Injury Prevention
Category: Abstract Submission
Injury Prevention I
124 - Long-term physical and mental health outcomes for firearm-injured children and adolescents
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 124
Publication Number: 124.329
Publication Number: 124.329
Maya Haasz, Children's Hospital Colorado, Aurora, CO, United States; Alexandria Dulchavsky, Children’s Hospital of Colorado, Denver, CO, United States; Jenny Stevens, Children's Hospital Colorado, Aurora, CO, United States; Margo M. Nolan, Children's Hospital Colorado, Denver, CO, United States; Jeannie Zuk, University of Colorado School of Medicine, Aurora, CO, United States; Jan Leonard, University of Colorado Anschutz Medical Campus, Aurora, CO, United States; Thomas Schroeppel, University of Colorado School of Medicine, Colorado Springs, CO, United States; Ryan Phillips, Ochsner Hospital for Children, New Orleans, LA, United States
- MH
Maya Haasz, MD (she/her/hers)
Assistant Professor
University of Colorado School of Medicine
Aurora, Colorado, United States
Presenting Author(s)
Background: Firearms (FAs) are a leading cause of injury among US youth. Though database studies suggest increased mental health (MH) diagnoses following FA injuries, there is little research describing the long-term physical and MH outcomes of survivors.
Objective: Assess long-term physical and MH outcomes among non-fatal FA vs. motor vehicle collision (MVC) injured victims and a standard population.
Design/Methods: We conducted a prospective matched cohort study (January-November 2021) of patients retrospectively identified from 4 pediatric trauma center registries. Eligible patients were English-speaking, injured after 2008 and ≥6 months prior to study start, < 18 years old at time of injury and ≥8 years old at time of study start. An attempt was made to contact all FA patients via telephone. FA patients who participated were matched 1:1 with MVC patients on ISS ( < 15 vs ≥ 15), age (+/- 1 year) and year of injury (exact). An investigator called eligible patients and conducted a structured interview of patients and parents including resource utilization questions and validated tools (Patient-Reported Outcomes Measurement Information System (PROMIS) measures, Children’s Impact of Event Scale (CRIES-8) for < 18 and parent-proxies). PROMIS scores are reported on a T-score metric (mean=50; SD=10); higher scores indicate more of the domain. We used paired T-tests to compare PROMIS and CRIES-8 scores between FA and MVC patients and one-sample t-tests to compare FA scores to the standard population.
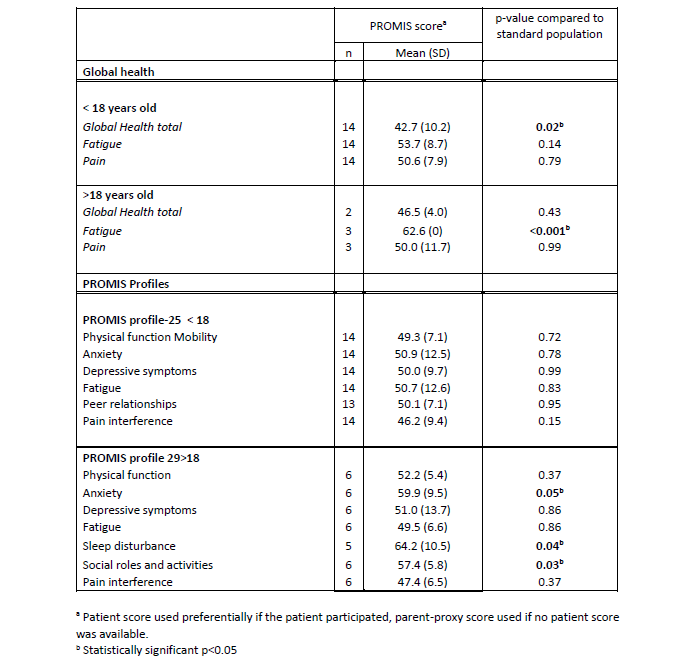
Results: Two hundred and sixty-one subjects were included. Of these, 112 patients were < 18 years old; of 32 (28.6%) parents reached in this group, 28 (87.5%) participated and all children reached (n=15) participated. Thirty of 149 patients >18 years old (20.1%) were reached and 22 (66.7%) participated; 9/10 parents reached participated. MVC vs FA injured groups had similar participation rates. PROMIS and CRIES-8 scores were similar between the two groups. Compared to a standard population, the >18 yo FA group had increased fatigue, anxiety, sleep disturbance, pain interference, and poorer social roles and activities; the < 18 yo group had poorer global health. Conclusion(s): Long term outcomes for FA patients are worse than a standard population in many domains but similar to MVC-injured patients, suggesting that injured youth experience worse physical and MH outcomes irrespective of mechanism of injury. True differences may have been missed due to a small sample size. Participation among those reached was high, supporting prospectively studying the long-term physical and MH outcomes of injured children.
Table 1: Long-term physical and mental health outcomes for firearm-injured children and adolescents compared to the general population as assessed by Patient-Reported Outcomes Measurement Information System (PROMIS) measures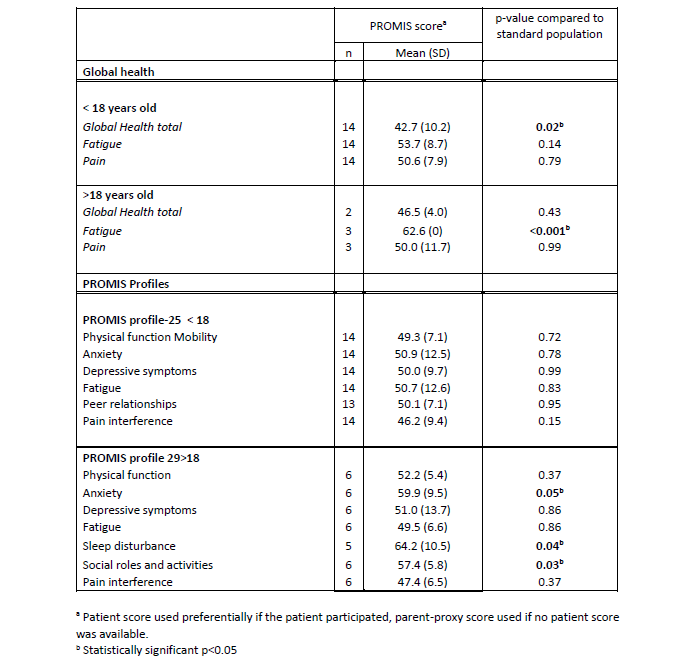
Objective: Assess long-term physical and MH outcomes among non-fatal FA vs. motor vehicle collision (MVC) injured victims and a standard population.
Design/Methods: We conducted a prospective matched cohort study (January-November 2021) of patients retrospectively identified from 4 pediatric trauma center registries. Eligible patients were English-speaking, injured after 2008 and ≥6 months prior to study start, < 18 years old at time of injury and ≥8 years old at time of study start. An attempt was made to contact all FA patients via telephone. FA patients who participated were matched 1:1 with MVC patients on ISS ( < 15 vs ≥ 15), age (+/- 1 year) and year of injury (exact). An investigator called eligible patients and conducted a structured interview of patients and parents including resource utilization questions and validated tools (Patient-Reported Outcomes Measurement Information System (PROMIS) measures, Children’s Impact of Event Scale (CRIES-8) for < 18 and parent-proxies). PROMIS scores are reported on a T-score metric (mean=50; SD=10); higher scores indicate more of the domain. We used paired T-tests to compare PROMIS and CRIES-8 scores between FA and MVC patients and one-sample t-tests to compare FA scores to the standard population.
Results: Two hundred and sixty-one subjects were included. Of these, 112 patients were < 18 years old; of 32 (28.6%) parents reached in this group, 28 (87.5%) participated and all children reached (n=15) participated. Thirty of 149 patients >18 years old (20.1%) were reached and 22 (66.7%) participated; 9/10 parents reached participated. MVC vs FA injured groups had similar participation rates. PROMIS and CRIES-8 scores were similar between the two groups. Compared to a standard population, the >18 yo FA group had increased fatigue, anxiety, sleep disturbance, pain interference, and poorer social roles and activities; the < 18 yo group had poorer global health. Conclusion(s): Long term outcomes for FA patients are worse than a standard population in many domains but similar to MVC-injured patients, suggesting that injured youth experience worse physical and MH outcomes irrespective of mechanism of injury. True differences may have been missed due to a small sample size. Participation among those reached was high, supporting prospectively studying the long-term physical and MH outcomes of injured children.
Table 1: Long-term physical and mental health outcomes for firearm-injured children and adolescents compared to the general population as assessed by Patient-Reported Outcomes Measurement Information System (PROMIS) measures