Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine XI
404 - Outcomes of Long vs Short Duration Pediatric Interfacility Transport
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 404
Publication Number: 404.315
Publication Number: 404.315
Brian Schultz, Children's Hospital of Colorado, Strasburg, CO, United States; George Burnet, University of Colorado School of Medicine, Colorado Springs, CO, United States; Sydney S. Tyler, University of Colorado Denver/Anschutz Medical Campus, Denver, CO, United States; Maria J. Mandt, Children's Hospital Colorado, Littleton, CO, United States

Brian Schultz, MD
Pediatric Critical Care Fellow
University of Colorado
Strasburg, Colorado, United States
Presenting Author(s)
Background: Rapid access to pediatric care is variable in the United States. Nearly 1/3 of the pediatric population lives greater than 50 miles from specialized pediatric resources and in the western United States this distance can routinely be over 300 miles. Guidelines and clinical acumen suggest that outcomes are worse as the time to definitive care increases. The literature exploring the relationship between these pediatric long duration interfacility transports and their outcomes is lacking.
Objective: To compare the outcomes of pediatric patients who undergo long duration interfacility transport (LDIFT) to those who experience short duration interfacility transport (SDIFT).
Design/Methods: This was a retrospective cohort study. Regional transport records were coalesced with the National EMS Information System (NEMSIS) to identify pediatric ( < 18yo) interfacility transports to a regional quaternary children’s hospital between Feb 2019-Feb 2020. Long-duration transportation was given an a-priori definition of ≥60 minutes for cohort comparisons. The primary outcome was 72-hour mortality. Secondary outcomes included length of stay, 30-day mortality, and indicators of escalation of care. Statistics including logistic regression were performed in R.
Results: Outcomes data was collected for 540 of the 6181 total interfacility transports during the study period with 117 LDIFTs and 423 SDIFTs. Patient demographics were similar between the two cohorts (Table 1). LDIFTs utilized less ground transport, had higher assigned EMS acuity and were more often directly admitted to an inpatient service as compared to SDIFTs. There was a high utilization rate of ICU services among both types of transport in the first 72 hours. Regarding outcomes (Table 2), mortality rate was similar at 72 hours (1.2% in SDIFTs, 1.7% in LDIFTs, p=0.648). 30-day mortality and mean LOS were not statistically different (p= 0.729 and p=0.152, respectively). Indicators of care escalation were generally similar (p=0.295). Univariate logistic regression showed a weak association between 72hr mortality and time at the patient bedside (OR 1.01 CI 1.00-1.03, p =0.02) (Table 3). Multivariate logistic regression models did not produce a statistically significant association between transport durations and outcomes of interest.Conclusion(s): When segregated by time to destination of 60 minutes, interfacility transports did not differ on the basis of 72-hour mortality, 30-day mortality or hospital LOS. Indicators of care escalation were also statistically insignificant. Future work remains to explore the complexities of transport times and outcomes.
CV-BMS.pdf
Table 2: Outcomes of Interfacility Transpors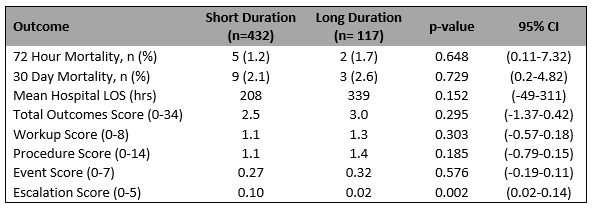 An abbreviated summary of the outcomes of interest for short and long duration interfacility transports. The outcomes scores represent numerical occurrences of indicators of escalation in care. Numeric comparisons were done with the Welch 2 Sample T-Test and categorical comparisons utilized the Fisher's Exact test. All significance levels were 95%.
An abbreviated summary of the outcomes of interest for short and long duration interfacility transports. The outcomes scores represent numerical occurrences of indicators of escalation in care. Numeric comparisons were done with the Welch 2 Sample T-Test and categorical comparisons utilized the Fisher's Exact test. All significance levels were 95%.
Objective: To compare the outcomes of pediatric patients who undergo long duration interfacility transport (LDIFT) to those who experience short duration interfacility transport (SDIFT).
Design/Methods: This was a retrospective cohort study. Regional transport records were coalesced with the National EMS Information System (NEMSIS) to identify pediatric ( < 18yo) interfacility transports to a regional quaternary children’s hospital between Feb 2019-Feb 2020. Long-duration transportation was given an a-priori definition of ≥60 minutes for cohort comparisons. The primary outcome was 72-hour mortality. Secondary outcomes included length of stay, 30-day mortality, and indicators of escalation of care. Statistics including logistic regression were performed in R.
Results: Outcomes data was collected for 540 of the 6181 total interfacility transports during the study period with 117 LDIFTs and 423 SDIFTs. Patient demographics were similar between the two cohorts (Table 1). LDIFTs utilized less ground transport, had higher assigned EMS acuity and were more often directly admitted to an inpatient service as compared to SDIFTs. There was a high utilization rate of ICU services among both types of transport in the first 72 hours. Regarding outcomes (Table 2), mortality rate was similar at 72 hours (1.2% in SDIFTs, 1.7% in LDIFTs, p=0.648). 30-day mortality and mean LOS were not statistically different (p= 0.729 and p=0.152, respectively). Indicators of care escalation were generally similar (p=0.295). Univariate logistic regression showed a weak association between 72hr mortality and time at the patient bedside (OR 1.01 CI 1.00-1.03, p =0.02) (Table 3). Multivariate logistic regression models did not produce a statistically significant association between transport durations and outcomes of interest.Conclusion(s): When segregated by time to destination of 60 minutes, interfacility transports did not differ on the basis of 72-hour mortality, 30-day mortality or hospital LOS. Indicators of care escalation were also statistically insignificant. Future work remains to explore the complexities of transport times and outcomes.
CV-BMS.pdf
Table 2: Outcomes of Interfacility Transpors
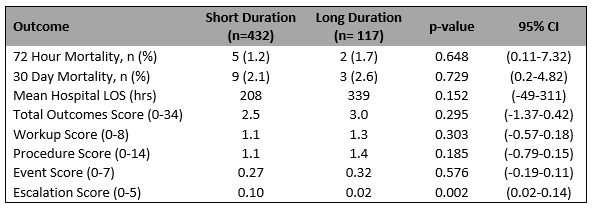 An abbreviated summary of the outcomes of interest for short and long duration interfacility transports. The outcomes scores represent numerical occurrences of indicators of escalation in care. Numeric comparisons were done with the Welch 2 Sample T-Test and categorical comparisons utilized the Fisher's Exact test. All significance levels were 95%.
An abbreviated summary of the outcomes of interest for short and long duration interfacility transports. The outcomes scores represent numerical occurrences of indicators of escalation in care. Numeric comparisons were done with the Welch 2 Sample T-Test and categorical comparisons utilized the Fisher's Exact test. All significance levels were 95%.