Breastfeeding/Human Milk
Category: Abstract Submission
Breastfeeding/Human Milk II
431 - In vivo measurement of breastmilk flow
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 431
Publication Number: 431.302
Publication Number: 431.302
Meredith Y. Kinoshita, Royal College of Surgeons Ireland, Dublin 6W, Dublin, Ireland; Helen Barry, Coroflo. Royal College of Surgeons Ireland (RCSI), Dublin, Dublin, Ireland; James Travers, Coroflo, Rush, Dublin, Ireland; Francesca Sorgini, Coroflo, Dublin, Dublin, Ireland; Anne O'Sullivan, Coombe Woman and Infants University Hospital, Dublin, Dublin, Ireland; Martin J. White, RCSI, Dublin, Dublin, Ireland; Michael J. Turner, UCD Centre for Human Reproduction, Dublin, FL, United States; Anne Doolan, Coombe Women and Infants Hospital, Dublin 8, Dublin, Ireland
- MK
Meredith Kinoshita, BMedSc, MB, BCh, BAO (Hons) (she/her/hers)
Specialist Registrar
The Coombe Hospital
Dublin, Dublin, Ireland
Presenting Author(s)
Background: During establishment of breastfeeding concern about feed sufficiency is common, but clinical assessment tools designed to measure milk transfer are unreliable. Accurate measurement of milk transfer may be clinically relevant in infants who are preterm, have congenital heart disease or are failing to thrive. Historically, breastmilk flow and volume have been measured using breast pumps over intervals of seconds with maximum flow rates of 0.9 ml/sec. The aim was to measure real time breastmilk flow and volume of milk transfer in breastfeeding infants by using a nipple shield with integrated flow sensor (Coroflo™).
Objective: Objectives were to measure flow rates and volumes transferred in vivo during breastfeeds. Flow rates, volumes, and duration of feeds were recorded in preterm and term breastfeeding dyads.
Design/Methods: The breastmilk flow sensor consists of a silicone nipple shield with an integrated microflow sensor (Figure 1). The flow sensor was selected for its’ reliability at flow rates from 0-1.5 ml/sec. Preterm and term mother-infant breastfeeding dyads were prospectively recruited. Each dyad used the device for at least one feed and test weights were performed to assess milk transfer. Flow rates, volumes, and duration of breastfeeds were measured by the sensor and sent via Bluetooth to a dedicated smartphone application. Breastmilk flow sensors were provided by Coroflo Ltd and are not classified as medical devices.
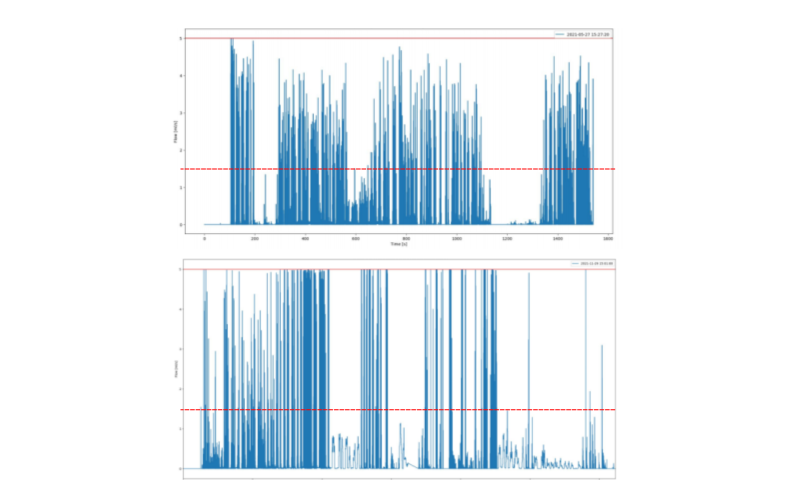
Results: 12 feeds were recorded from 4 preterm and 4 term dyads. 3.4% of flow rates recorded exceeded 1.5 ml/sec which is the upper limit of sensor reliability (Figure 2). All participants registered flows exceeding 5 ml/sec and above this threshold the sensor can not discriminate flow rates (Figure 3). Volumes measured by flow sensors were not similar to those from test weights (mean absolute difference 23.25 ml +/- 93) and at low flows, retrograde flow may have contributed to volume outputs. There was no significant difference between term and preterm infants in feed duration, volume or percent of flow rates exceeding sensor limits.Conclusion(s): Flow rates during breastfeeds were much higher than previously described. The current model demonstrates high flow rates when measured at the frequency of individual suction pulses. Flow rates frequently surpassed thresholds of sensor reliability and exceeded 5ml/sec for up to 10 msec, suggesting that much higher flows may be present but are indeterminable with this sensor. Measurement of actual flow rates during breastfeeding furthers understanding of milk transfer and provides a basis for future methods of breastfeeding assessment.
Figure 1. Coroflo breastfeeding monitor with components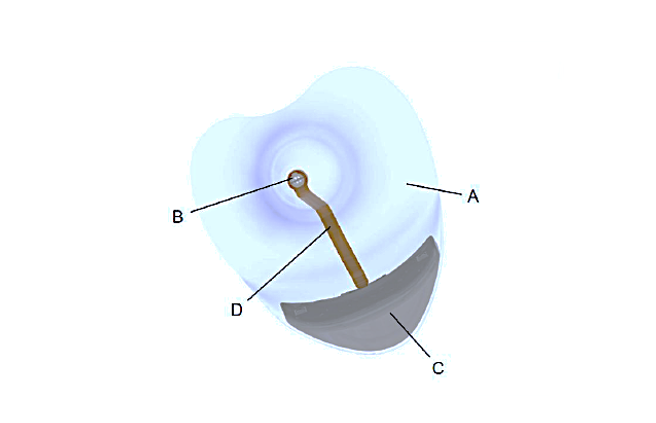 A) silicone nipple shield, B) sensing unit, C) electronic processing unit, D) flex cable.
A) silicone nipple shield, B) sensing unit, C) electronic processing unit, D) flex cable.
Figure 2. Flow rates frequently exceed limits of sensor accuracy in preterm (top) and term infants (bottom).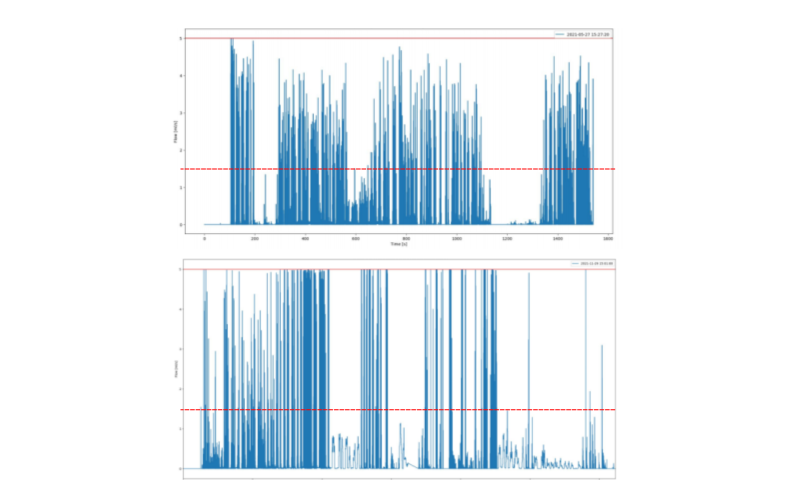
Objective: Objectives were to measure flow rates and volumes transferred in vivo during breastfeeds. Flow rates, volumes, and duration of feeds were recorded in preterm and term breastfeeding dyads.
Design/Methods: The breastmilk flow sensor consists of a silicone nipple shield with an integrated microflow sensor (Figure 1). The flow sensor was selected for its’ reliability at flow rates from 0-1.5 ml/sec. Preterm and term mother-infant breastfeeding dyads were prospectively recruited. Each dyad used the device for at least one feed and test weights were performed to assess milk transfer. Flow rates, volumes, and duration of breastfeeds were measured by the sensor and sent via Bluetooth to a dedicated smartphone application. Breastmilk flow sensors were provided by Coroflo Ltd and are not classified as medical devices.
Results: 12 feeds were recorded from 4 preterm and 4 term dyads. 3.4% of flow rates recorded exceeded 1.5 ml/sec which is the upper limit of sensor reliability (Figure 2). All participants registered flows exceeding 5 ml/sec and above this threshold the sensor can not discriminate flow rates (Figure 3). Volumes measured by flow sensors were not similar to those from test weights (mean absolute difference 23.25 ml +/- 93) and at low flows, retrograde flow may have contributed to volume outputs. There was no significant difference between term and preterm infants in feed duration, volume or percent of flow rates exceeding sensor limits.Conclusion(s): Flow rates during breastfeeds were much higher than previously described. The current model demonstrates high flow rates when measured at the frequency of individual suction pulses. Flow rates frequently surpassed thresholds of sensor reliability and exceeded 5ml/sec for up to 10 msec, suggesting that much higher flows may be present but are indeterminable with this sensor. Measurement of actual flow rates during breastfeeding furthers understanding of milk transfer and provides a basis for future methods of breastfeeding assessment.
Figure 1. Coroflo breastfeeding monitor with components
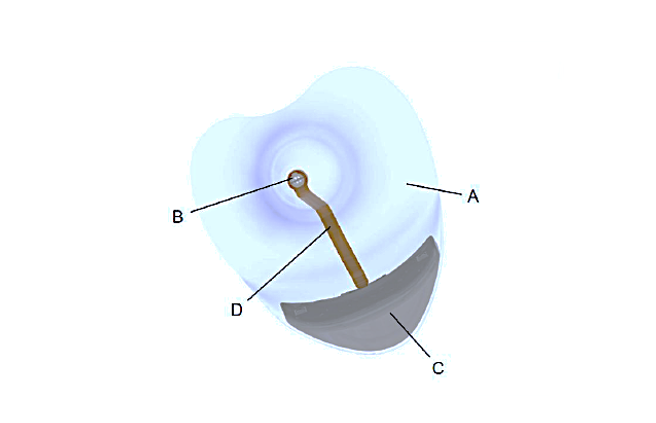 A) silicone nipple shield, B) sensing unit, C) electronic processing unit, D) flex cable.
A) silicone nipple shield, B) sensing unit, C) electronic processing unit, D) flex cable.Figure 2. Flow rates frequently exceed limits of sensor accuracy in preterm (top) and term infants (bottom).