Medical Education: Fellow
Category: Abstract Submission
Medical Education 8 - Medical Education: Fellow II
234 - RAPID-FIRE: Recognition, Activation and Prevention of In hospital Deterioration: Forming Interprofessional Readiness for Escalation
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 234
Publication Number: 234.332
Publication Number: 234.332
Lauren E. Castaneda, Children's Hospital Colorado, Denver, CO, United States; Justin M. Lockwood, University of Colorado School of Medicine, Aurora, CO, United States; Laura G. Bricklin, University of Colorado School of Medicine, Denver, CO, United States; Leanne Adamson, Children's Hospital Colorado, Aurora, CO, United States; Beth Wathen, Children's Hospital Colorado, DENVER, CO, United States; Angela S. Czaja, University of Colorado School of Medicine, Aurora, CO, United States

Lauren E. Castaneda, MD
Critical Care Fellow
Children's Hospital Colorado
Denver, Colorado, United States
Presenting Author(s)
Background: Pediatric in-hospital cardiac arrest carries significant morbidity and mortality, but often has preceding early signs of deterioration. Early recognition and care escalation may improve patient outcomes but require interprofessional (IP) collaboration. Previously identified barriers to care escalation at our quaternary care hospital included variable knowledge and training by care role, ineffective communication and hierarchical influences. IP education can mitigate these barriers but is infrequent.
Objective: To implement an IP curriculum using just-in-time (JIT) strategies in a situated learning approach focused on care escalation in the acutely hospitalized patient.
Design/Methods: An educational intervention using JIT & situated learning focused on care escalation in the non-ICU setting was developed by an IP team. Targeted learners were team members (nurses, pediatric residents, advanced practice providers) actively caring for hospitalized patients. Participants were invited to join a 10-minute escalation of care exercise while on-shift. Team members identified shared patients admitted to the acute care service at highest risk of deterioration and discussed IP communication and patient care strategies with facilitator guidance. Primary outcomes included self-efficacy in patient care, IP communication and perceptions of IP collaboration measured via post session electronic survey.
Results: 12 sessions were conducted between Sept-Dec 2021 with 23 team members (12 nurses, 1 APP, 10 residents). Effective on-shift recruitment required consideration of increased care team workload due to high patient census and unique team member strains. All respondents agreed or strongly agreed that using real patient scenarios improved realism and comfort with management of at-risk patients. Only 61% felt the exercise reinforced team-based communication & there continued to be less comfort communicating concerns to attendings or ICU teams. However, 96% found the exercise a worthwhile use of on-shift time and all participants agreed or strongly agreed that presence of other care team members was a positive contributor to learning.Conclusion(s): IP education exercises using real patient data improve perceived readiness for escalation of care and enhance collaborative learning. Successful implementation requires consideration of care team member workflow unique to each role for meaningful participation. IP education may improve team-based communication, though hierarchical influences remain.
Lauren Castaneda CVCastanedaCV2021.pdf
Figure 2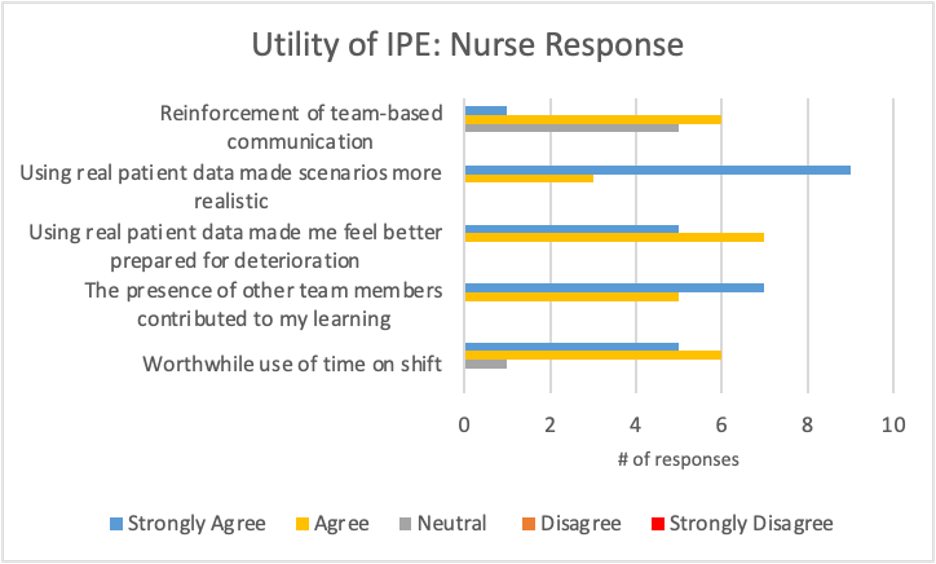 RN perceived utility of IP escalation exercise
RN perceived utility of IP escalation exercise
Objective: To implement an IP curriculum using just-in-time (JIT) strategies in a situated learning approach focused on care escalation in the acutely hospitalized patient.
Design/Methods: An educational intervention using JIT & situated learning focused on care escalation in the non-ICU setting was developed by an IP team. Targeted learners were team members (nurses, pediatric residents, advanced practice providers) actively caring for hospitalized patients. Participants were invited to join a 10-minute escalation of care exercise while on-shift. Team members identified shared patients admitted to the acute care service at highest risk of deterioration and discussed IP communication and patient care strategies with facilitator guidance. Primary outcomes included self-efficacy in patient care, IP communication and perceptions of IP collaboration measured via post session electronic survey.
Results: 12 sessions were conducted between Sept-Dec 2021 with 23 team members (12 nurses, 1 APP, 10 residents). Effective on-shift recruitment required consideration of increased care team workload due to high patient census and unique team member strains. All respondents agreed or strongly agreed that using real patient scenarios improved realism and comfort with management of at-risk patients. Only 61% felt the exercise reinforced team-based communication & there continued to be less comfort communicating concerns to attendings or ICU teams. However, 96% found the exercise a worthwhile use of on-shift time and all participants agreed or strongly agreed that presence of other care team members was a positive contributor to learning.Conclusion(s): IP education exercises using real patient data improve perceived readiness for escalation of care and enhance collaborative learning. Successful implementation requires consideration of care team member workflow unique to each role for meaningful participation. IP education may improve team-based communication, though hierarchical influences remain.
Lauren Castaneda CVCastanedaCV2021.pdf
Figure 2
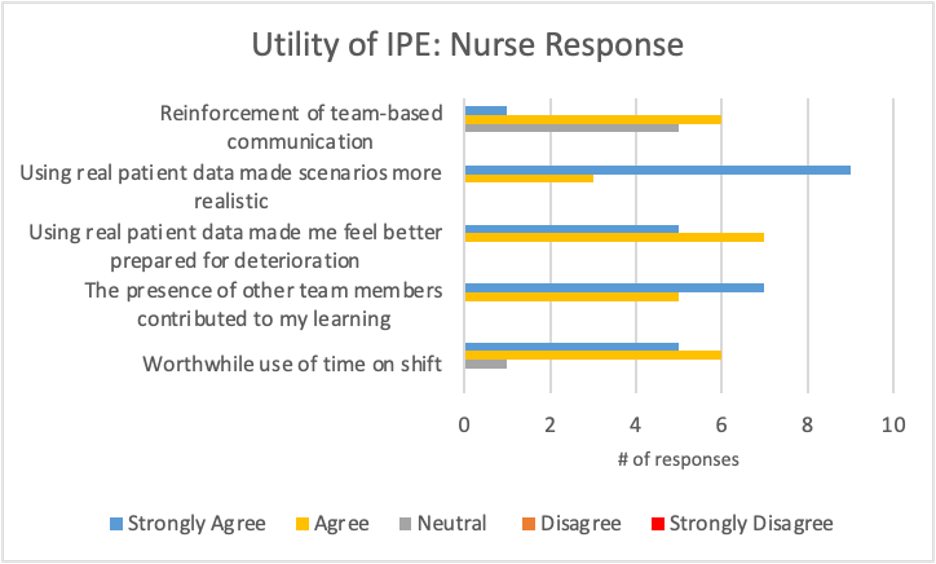 RN perceived utility of IP escalation exercise
RN perceived utility of IP escalation exercise