles in Black infants compared to White. UVA = University of Virginia, WU = Washington University in St. Louis, CU = Columbia University, UAB = University of Alabama
Table 1. Patient characteristics of infants < 29 weeks’ gestational age admitted to 4 NICUs.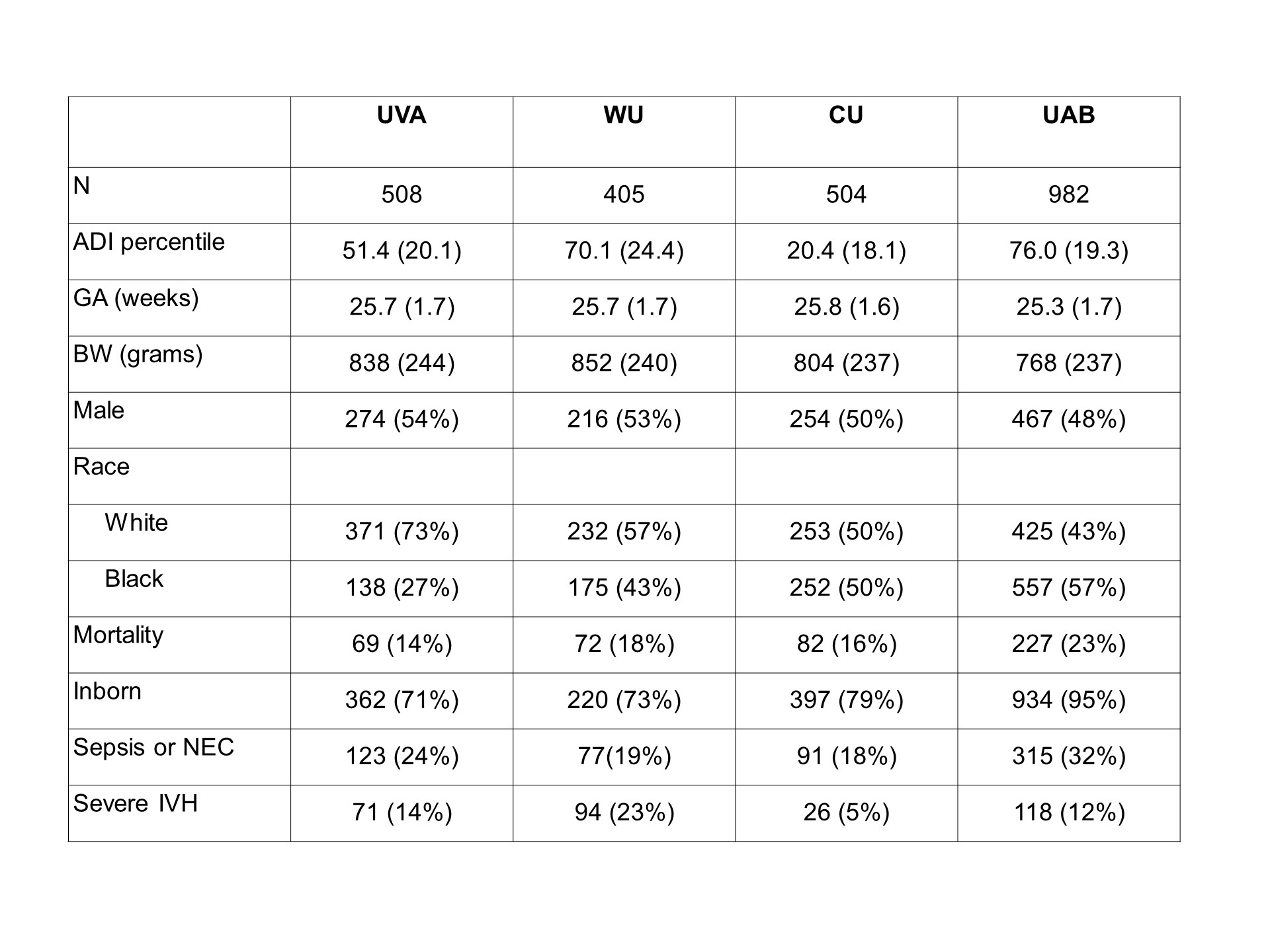 Variables are presented as mean (SD) or number (%). UVA = University of Virginia, WU = Washington University in St. Louis, CU = Columbia University, UAB = University of Alabama, NEC = necrotizing enterocolitis, Bell’s stage 2-3, Severe IVH = grade 3-4 intraventricular hemorrhage
Variables are presented as mean (SD) or number (%). UVA = University of Virginia, WU = Washington University in St. Louis, CU = Columbia University, UAB = University of Alabama, NEC = necrotizing enterocolitis, Bell’s stage 2-3, Severe IVH = grade 3-4 intraventricular hemorrhage
Objective: To evaluate associations of ADI as an independent predictor of NICU mortality or in-hospital comorbidities in extremely premature infants from NICUs in different US regions.
Design/Methods: For all infants < 29 weeks gestational age admitted to 4 level IV NICUs from 2012-2019, we used Federal Information Processing Series (FIPS) codes and Neighborhood Atlas data (https://www.neighborhoodatlas.medicine.wisc.edu) to determine the National ADI percentile of all Non-Hispanic White and Black infants. We analyzed the relationship between ADI and NICU mortality using Bayesian logistic regression adjusted for site, race, birth weight, and sex. A predictor was considered significant if the posterior 95% Credible Intervals (CrI) did not include zero. We also modeled the effect of ADI on secondary outcomes, including a) having late-onset sepsis or necrotizing enterocolitis (NEC) and b) severe (grade 3-4) intraventricular hemorrhage (IVH).
Results: At 4 NICUs, data were available for 2,399 infants and demonstrated inter-center differences in patient characteristics and ADI (Table 1, Figure 1). At each NICU, Black infants lived in areas with higher ADI percentiles than White (Figure 1a, median ADI 72 vs. 55), indicating lower socioeconomic status. While there was no significant association between ADI and mortality (Figure 1b) after adjustment for demographics and site, the posterior probability of a positive association between ADI and mortality was 90%. ADI was not a significant predictor of sepsis/NEC or severe IVH. In a Bayesian multivariable model, birth weight and male sex were significant predictors of mortality, but race and center were not (Table 2). Conclusion(s): Among preterm infants < 29 weeks’ gestation admitted to four NICUs, the association between ADI percentile and mortality was not significant after adjusting for demographics and site. However, Bayesian posterior probabilities indicate that ADI may be an independent risk factor for NICU mortality.
Figure 1. Distributions of ranked national Area Deprivation index percentiles by race and mortality at each of four NICUs.
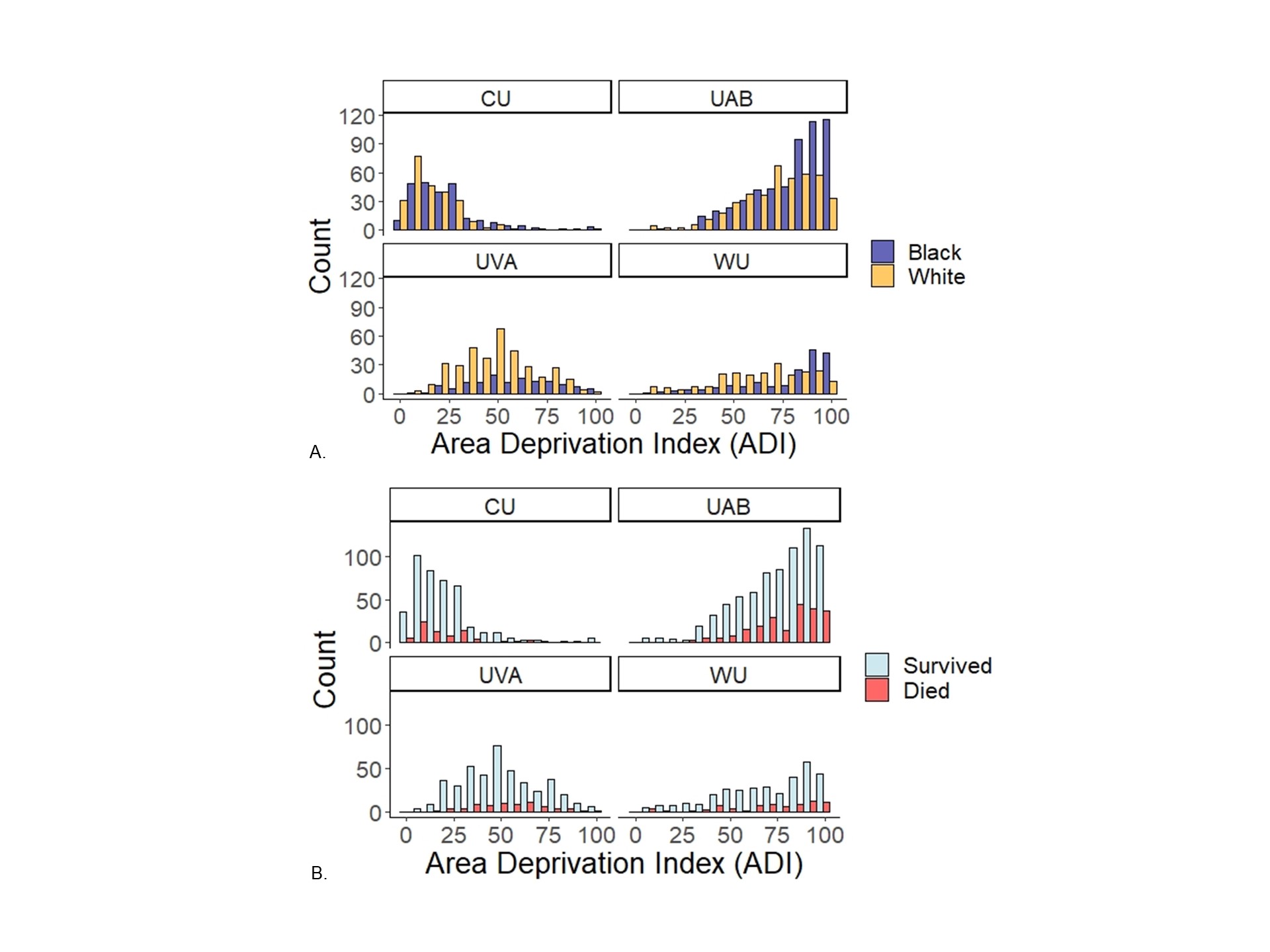 National ranked Area Deprivation Index percentiles in infants < 29 weeks gestational age at four NICUs. Panel A compares ADI between Black and White infants and Panel B compares ADI between survivors and non-survivors. ADI distributions were similar by survival status at each site but differed by race at each site, with higher ADI percentiles in Black infants compared to White. UVA = University of Virginia, WU = Washington University in St. Louis, CU = Columbia University, UAB = University of Alabama
National ranked Area Deprivation Index percentiles in infants < 29 weeks gestational age at four NICUs. Panel A compares ADI between Black and White infants and Panel B compares ADI between survivors and non-survivors. ADI distributions were similar by survival status at each site but differed by race at each site, with higher ADI percentiles in Black infants compared to White. UVA = University of Virginia, WU = Washington University in St. Louis, CU = Columbia University, UAB = University of AlabamaTable 1. Patient characteristics of infants < 29 weeks’ gestational age admitted to 4 NICUs.
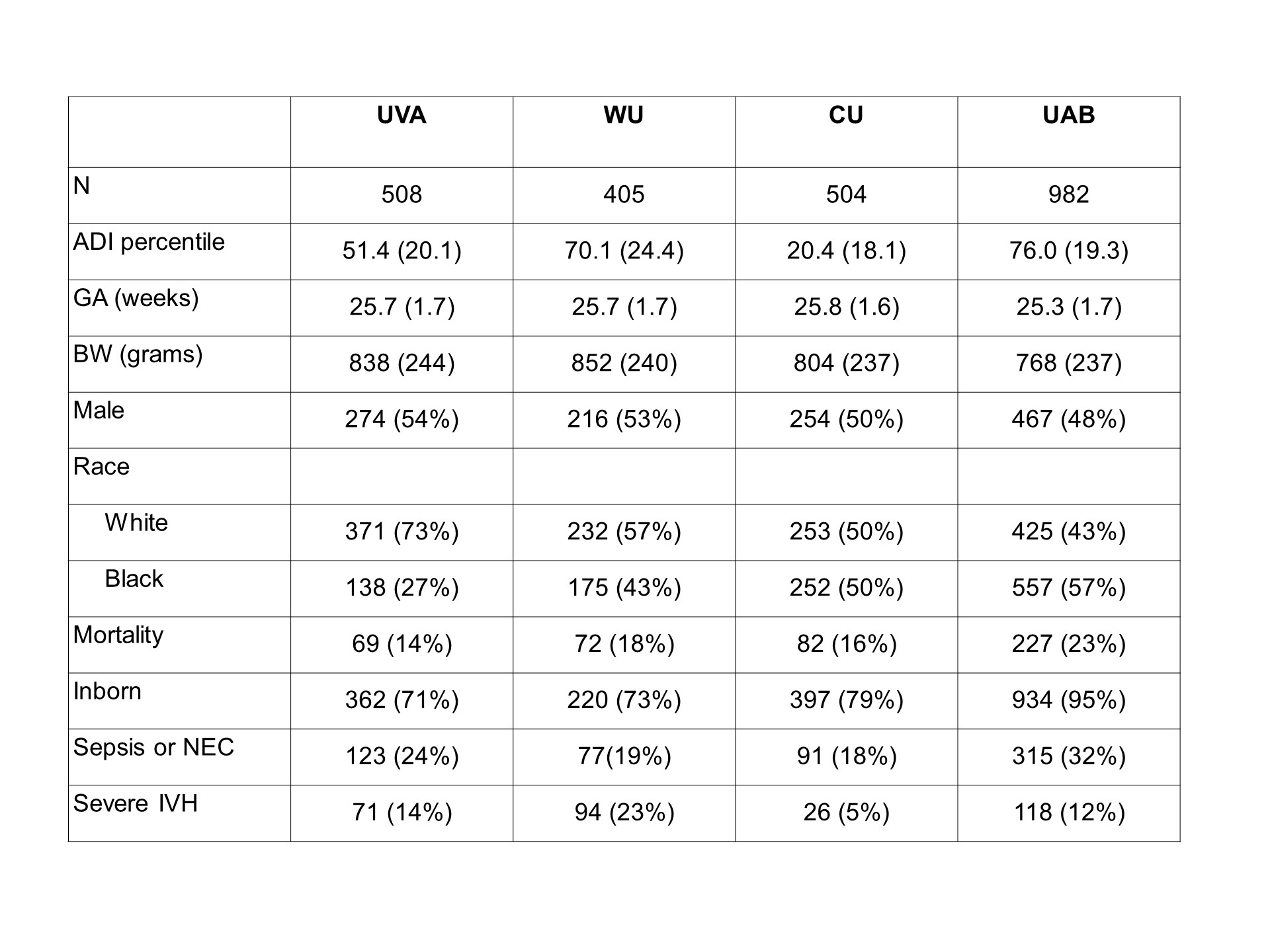 Variables are presented as mean (SD) or number (%). UVA = University of Virginia, WU = Washington University in St. Louis, CU = Columbia University, UAB = University of Alabama, NEC = necrotizing enterocolitis, Bell’s stage 2-3, Severe IVH = grade 3-4 intraventricular hemorrhage
Variables are presented as mean (SD) or number (%). UVA = University of Virginia, WU = Washington University in St. Louis, CU = Columbia University, UAB = University of Alabama, NEC = necrotizing enterocolitis, Bell’s stage 2-3, Severe IVH = grade 3-4 intraventricular hemorrhage