Nephrology: Clinical
Category: Abstract Submission
Nephrology III: General Nephrology and Dialysis
45 - Bone Structure in Children and Young Adults With Kidney Stone Disease
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 45
Publication Number: 45.340
Publication Number: 45.340
Kate B. Fitzpatrick, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Kathryn Howarth, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Lawrence Copelovitch, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Spandana Makeneni, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Erin L. Doherty, Childrens Hospital of Philadelphia, Collegeville, PA, United States; Jessica P. Lalli, Nephrology, PHILADELPHIA, PA, United States; Gregory E. Tasian, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Babette S. Zemel, Children's Hosp of Phila, Philadelphia, PA, United States; Kyla Kent, Stanford School of Medicine, Redwood City, CA, United States; LONG Jin, Stanford University, San Jose, CA, United States; Andrew J. Burghardt, University of California, San Francisco, San Francisco, CA, United States; Mary B. Leonard, Stanford University School of Medicine, Palo Alto, CA, United States; Michelle Denburg, Childrens Hospital of Philadelphia, Philadelphia, PA, United States

Kate B. Fitzpatrick
Clinical Research Coordinator
Children's Hospital of Philadelphia
Presenting Author(s)
Background: Kidney stone disease (KSD) is a systemic disorder of mineral homeostasis, and its incidence is rising disproportionately among adolescents. Population-based studies have demonstrated that patients with KSD have an increased risk of fracture and suggest particular vulnerability of growing bone. Current understanding of deficits in bone structure and strength in patients with KSD is limited.
Objective: We sought to compare high-resolution peripheral quantitative computed tomography (HR-pQCT) measures of cortical microarchitecture between children and young adults with and without KSD.
Design/Methods: This was a cross-sectional analysis of baseline data from an ongoing prospective cohort study of bone quality in patients with KSD. 55 children and young adults with idiopathic KSD, aged 5-21 years, were compared to 175 healthy controls. 24-hour urine chemistry testing (Litholink) was performed if not recently done for clinical care, and all Litholink data was collected. HR-pQCT scans were obtained in the tibial diaphysis. Measures of cortical structure and microarchitecture were compared used multivariable linear regression.
Results: Table 1 shows participant characteristics. 47% of females and 26% of males with KSD had a prior fracture (range 1 to 6 fractures). 75% of participants with KSD had ≥1 abnormal 24-urine study, with a median of 2 abnormal studies (range 1 to 10). 47% had hypercalciuria, 47% had hypocitraturia, and 34% had hyperoxaluria on ≥1 study. Participants with KSD had significantly lower cortical periosteal perimeter (mm) and cortical area (mm2) in the tibial diaphysis, compared with controls, independent of age, sex, pubertal status (Tanner stage), sex-Tanner interactions, bone length and body mass index Z-score: perimeter β = -2.9, 95% CI: -4.1, -1.7, p < 0.001, Model R2 = 0.80 and area β = -18.2, 95% CI: -26.9, -9.5, p < 0.001, Model R2 = 0.77 (Table 2). Participants with KSD also had significantly lower cortical volumetric bone mineral density (vBMD) in the tibia compared with controls, independent of cortical area, age, sex, Tanner stage, and sex-Tanner interactions: β = -18.3, 95% CI: -27.8, -8.7, p < 0.001, R2=0.61 (Table 3).Conclusion(s): High resolution imaging demonstrated impaired expansion of periosteal circumference, consistent with reduced bone formation and decreased cortical bone density. These deficits may contribute to skeletal fragility in KSD.
Table 1: Participant characteristics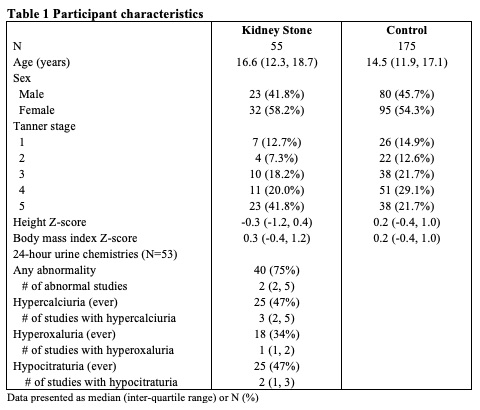
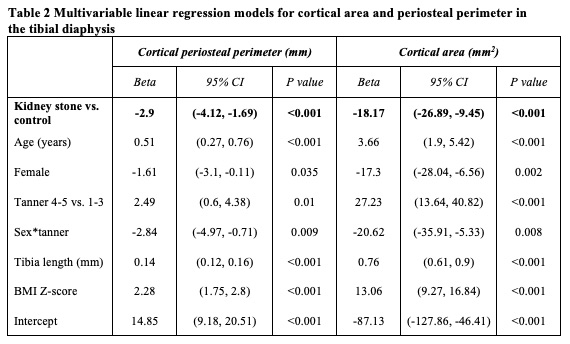
Table 2: Multivariable linear regression models for cortical area and periosteal perimeter in the tibial diaphysis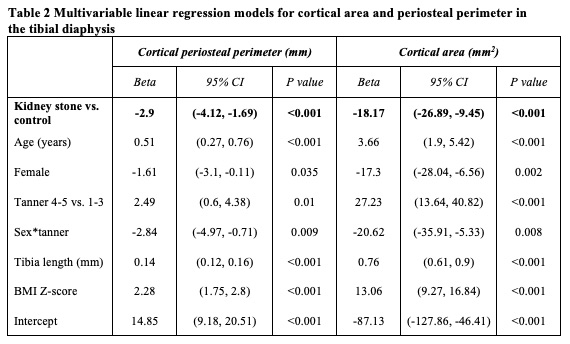
Objective: We sought to compare high-resolution peripheral quantitative computed tomography (HR-pQCT) measures of cortical microarchitecture between children and young adults with and without KSD.
Design/Methods: This was a cross-sectional analysis of baseline data from an ongoing prospective cohort study of bone quality in patients with KSD. 55 children and young adults with idiopathic KSD, aged 5-21 years, were compared to 175 healthy controls. 24-hour urine chemistry testing (Litholink) was performed if not recently done for clinical care, and all Litholink data was collected. HR-pQCT scans were obtained in the tibial diaphysis. Measures of cortical structure and microarchitecture were compared used multivariable linear regression.
Results: Table 1 shows participant characteristics. 47% of females and 26% of males with KSD had a prior fracture (range 1 to 6 fractures). 75% of participants with KSD had ≥1 abnormal 24-urine study, with a median of 2 abnormal studies (range 1 to 10). 47% had hypercalciuria, 47% had hypocitraturia, and 34% had hyperoxaluria on ≥1 study. Participants with KSD had significantly lower cortical periosteal perimeter (mm) and cortical area (mm2) in the tibial diaphysis, compared with controls, independent of age, sex, pubertal status (Tanner stage), sex-Tanner interactions, bone length and body mass index Z-score: perimeter β = -2.9, 95% CI: -4.1, -1.7, p < 0.001, Model R2 = 0.80 and area β = -18.2, 95% CI: -26.9, -9.5, p < 0.001, Model R2 = 0.77 (Table 2). Participants with KSD also had significantly lower cortical volumetric bone mineral density (vBMD) in the tibia compared with controls, independent of cortical area, age, sex, Tanner stage, and sex-Tanner interactions: β = -18.3, 95% CI: -27.8, -8.7, p < 0.001, R2=0.61 (Table 3).Conclusion(s): High resolution imaging demonstrated impaired expansion of periosteal circumference, consistent with reduced bone formation and decreased cortical bone density. These deficits may contribute to skeletal fragility in KSD.
Table 1: Participant characteristics
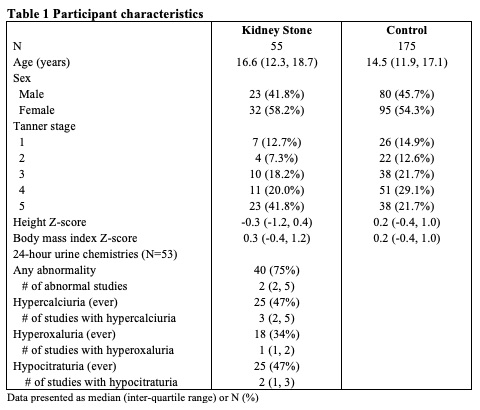
Table 2: Multivariable linear regression models for cortical area and periosteal perimeter in the tibial diaphysis