Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine VIII
359 - Pediatric Disaster Triage eModule for Evaluating and Improving Pediatric Triage Decisions
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 359
Publication Number: 359.313
Publication Number: 359.313
Dennis Ren, Children's National Hospital, Washington, DC, United States; Kristen A. Breslin, Children's National Hospital, Washington, DC, United States; Tress Goodwin, Children's National Hospital, Washington, DC, United States; Joelle Simpson, Children's National Health System, Washington, DC, United States
Dennis Ren, MD
Pediatric Emergency Medicine Fellow
Children's National Hospital
Washington, District of Columbia, United States
Presenting Author(s)
Background: Disaster triage requires a shift from usual standards of care and pediatric providers may not be familiar with the principles and practice of such triage. There is currently no standardized curriculum for disaster triage in pediatric training.
Objective: Evaluate and improve the accuracy of triage decisions using the Sort, Assess, Life-Saving Intervention, Treatment/Transport (SALT) triage system.
Design/Methods: We created a pediatric disaster triage eLearning module to evaluate and improve the accuracy of triage decisions using the Sort, Assess, Life-Saving Intervention, Treatment/Transport (SALT) triage system. The module included a didactic covering the concept of triage, the SALT algorithm, and pediatric limitations of triage systems. We recruited pediatric emergency medicine (PEM) attendings, PEM fellows, and pediatric residents at a tertiary-care pediatric hospital to evaluate the effectiveness of the curriculum.
The investigators created descriptions for 20 fictional patients that were used in a pre and post-test triage activity, including infants, medically complex patients, and technology-dependent patients. The investigators reached a consensus on the accurate triage level for each patient.
During the pre- and post-test activity, participants triaged these 20 patients to either green, yellow, red, or black categories. To simulate real-life scenarios, participants had an average of 20 seconds to designate a triage category for each patient. Participants had access to the SALT triage algorithm during both activities. Non-parametric tests were used to compare median percent accuracy between groups.
Results: There were 48 participants: 27 pediatric emergency medicine attendings (56%), 9 pediatric emergency medicine fellows (19%), 12 pediatric residents (25%). Approximately half reported previous experience with disaster triage. The median (interquartile range [IQR]) pretest percent accuracy across all participants was 75 (65, 85). Attendings scored higher than residents (80; 70, 90 compared to 62.5; 55, 68.8, p < 0.01) but not significantly higher than fellows (75; 67.5, 87.5). For the 44 participants who completed both the pre and post-test, median score significantly improved 75 (65, 85) to 80 (75, 90), p < 0.01.
Data collection is ongoing with plans to expand this offering.Conclusion(s): There is variation in accuracy of triage decisions amongst clinicians of different training levels.
Our module is a feasible method of delivering just-in-time triage training and improves accuracy of disaster triage decisions for pediatric patients.
Pre and Post Test Accuracy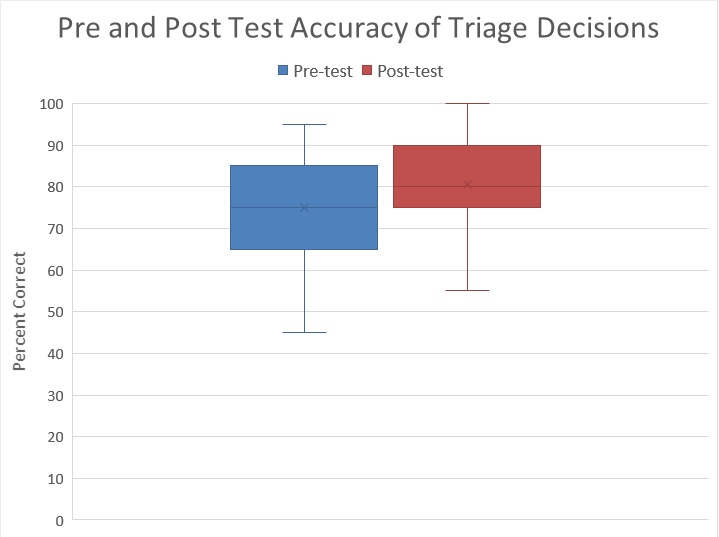 Pre- and post-test accuracy
Pre- and post-test accuracy
Accuracy of Triage Decisions by Training Level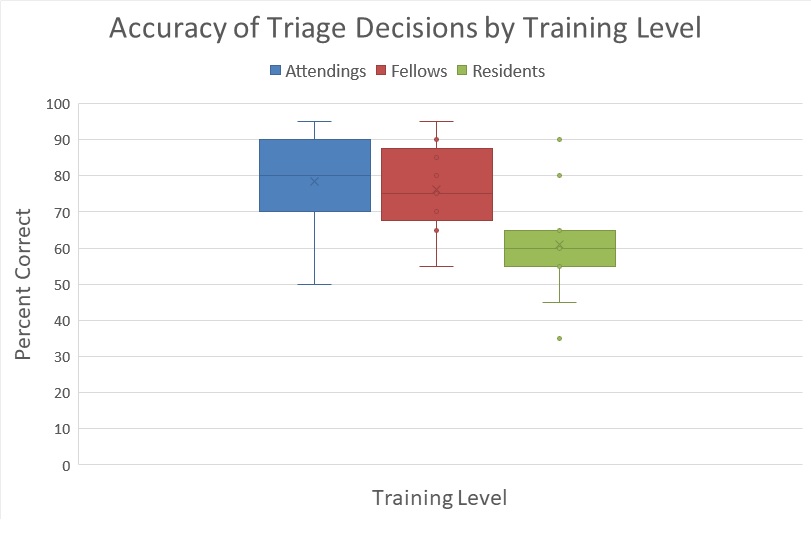 Variation in accuracy of pre-test scores amongst attendings, fellows, and residents.
Variation in accuracy of pre-test scores amongst attendings, fellows, and residents.
Objective: Evaluate and improve the accuracy of triage decisions using the Sort, Assess, Life-Saving Intervention, Treatment/Transport (SALT) triage system.
Design/Methods: We created a pediatric disaster triage eLearning module to evaluate and improve the accuracy of triage decisions using the Sort, Assess, Life-Saving Intervention, Treatment/Transport (SALT) triage system. The module included a didactic covering the concept of triage, the SALT algorithm, and pediatric limitations of triage systems. We recruited pediatric emergency medicine (PEM) attendings, PEM fellows, and pediatric residents at a tertiary-care pediatric hospital to evaluate the effectiveness of the curriculum.
The investigators created descriptions for 20 fictional patients that were used in a pre and post-test triage activity, including infants, medically complex patients, and technology-dependent patients. The investigators reached a consensus on the accurate triage level for each patient.
During the pre- and post-test activity, participants triaged these 20 patients to either green, yellow, red, or black categories. To simulate real-life scenarios, participants had an average of 20 seconds to designate a triage category for each patient. Participants had access to the SALT triage algorithm during both activities. Non-parametric tests were used to compare median percent accuracy between groups.
Results: There were 48 participants: 27 pediatric emergency medicine attendings (56%), 9 pediatric emergency medicine fellows (19%), 12 pediatric residents (25%). Approximately half reported previous experience with disaster triage. The median (interquartile range [IQR]) pretest percent accuracy across all participants was 75 (65, 85). Attendings scored higher than residents (80; 70, 90 compared to 62.5; 55, 68.8, p < 0.01) but not significantly higher than fellows (75; 67.5, 87.5). For the 44 participants who completed both the pre and post-test, median score significantly improved 75 (65, 85) to 80 (75, 90), p < 0.01.
Data collection is ongoing with plans to expand this offering.Conclusion(s): There is variation in accuracy of triage decisions amongst clinicians of different training levels.
Our module is a feasible method of delivering just-in-time triage training and improves accuracy of disaster triage decisions for pediatric patients.
Pre and Post Test Accuracy
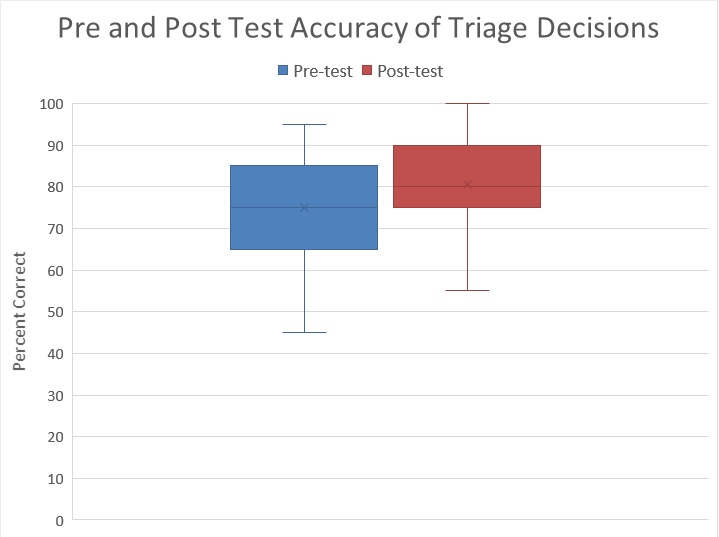 Pre- and post-test accuracy
Pre- and post-test accuracyAccuracy of Triage Decisions by Training Level
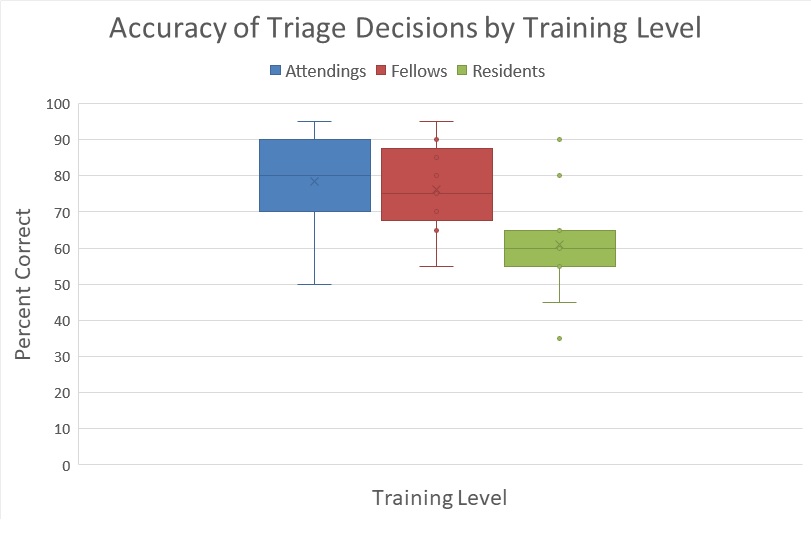 Variation in accuracy of pre-test scores amongst attendings, fellows, and residents.
Variation in accuracy of pre-test scores amongst attendings, fellows, and residents.