Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: Potpourri
555 - Association of chronologic age with different types of healthcare-associated bloodstream infections and causative pathogens in the Neonatal ICU population
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 555
Publication Number: 555.336
Publication Number: 555.336
Kyra E. Solowey, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Anshu Paul, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Irene Frantzis, Columbia University Medical Center, New York, NY, United States; Eliza Gentzler, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Surya Manickam, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; maria messina, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Sandhya S. Brachio, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States; Candace Johnson, NewYork-Presbyterian Morgan Stanley Children's Hospital, New York, NY, United States; Luis R. Alba, Columbia University Medical Center, New York, NY, United States; Lisa Saiman, Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States

Kyra E. Solowey, MD, MPH
Resident
NewYork-Presbyterian Morgan Stanley Children's Hospital
New York, New York, United States
Presenting Author(s)
Background: Infants in the NICU are at increased risk of healthcare-associated bloodstream infections (HABSIs). Few studies have examined the association of chronological age with different types of HABSIs and their causative pathogens.
Objective: Compare the frequency and causative pathogens of HABSIs that are primary BSIs, BSIs secondary to infections at another site, or central line-associated BSIs (CLABSIs) among infants of different chronological ages.
Design/Methods: We conducted a retrospective study of infants with a positive blood culture obtained on >3 days of life (DOL) in a Level IV NICU from 2010-2019. HABSIs were classified as primary, secondary to infections at another site, or central-line associated BSIs using the CDC’s National Healthcare Surveillance Network (NHSN) surveillance definitions. BSI episodes that met some, but not all, criteria for secondary BSIs were included as some symptoms are not consistently observed in neonates, e.g., meningeal signs, and some laboratory studies are not validated in neonates, e.g., > 105 colony forming units for diagnosis of urinary tract infections.
Results: In all, 261 HABSI episodes have been reviewed thus far during the study period at a median chronological age of 23 DOL. 91 (35%), 57 (22%), 71 (27%) and 42 (16%) HABSI episodes occurred at 3-14,15-28, 29-60 and >60 DOL, respectively (Table). Secondary BSIs were most common in all age strata. HABSI pathogens were most commonly coagulase negative staphylococci (CoNS, 38%). S. aureus was most common at 29-60 DOL and gram-negative rods were most common at >60 DOL.Conclusion(s): Secondary BSIs attributed to infections at another site were most common across all age groups. Primary BSIs accounted for a greater proportion of HABSIs during DOL 3-14 while CLABSIs accounted for a greater proportion of HABSIs during DOL 15-28 when compared to other age groups. Future analyses will incorporate gestational age, as it is an important factor that influences both susceptibility to BSI and length of hospital stay. An improved understanding of factors associated with primary and secondary HABSIs during a prolonged NICU stay could lead to risk reduction strategies.
Association of Chronologic Age with BSI Classification and Causative Pathogens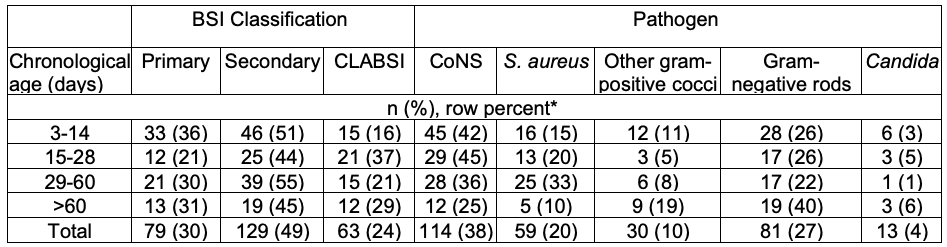 *Total percentages may exceed 100% if two NHSN definitions applied to one BSI episode.
*Total percentages may exceed 100% if two NHSN definitions applied to one BSI episode.
Objective: Compare the frequency and causative pathogens of HABSIs that are primary BSIs, BSIs secondary to infections at another site, or central line-associated BSIs (CLABSIs) among infants of different chronological ages.
Design/Methods: We conducted a retrospective study of infants with a positive blood culture obtained on >3 days of life (DOL) in a Level IV NICU from 2010-2019. HABSIs were classified as primary, secondary to infections at another site, or central-line associated BSIs using the CDC’s National Healthcare Surveillance Network (NHSN) surveillance definitions. BSI episodes that met some, but not all, criteria for secondary BSIs were included as some symptoms are not consistently observed in neonates, e.g., meningeal signs, and some laboratory studies are not validated in neonates, e.g., > 105 colony forming units for diagnosis of urinary tract infections.
Results: In all, 261 HABSI episodes have been reviewed thus far during the study period at a median chronological age of 23 DOL. 91 (35%), 57 (22%), 71 (27%) and 42 (16%) HABSI episodes occurred at 3-14,15-28, 29-60 and >60 DOL, respectively (Table). Secondary BSIs were most common in all age strata. HABSI pathogens were most commonly coagulase negative staphylococci (CoNS, 38%). S. aureus was most common at 29-60 DOL and gram-negative rods were most common at >60 DOL.Conclusion(s): Secondary BSIs attributed to infections at another site were most common across all age groups. Primary BSIs accounted for a greater proportion of HABSIs during DOL 3-14 while CLABSIs accounted for a greater proportion of HABSIs during DOL 15-28 when compared to other age groups. Future analyses will incorporate gestational age, as it is an important factor that influences both susceptibility to BSI and length of hospital stay. An improved understanding of factors associated with primary and secondary HABSIs during a prolonged NICU stay could lead to risk reduction strategies.
Association of Chronologic Age with BSI Classification and Causative Pathogens
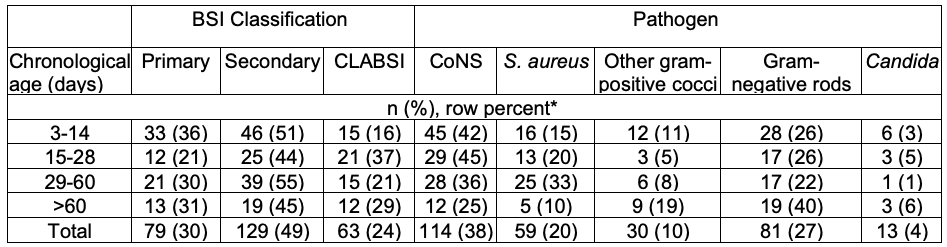 *Total percentages may exceed 100% if two NHSN definitions applied to one BSI episode.
*Total percentages may exceed 100% if two NHSN definitions applied to one BSI episode.