Hospital Medicine: Clinical
Category: Abstract Submission
Hospital Medicine: Education/Research/QI Potpourri
318 - Pediatric Intermediate Care Units: Composition, Staffing and Interventions
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 318
Publication Number: 318.322
Publication Number: 318.322
Debra F. Hillier, Boston Children's Hospital, Winchester, MA, United States; Daniel Kelly, Boston Children's Hospital, Boston, MA, United States; Alla Smith, Boston Children's Hospital, Boston, MA, United States; Rebecca Eige, Boston Children's Hospital, Brookline, MA, United States; Alison J. Kan, Boston Children's Hospital, Westbury, NY, United States; Sithya Lach, Boston Children's Hospital, Boston, MA, United States; Susan S. Stone, Boston Children's Hospital, Boston, MA, United States; Christiana M. Russ, Boston Children's Hospital, Boston, MA, United States

Debra F. Hillier, MD, MS-HPEd
Assistant Professor of Pediatrics
Boston Children's Hospital
Winchester, Massachusetts, United States
Presenting Author(s)
Background: Pediatric Intermediate Care Units (PIMCUs) have cared for high acuity pediatric patients for over three decades. Given diversity in PIMCU constructs, it remains uncertain if variation in staff training and administrative structure influences interventions supported in individual units.
Objective: This study aimed to 1) describe characteristics of general medical or medical-surgical PIMCUs in children’s hospitals across the US and Canada, and 2) compare characteristics of PIMCUs staffed by critical care-trained clinicians with those staffed by non-critical care trained clinicians.
Design/Methods: A 29-question survey was administered in 2021 to directors of PIMCUs identified by contacting acute care hospitals in the Children’s Hospital Association (CHA) registry; units specific to single subspecialties were excluded. Data were de-identified and analyzed in aggregate. PIMCU characteristics, including staff ratios, staff training, leadership structure, and clinical interventions were evaluated using frequencies with associated percentages within each response item, when applicable.
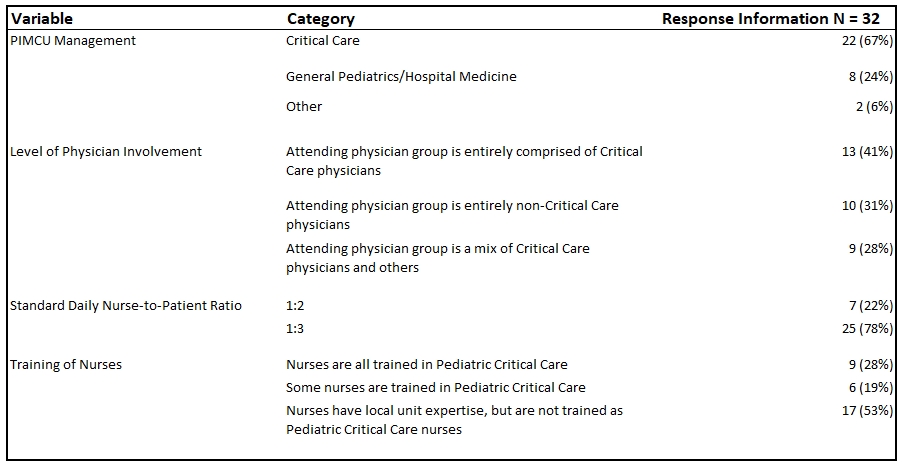
Results: 173 out of 195 CHA hospitals queried for presence of a PIMCU responded; 46 of that 173 had a PIMCU that met study criteria. Of those 46 sites, 32 completed a survey describing PIMCU characteristics. The most common interventions offered were high-flow nasal cannula (88%); apnea monitoring (84%); and stable, chronic non-invasive ventilation (75%). The least common interventions offered were vasopressors (16%), arterial lines (16%), and acute renal replacement therapy (9%). Of the PIMCUs analyzed, 66% were managed under a Division of Critical Care, 25% under Pediatric Hospital Medicine, and 6% by other groups. Overall, 41% of units were staffed solely by critical care physicians, 31% by non-critical care providers, and 28% by a combination of the two. About half of the units had some or all critical care trained nursing staff; a majority (78%) had a 1:3 nursing ratio. There were no clear patterns of unit traits based on critical care versus other training backgrounds of staff or leadership.Conclusion(s): Responsibilities of caring for pediatric intermediate level patients are shared between pediatric critical care and non-critical care physicians and nurses. More studies are needed to determine how structure and staff training in intermediate care units can optimize outcomes and which patients best benefit from this level of care.
PIMCU Interventions.jpg) Frequency of Interventions offered in PIMCUs Participating in Study
Frequency of Interventions offered in PIMCUs Participating in Study
PIMCU Staffing Characteristics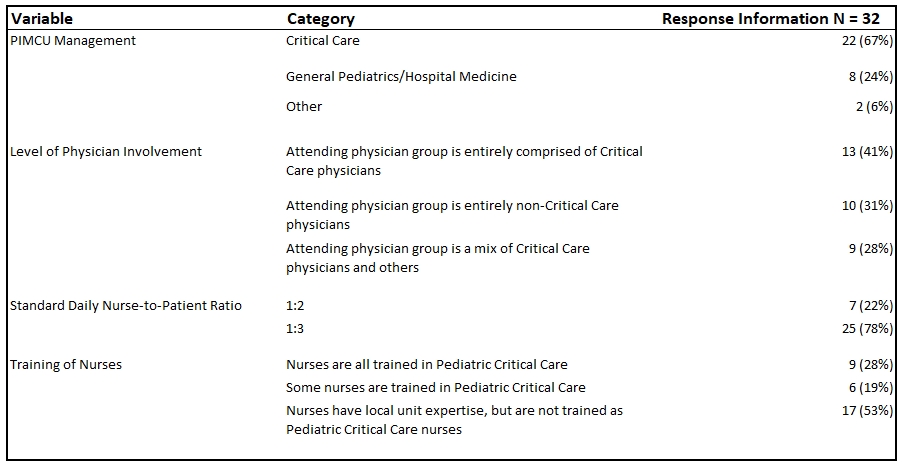 Profiles of Staff Training, Nurse Ratios, and Leadership in 32 PMICUs
Profiles of Staff Training, Nurse Ratios, and Leadership in 32 PMICUs
Objective: This study aimed to 1) describe characteristics of general medical or medical-surgical PIMCUs in children’s hospitals across the US and Canada, and 2) compare characteristics of PIMCUs staffed by critical care-trained clinicians with those staffed by non-critical care trained clinicians.
Design/Methods: A 29-question survey was administered in 2021 to directors of PIMCUs identified by contacting acute care hospitals in the Children’s Hospital Association (CHA) registry; units specific to single subspecialties were excluded. Data were de-identified and analyzed in aggregate. PIMCU characteristics, including staff ratios, staff training, leadership structure, and clinical interventions were evaluated using frequencies with associated percentages within each response item, when applicable.
Results: 173 out of 195 CHA hospitals queried for presence of a PIMCU responded; 46 of that 173 had a PIMCU that met study criteria. Of those 46 sites, 32 completed a survey describing PIMCU characteristics. The most common interventions offered were high-flow nasal cannula (88%); apnea monitoring (84%); and stable, chronic non-invasive ventilation (75%). The least common interventions offered were vasopressors (16%), arterial lines (16%), and acute renal replacement therapy (9%). Of the PIMCUs analyzed, 66% were managed under a Division of Critical Care, 25% under Pediatric Hospital Medicine, and 6% by other groups. Overall, 41% of units were staffed solely by critical care physicians, 31% by non-critical care providers, and 28% by a combination of the two. About half of the units had some or all critical care trained nursing staff; a majority (78%) had a 1:3 nursing ratio. There were no clear patterns of unit traits based on critical care versus other training backgrounds of staff or leadership.Conclusion(s): Responsibilities of caring for pediatric intermediate level patients are shared between pediatric critical care and non-critical care physicians and nurses. More studies are needed to determine how structure and staff training in intermediate care units can optimize outcomes and which patients best benefit from this level of care.
PIMCU Interventions
.jpg) Frequency of Interventions offered in PIMCUs Participating in Study
Frequency of Interventions offered in PIMCUs Participating in StudyPIMCU Staffing Characteristics
 Profiles of Staff Training, Nurse Ratios, and Leadership in 32 PMICUs
Profiles of Staff Training, Nurse Ratios, and Leadership in 32 PMICUs