Clinical Bioethics
Category: Abstract Submission
Clinical Bioethics
609 - But My Baby…Parent Intuition and Periviable Birth Treatment Choice
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 609
Publication Number: 609.306
Publication Number: 609.306
Siobhan M. McDonnell, Medical College of Wisconsin, Germantown, WI, United States; Mir A. Basir, Medical College of Wisconsin, Wauwatosa, WI, United States; Ke Yan, Medical College of Wisconsin, Milwaukee, WI, United States; Melodee O. Liegl, Medical College of Wisconsin, Delafield, WI, United States; Paul D. Windschitl, University of Iowa, Iowa City, IA, United States
- SM
Siobhan M. McDonnell, MS (she/her/hers)
Clinical Research Assistant
Medical College of Wisconsin
Willmar, Minnesota, United States
Presenting Author(s)
Background: For periviable preterm birth, parents choose either neonatal intensive care (IC) or palliative care (PC) after receiving information on their baby’s chances of survival. In Kidszun et al. (2020), random presentation of a 30% or 60% chance of survival did not affect treatment choice. However, they used text rather than the recommended pictographs to convey survival information. Families, including neonatologists who had to choose a treatment as a parent, have reported that intuitive beliefs about their baby’s chances guided their decisions (Janvier et al., 2016).
Objective: Determine if a) 30% or 60% chance of survival, b) risk communication format, c) correct recall of chance of survival, or d) intuitive belief of their child’s chance of survival affects participant treatment choice.
Design/Methods: A vignette was presented in an internet survey to child-bearing aged women in the U.S. Information on neonatal chance of survival was presented in the context of periviable preterm birth. Participants were randomized to the chance of survival (30% or 60%) and risk communication format: text-only, static pictograph (Figure 1), or iterative pictograph (Figure 2). Iterative pictographs displayed 10 images of randomly shuffled icons to depict chances. Participants chose neonatal IC or PC and reported their recall and intuitive belief of their baby’s chance of survival. We collected information on religiosity, values, past NICU exposure, health literacy, and demographics. Fisher’s exact test and logistic regression were conducted.
Results: Of the 1,052 participants, 75% chose IC (Table 1). Treatment choice was not affected by 30% or 60% assigned chance of survival (p=0.48), risk communication format (p=0.80), or their interaction (p=0.18). Among the 463 (44%) participants who showed accurate recall, the assigned chance of survival did not affect treatment choice (p=0.91). Conversely, treatment choice was predicted by participants’ intuitive beliefs about their baby’s chances (p < 0.001). Intuitive beliefs did not differ by assigned chance of survival (p=0.98) or risk communication format (p=0.81). The chance of survival participants reported based on intuitive beliefs was greater than their recalled chance of survival (p < 0.001).Conclusion(s): Among women of child-bearing age who accurately recalled the chance of survival, intuitive beliefs about their own baby’s chances were more optimistic and predictive of treatment choice. Perinatal clinicians should recognize that optimistic treatment choices by parents does not necessarily indicate a lack of comprehension of presented outcome data.
Figure 1.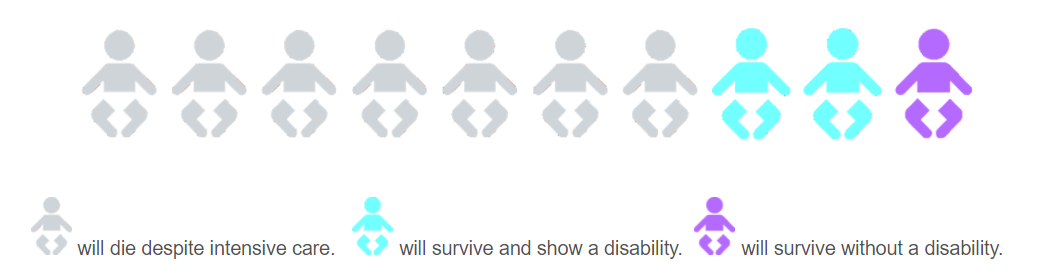 Example static pictograph displaying chance of survival and risk of disability in the group viewing a 30% chance of survival.
Example static pictograph displaying chance of survival and risk of disability in the group viewing a 30% chance of survival.
Figure 2.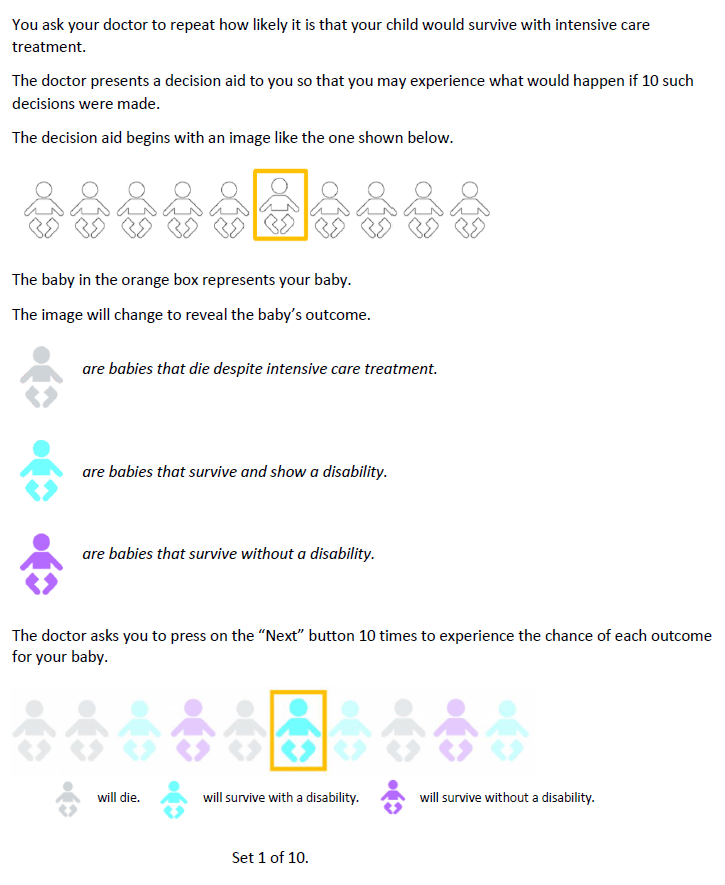 Example of survey pages describing and displaying the iterative pictograph to participants. The iterative pictograph helps participants experience the possible outcomes if 10 such decisions were made under similar conditions.
Example of survey pages describing and displaying the iterative pictograph to participants. The iterative pictograph helps participants experience the possible outcomes if 10 such decisions were made under similar conditions.
Objective: Determine if a) 30% or 60% chance of survival, b) risk communication format, c) correct recall of chance of survival, or d) intuitive belief of their child’s chance of survival affects participant treatment choice.
Design/Methods: A vignette was presented in an internet survey to child-bearing aged women in the U.S. Information on neonatal chance of survival was presented in the context of periviable preterm birth. Participants were randomized to the chance of survival (30% or 60%) and risk communication format: text-only, static pictograph (Figure 1), or iterative pictograph (Figure 2). Iterative pictographs displayed 10 images of randomly shuffled icons to depict chances. Participants chose neonatal IC or PC and reported their recall and intuitive belief of their baby’s chance of survival. We collected information on religiosity, values, past NICU exposure, health literacy, and demographics. Fisher’s exact test and logistic regression were conducted.
Results: Of the 1,052 participants, 75% chose IC (Table 1). Treatment choice was not affected by 30% or 60% assigned chance of survival (p=0.48), risk communication format (p=0.80), or their interaction (p=0.18). Among the 463 (44%) participants who showed accurate recall, the assigned chance of survival did not affect treatment choice (p=0.91). Conversely, treatment choice was predicted by participants’ intuitive beliefs about their baby’s chances (p < 0.001). Intuitive beliefs did not differ by assigned chance of survival (p=0.98) or risk communication format (p=0.81). The chance of survival participants reported based on intuitive beliefs was greater than their recalled chance of survival (p < 0.001).Conclusion(s): Among women of child-bearing age who accurately recalled the chance of survival, intuitive beliefs about their own baby’s chances were more optimistic and predictive of treatment choice. Perinatal clinicians should recognize that optimistic treatment choices by parents does not necessarily indicate a lack of comprehension of presented outcome data.
Figure 1.
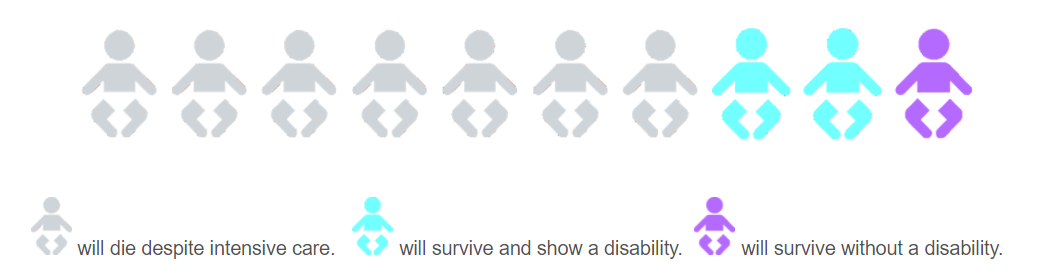 Example static pictograph displaying chance of survival and risk of disability in the group viewing a 30% chance of survival.
Example static pictograph displaying chance of survival and risk of disability in the group viewing a 30% chance of survival.Figure 2.
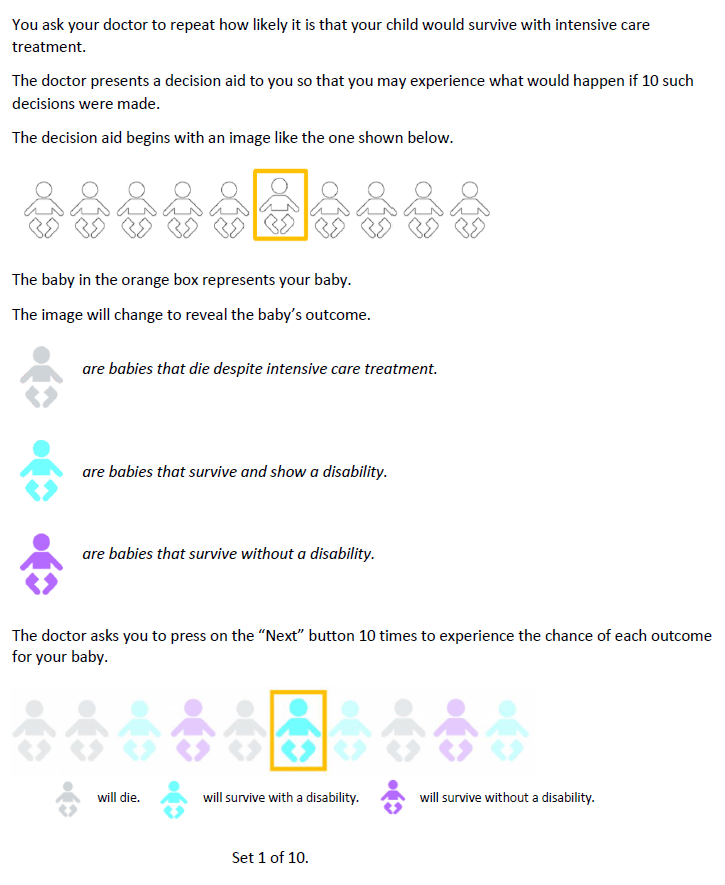 Example of survey pages describing and displaying the iterative pictograph to participants. The iterative pictograph helps participants experience the possible outcomes if 10 such decisions were made under similar conditions.
Example of survey pages describing and displaying the iterative pictograph to participants. The iterative pictograph helps participants experience the possible outcomes if 10 such decisions were made under similar conditions.