Medical Education: Resident
Category: Abstract Submission
Medical Education 10 - Medical Education: Resident III
259 - Pediatric Hocus “POCUS:" Point-of-Care Ultrasound Technique and Interpretation for Pediatric Resident Education
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 259
Publication Number: 259.330
Publication Number: 259.330
Mark J. Occhionero, Janet Weis Children's Hospital at Geisinger, Danville, PA, United States; Kristin Huynh, Geisinger Commonwealth School of Medicine, Danville, PA, United States; Lee Morris, Michigan State University College of Human Medicine, Grand Rapids, MI, United States

Mark J. Occhionero, MD
Resident Physician
Janet Weis Children's Hospital at Geisinger
Danville, Pennsylvania, United States
Presenting Author(s)
Background: The use of Point-of-care ultrasound (POCUS) is on the rise as a clinician-performed modality used to augment history-taking and physical examination skills. A great amount of literature is documented within other medical fields, but Pediatrics only recently started to adopt these concepts into practice. The American Academy of Pediatrics endorses POCUS for pediatric emergency medicine; however, no standard guidelines have been established for the specialty. Furthermore, few pediatric residency programs have started developing curricula for their residents with regards to POCUS knowledge and skills.
Objective: Our aim was to improve pediatric resident knowledge of POCUS through the development of standardized education, practical application, and testing with the goal of setting a foundation for pediatric bedside ultrasound in a large medical center.
Design/Methods: Our resident-organized POCUS interest group developed knowledge and skills sessions for a pediatric curriculum. Eighteen residents were recruited for a pilot POCUS curriculum. The residents completed a comprehensive examination prior to the course onset. Sessions were delivered over an eight-month period focusing on our six designated core competencies including: 1) ultrasound fundamentals, 2) extended focused assessment with sonography for trauma (e-FAST), 3) cardiac, 4) pulmonary, 5) gastrointestinal and genitourinary, and 6) vascular and musculoskeletal POCUS. Residents were tested on each topic presented during the session and repeat testing was conducted upon session completion. At the conclusion of the course, residents took the same examination used as a pretest, and comprehensive examination was completed at one- and three-months post course to measure retention.
Results: Following our eight-month course, twelve residents completed the course and demonstrated an overall improvement of 21% across our six designated core competencies. A paired t-test was performed demonstrating statistical significance of our post-course testing with a p-value of 0.00032. There was an insufficient sample size at one and three month testing for subsequent statistical analysis.
Conclusion(s): Our residents demonstrated significant improvement in POCUS knowledge. There were several limitations to our study including sample size, equipment resourcing, curriculum format, and generalizability to other pediatric residency programs. A strength of our curriculum was that our course provided introductory POCUS knowledge. Future iterations will focus on the assessment of skills-based competency, along with refinement of the knowledge-based curricula.
Figure 1: Average Resident Improvement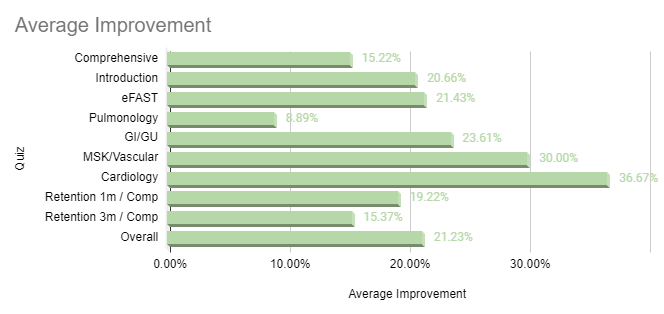 Evaluation was performed both prior to, and at the completion of each session. The difference of each session was calculated as demonstrated on this table. Overall and retention averages were also calculated as shown, with overall improvement of 21%.
Evaluation was performed both prior to, and at the completion of each session. The difference of each session was calculated as demonstrated on this table. Overall and retention averages were also calculated as shown, with overall improvement of 21%.
Objective: Our aim was to improve pediatric resident knowledge of POCUS through the development of standardized education, practical application, and testing with the goal of setting a foundation for pediatric bedside ultrasound in a large medical center.
Design/Methods: Our resident-organized POCUS interest group developed knowledge and skills sessions for a pediatric curriculum. Eighteen residents were recruited for a pilot POCUS curriculum. The residents completed a comprehensive examination prior to the course onset. Sessions were delivered over an eight-month period focusing on our six designated core competencies including: 1) ultrasound fundamentals, 2) extended focused assessment with sonography for trauma (e-FAST), 3) cardiac, 4) pulmonary, 5) gastrointestinal and genitourinary, and 6) vascular and musculoskeletal POCUS. Residents were tested on each topic presented during the session and repeat testing was conducted upon session completion. At the conclusion of the course, residents took the same examination used as a pretest, and comprehensive examination was completed at one- and three-months post course to measure retention.
Results: Following our eight-month course, twelve residents completed the course and demonstrated an overall improvement of 21% across our six designated core competencies. A paired t-test was performed demonstrating statistical significance of our post-course testing with a p-value of 0.00032. There was an insufficient sample size at one and three month testing for subsequent statistical analysis.
Conclusion(s): Our residents demonstrated significant improvement in POCUS knowledge. There were several limitations to our study including sample size, equipment resourcing, curriculum format, and generalizability to other pediatric residency programs. A strength of our curriculum was that our course provided introductory POCUS knowledge. Future iterations will focus on the assessment of skills-based competency, along with refinement of the knowledge-based curricula.
Figure 1: Average Resident Improvement
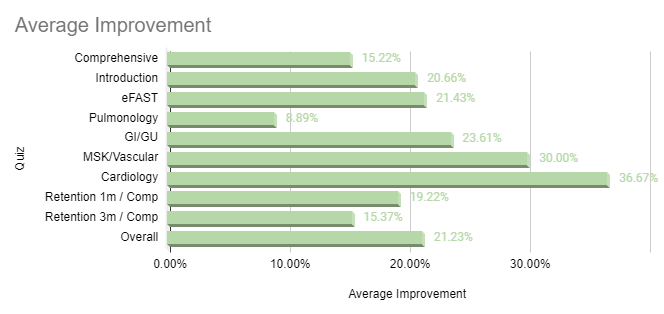 Evaluation was performed both prior to, and at the completion of each session. The difference of each session was calculated as demonstrated on this table. Overall and retention averages were also calculated as shown, with overall improvement of 21%.
Evaluation was performed both prior to, and at the completion of each session. The difference of each session was calculated as demonstrated on this table. Overall and retention averages were also calculated as shown, with overall improvement of 21%.