Neonatal General
Category: Abstract Submission
Neonatology General 8: Health Disparities - Health Services Research
214 - Breastfeeding rate remains low during COVID-19 pandemic in infants with neonatal opioid withdrawal syndrome (NOWS)
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 214
Publication Number: 214.339
Publication Number: 214.339
Allison Fisher, University of Utah, Salt Lake CIty, UT, United States; Adam McDougal, University of Utah Health, Salt Lake City, UT, United States; Camille M. Fung, University of Utah, Dept. of Pediatrics, Salt Lake City, UT, United States

Allison Fisher, MD (she/her/hers)
Fellow
University of Utah
Salt Lake CIty, Utah, United States
Presenting Author(s)
Background: Breastfeeding is a well-established non-pharmacological way to improve severity of NOWS in infants with in-utero drug exposure. The COVID-19 pandemic has impacted breastfeeding rates and has disproportionately affected those of lower socioeconomic and lower educational status.
Objective: The purpose of this study was to assess breastfeeding rate among infants with NOWS during the COVID-19 pandemic and compare findings to our published cohort at the University of Utah prior to the pandemic.
Design/Methods: This was a retrospective chart review of a single academic center at University of Utah. Infants born at ≥34 weeks gestational age, between January 1-December 31, 2020, who received Neonatal Withdrawal Inventory (NWI) scoring were reviewed. Infants who received NWI for non-intrauterine drug exposure were excluded. We calculated the percentages of breastfeeding rates of eligibility, initiation, and continuation at discharge. Eligibility for breastfeeding was determined by the provider permitting such use. We additionally noted infant and maternal demographic data, modes of delivery, and drug exposures per cord toxicology screens.
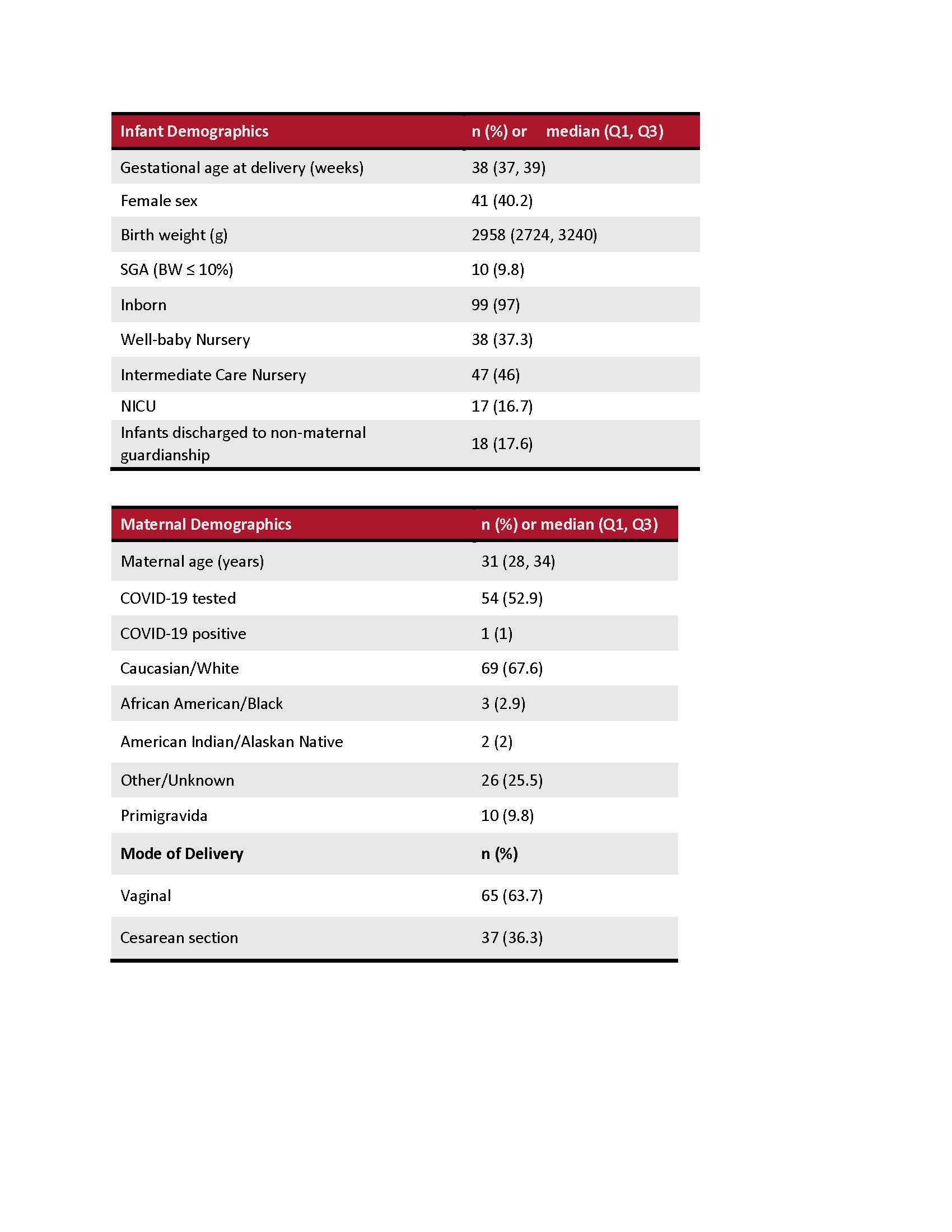
Results: Of the 125 infants reviewed, 102 infants met eligibility. Table 1 summarizes the data. Mothers of 77% infants received medication-assisted therapy (MAT) compared to only 61% in our prior study. Similar to our prior study, 21% infants had isolated opioid exposure compared to 79% with polysubstance exposure which included opioid and non-opioid substances. Sixty-five (64%) of the infants were deemed eligible to breastfeed or to receive expressed maternal milk. Fifty-seven (56% of total, 88% of breastfeeding eligible) infants received maternal milk at least once during hospitalization. However, only 37 (36% of total, 57% of breastfeeding eligible) infants were receiving maternal milk at discharge compared to 48% in our prior study. 18 (18%) infants were discharged to adoptive family or state custody and three of them were eligible to receive maternal milk but did not due to social limitations.Conclusion(s): Despite a higher rate of maternal MAT with no change in the substance exposure rates, infants with NOWS during COVID-19 suffered from the loss of benefits of breastfeeding/breastmilk feeding. The provision of maternal milk when medically safe in infants with NOWS is vital to optimizing short- and long-term outcomes. However, in this population of vulnerable mother-infant dyads, establishing and sustaining breastfeeding remains a complex challenge particularly during the COVID-19 pandemic when additional psychosocial factors and unanticipated barriers may dominate.
Infant and maternal demographics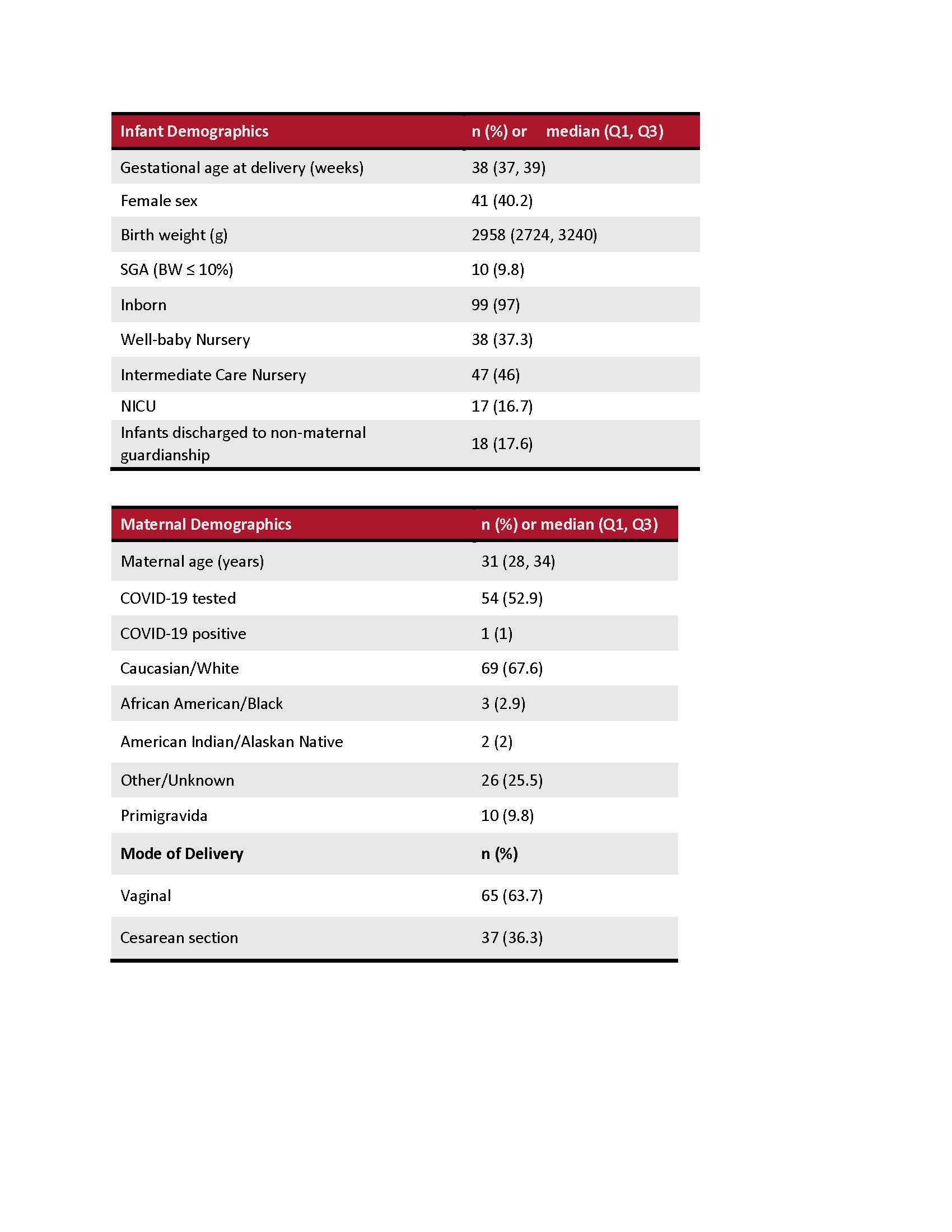
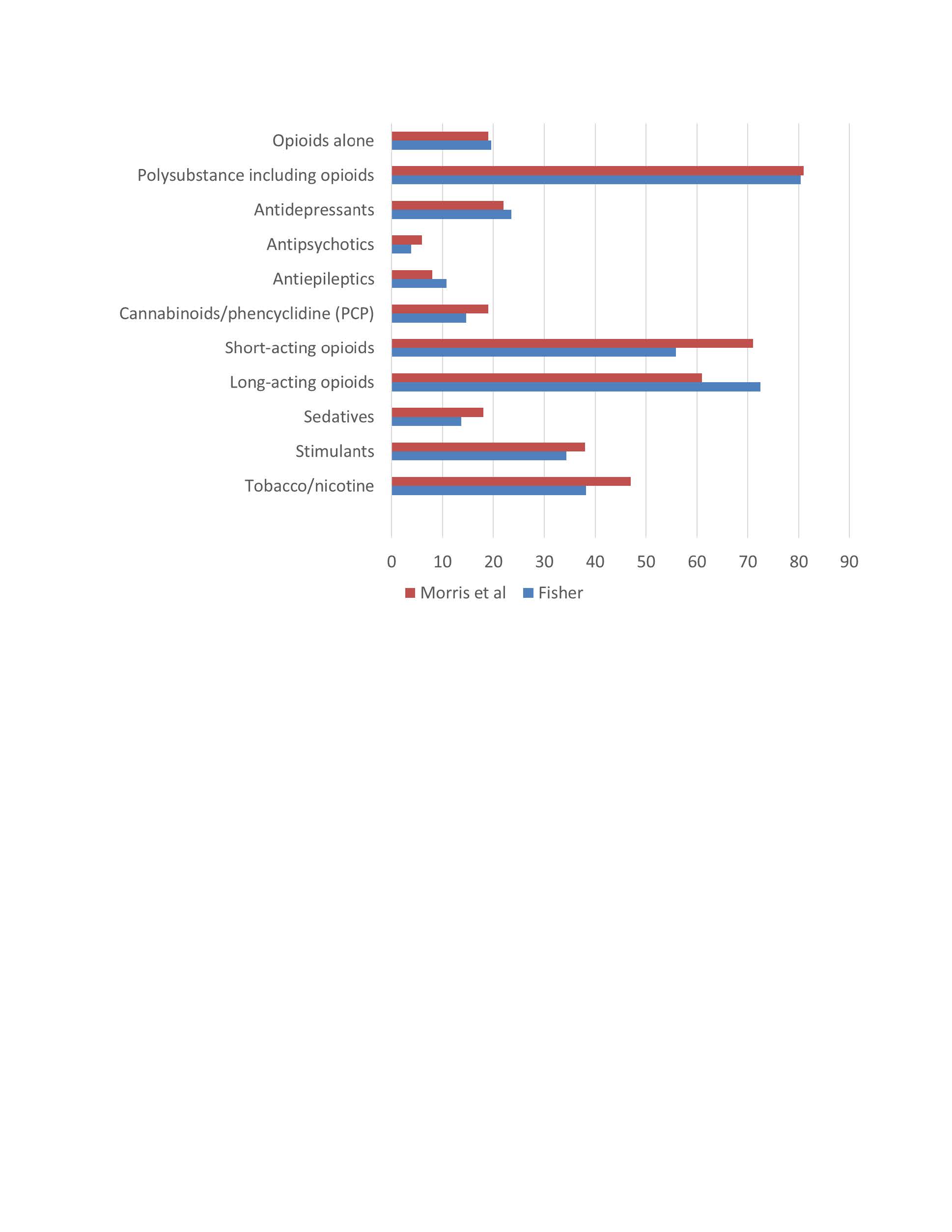
Fetal substance exposure by drug category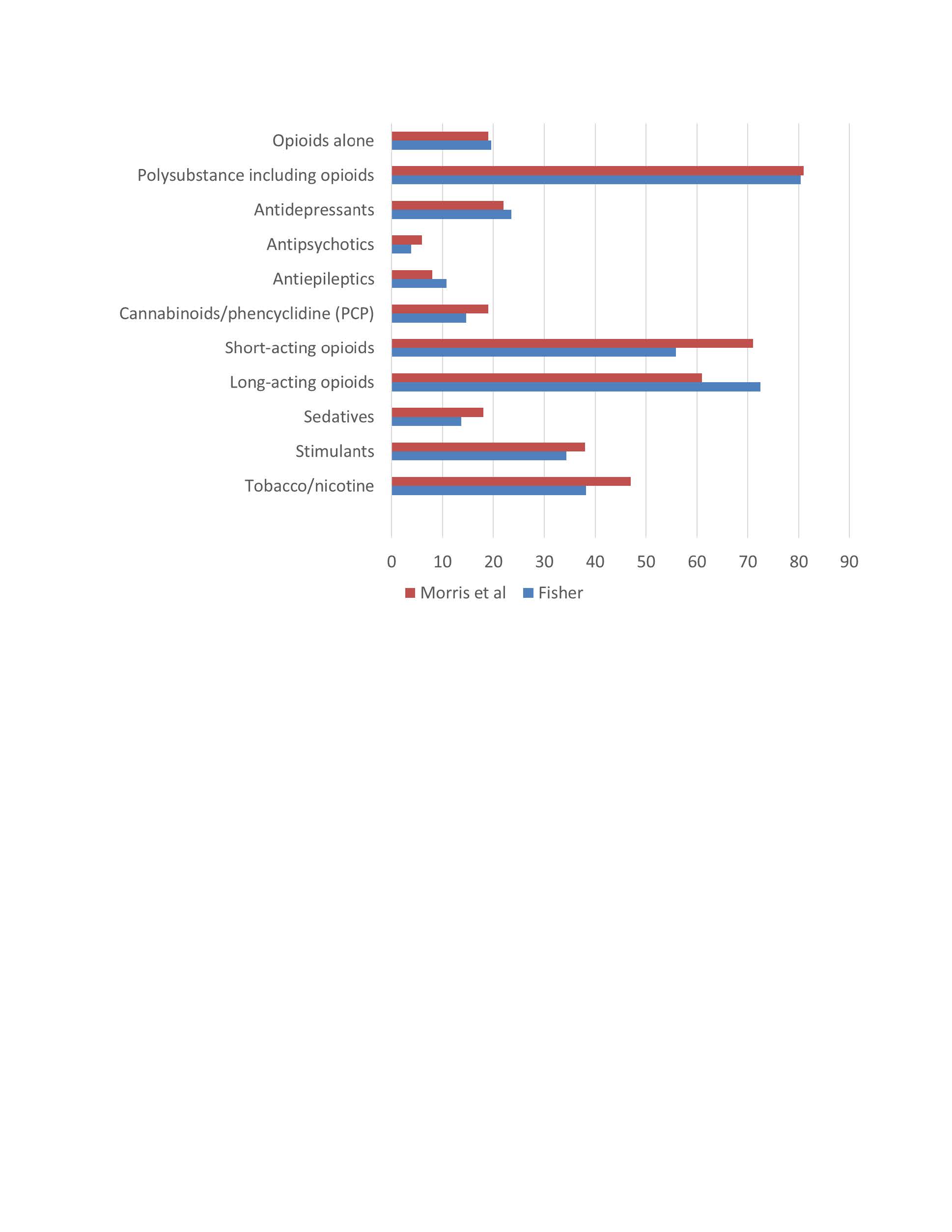
Objective: The purpose of this study was to assess breastfeeding rate among infants with NOWS during the COVID-19 pandemic and compare findings to our published cohort at the University of Utah prior to the pandemic.
Design/Methods: This was a retrospective chart review of a single academic center at University of Utah. Infants born at ≥34 weeks gestational age, between January 1-December 31, 2020, who received Neonatal Withdrawal Inventory (NWI) scoring were reviewed. Infants who received NWI for non-intrauterine drug exposure were excluded. We calculated the percentages of breastfeeding rates of eligibility, initiation, and continuation at discharge. Eligibility for breastfeeding was determined by the provider permitting such use. We additionally noted infant and maternal demographic data, modes of delivery, and drug exposures per cord toxicology screens.
Results: Of the 125 infants reviewed, 102 infants met eligibility. Table 1 summarizes the data. Mothers of 77% infants received medication-assisted therapy (MAT) compared to only 61% in our prior study. Similar to our prior study, 21% infants had isolated opioid exposure compared to 79% with polysubstance exposure which included opioid and non-opioid substances. Sixty-five (64%) of the infants were deemed eligible to breastfeed or to receive expressed maternal milk. Fifty-seven (56% of total, 88% of breastfeeding eligible) infants received maternal milk at least once during hospitalization. However, only 37 (36% of total, 57% of breastfeeding eligible) infants were receiving maternal milk at discharge compared to 48% in our prior study. 18 (18%) infants were discharged to adoptive family or state custody and three of them were eligible to receive maternal milk but did not due to social limitations.Conclusion(s): Despite a higher rate of maternal MAT with no change in the substance exposure rates, infants with NOWS during COVID-19 suffered from the loss of benefits of breastfeeding/breastmilk feeding. The provision of maternal milk when medically safe in infants with NOWS is vital to optimizing short- and long-term outcomes. However, in this population of vulnerable mother-infant dyads, establishing and sustaining breastfeeding remains a complex challenge particularly during the COVID-19 pandemic when additional psychosocial factors and unanticipated barriers may dominate.
Infant and maternal demographics
Fetal substance exposure by drug category