Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine X
388 - Predictors of Adequate Post-Intubation Sedation in a Pediatric Emergency Department
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 388
Publication Number: 388.314
Publication Number: 388.314
Barron Frazier, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Amelia Wong, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, United States; Christopher Daly, Medical University of South Carolina, Charleston, SC, United States; Matthew J. Root, Monroe Carell Jr. Children's Hospital at Vanderbilt, Downer's Grove, IL, United States; Kristina A. Betters, Vanderbilt Univeristy, Nashville, TN, United States; Holly Hanson, Vanderbilt University School of Medicine, Nashville, TN, United States

Barron Frazier, MD (he/him/his)
Assistant Professor of Pediatrics
Monroe Carell Jr. Children's Hospital at Vanderbilt
Nashville, Tennessee, United States
Presenting Author(s)
Background: Post-intubation sedation (PIS) is critical in managing and stabilizing intubated patients. Inadequate sedation can lead to unrecognized pain, early extubation with the potential for an additional critical procedure, and have an impact of hemodynamic stability. Adult literature has shown that only 50% of patients who are intubated in the emergency department (ED) receive adequate sedation. Less is known regarding adequacy of PIS in pediatric EDs and related outcomes.
Objective: To determine predictors of adequate PIS in the pediatric ED and, secondarily, the impact of the adequacy of PIS on patient outcomes.
Design/Methods: A retrospective cohort study was performed on patients who were intubated in the pediatric ED, at a tertiary care children’s hospital, from 12/2017-03/2020. Adequate PIS was defined as the initiation of PIS prior to the loss of the therapeutic effect of the rapid sequence intubation sedative based on pharmacologic duration of action published by Microdex. Patient-specific variables included patient demographics, reason for intubation, time of day, sedative and paralytic used for rapid sequence intubation (RSI), intubation difficulty, and hypotension. Patient outcomes included the duration of mechanical ventilation (MV), intensive care unit (ICU) length of stay, and total hospital length of stay. Logistic regression was performed and adjusted for covariates of age, sex, race, ethnicity, payor, and a pediatric mortality index, PIM-2, to assess the relationship between patient-specific variables and adequate sedation.
Results: 150 subjects were reviewed, 99 had no missing data and were used for analysis. 25 (25%) subjects received adequate PIS. 2 (2%) patients had unplanned extubations in the ED. There were no associations between adequate PIS and patient age, RSI sedative or paralytic, presence of hypotension, or intubation difficulty (Table 1). There was an appreciated difference in adequate PIS sedation between subjects who received succinylcholine (40%) versus rocuronium (22%), but when adjusting for covariates, it was not statistically significant (p=0.205). Long term outcomes were not affected by PIS (Table 2).Conclusion(s): Similar to adult studies, our study found that 75% of pediatric patients intubated in the ED did not receive adequate PIS. There were no patient-specific factors that were associated with a subject being more likely to received PIS. Despite this poor performance in PIS, there was no change to length of stay or overall survivability. Future research should focus on barriers to PIS and use quality improvement work to improve process performance.
Table 1. Patient Variables Associated with Adequate PIS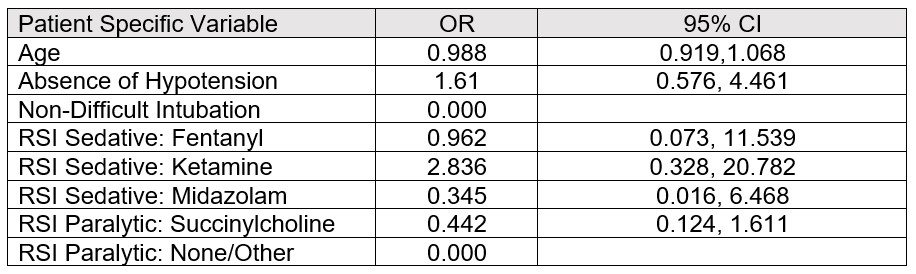
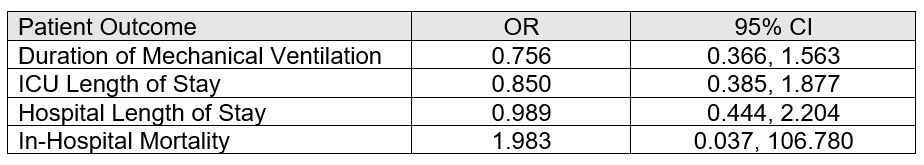
Table 2. Association Between Patient Outcomes and Adequate PIS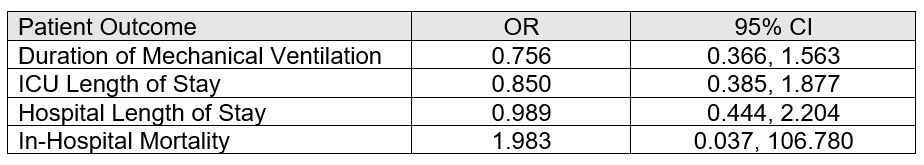
Objective: To determine predictors of adequate PIS in the pediatric ED and, secondarily, the impact of the adequacy of PIS on patient outcomes.
Design/Methods: A retrospective cohort study was performed on patients who were intubated in the pediatric ED, at a tertiary care children’s hospital, from 12/2017-03/2020. Adequate PIS was defined as the initiation of PIS prior to the loss of the therapeutic effect of the rapid sequence intubation sedative based on pharmacologic duration of action published by Microdex. Patient-specific variables included patient demographics, reason for intubation, time of day, sedative and paralytic used for rapid sequence intubation (RSI), intubation difficulty, and hypotension. Patient outcomes included the duration of mechanical ventilation (MV), intensive care unit (ICU) length of stay, and total hospital length of stay. Logistic regression was performed and adjusted for covariates of age, sex, race, ethnicity, payor, and a pediatric mortality index, PIM-2, to assess the relationship between patient-specific variables and adequate sedation.
Results: 150 subjects were reviewed, 99 had no missing data and were used for analysis. 25 (25%) subjects received adequate PIS. 2 (2%) patients had unplanned extubations in the ED. There were no associations between adequate PIS and patient age, RSI sedative or paralytic, presence of hypotension, or intubation difficulty (Table 1). There was an appreciated difference in adequate PIS sedation between subjects who received succinylcholine (40%) versus rocuronium (22%), but when adjusting for covariates, it was not statistically significant (p=0.205). Long term outcomes were not affected by PIS (Table 2).Conclusion(s): Similar to adult studies, our study found that 75% of pediatric patients intubated in the ED did not receive adequate PIS. There were no patient-specific factors that were associated with a subject being more likely to received PIS. Despite this poor performance in PIS, there was no change to length of stay or overall survivability. Future research should focus on barriers to PIS and use quality improvement work to improve process performance.
Table 1. Patient Variables Associated with Adequate PIS
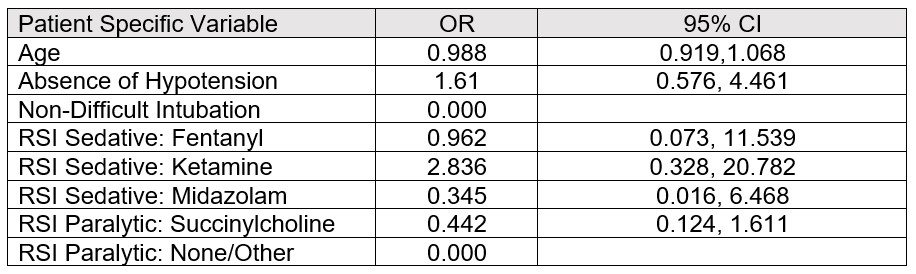
Table 2. Association Between Patient Outcomes and Adequate PIS