Hospital Medicine: Education
Category: Abstract Submission
Hospital Medicine: Education/Research/QI Potpourri
319 - Resident Independent Rounds: Attending Physician Perspective
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 319
Publication Number: 319.322
Publication Number: 319.322
Peggy Guo, University of Colorado School of Medicine, Colorado Springs, CO, United States; Barry Seltz, University of Colorado School of Medicine, Denver, CO, United States; Sonja I. Ziniel, University of Colorado School of Medicine, Aurora, CO, United States

Peggy Guo, MD
Assistant Professor
University of Colorado School of Medicine
Colorado Springs, Colorado, United States
Presenting Author(s)
Background: Post-graduate clinical education aims to provide pediatric residents with opportunities to practice autonomously in preparation for independent practice. Resident independent round (RIR) is an educational model where the inpatient team conducts family-centered rounds without the attending physician.
Objective: This study focused on the attending physician perspectives which have not been well described in published literature.
Design/Methods: In July 2020, we implemented weekly standardized RIR on pediatric hospital medicine services at our institution. A REDCap survey was developed for attending physicians and fellows on service. The survey focused on the impact of RIR on the plan of care, teaching, learner assessment, efficiency, and patient safety compared to traditional rounds. Surveys were sent to physicians at the end of each service week from October 2020 through May 2021. Statistical analysis focused on descriptive statistics and bivariate analyses accounting for clustering of surveys by physicians using design-based Pearson Chi-Square tests. Two investigators performed content analysis of answers to open-ended questions.
Results: Twenty-eight physicians (26 faculty, 2 fellows) completed 44/54 survey requests (81% response rate). Most physicians reported RIR had no impact on number of medical errors or safety events (98%), and no or positive impact on developmental of a clear plan of care (89%), family’s understanding of plan of care (89%), or learner assessment outside of rounds (84%). In addition, 59% reported that RIR positively impacted the amount of time physicians have for other tasks for that day. However, most reported decreased opportunities to teach (64%) and assess (80%) learners during rounds for the week. Bivariate analysis of the data based on years of physician experience and weeks on service did not find any significant differences.
Qualitative data analysis found that RIRs were successful in promoting resident autonomy and satisfaction. Seeing patients on their own, attending physicians valued the time to connect with families, but reported decreased opportunities for teaching and role modeling. Losing a day of direct observation of family-centered rounds also limited their ability to assess learners. Some expressed challenges with care coordination and team communication for new or complex patients.Conclusion(s): Attending physicians felt RIR enhanced resident autonomy and they enjoyed the opportunities to connect with families. Further work is needed to mitigate the challenges with learner assessment and care coordination for some patients.
Figure 1: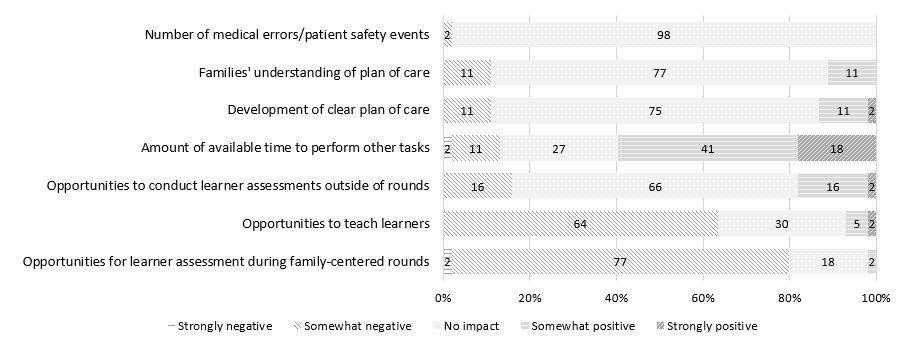 Attending Physicians’ Perspectives Regarding the Impact of Resident-Independent Rounds
Attending Physicians’ Perspectives Regarding the Impact of Resident-Independent Rounds
Objective: This study focused on the attending physician perspectives which have not been well described in published literature.
Design/Methods: In July 2020, we implemented weekly standardized RIR on pediatric hospital medicine services at our institution. A REDCap survey was developed for attending physicians and fellows on service. The survey focused on the impact of RIR on the plan of care, teaching, learner assessment, efficiency, and patient safety compared to traditional rounds. Surveys were sent to physicians at the end of each service week from October 2020 through May 2021. Statistical analysis focused on descriptive statistics and bivariate analyses accounting for clustering of surveys by physicians using design-based Pearson Chi-Square tests. Two investigators performed content analysis of answers to open-ended questions.
Results: Twenty-eight physicians (26 faculty, 2 fellows) completed 44/54 survey requests (81% response rate). Most physicians reported RIR had no impact on number of medical errors or safety events (98%), and no or positive impact on developmental of a clear plan of care (89%), family’s understanding of plan of care (89%), or learner assessment outside of rounds (84%). In addition, 59% reported that RIR positively impacted the amount of time physicians have for other tasks for that day. However, most reported decreased opportunities to teach (64%) and assess (80%) learners during rounds for the week. Bivariate analysis of the data based on years of physician experience and weeks on service did not find any significant differences.
Qualitative data analysis found that RIRs were successful in promoting resident autonomy and satisfaction. Seeing patients on their own, attending physicians valued the time to connect with families, but reported decreased opportunities for teaching and role modeling. Losing a day of direct observation of family-centered rounds also limited their ability to assess learners. Some expressed challenges with care coordination and team communication for new or complex patients.Conclusion(s): Attending physicians felt RIR enhanced resident autonomy and they enjoyed the opportunities to connect with families. Further work is needed to mitigate the challenges with learner assessment and care coordination for some patients.
Figure 1:
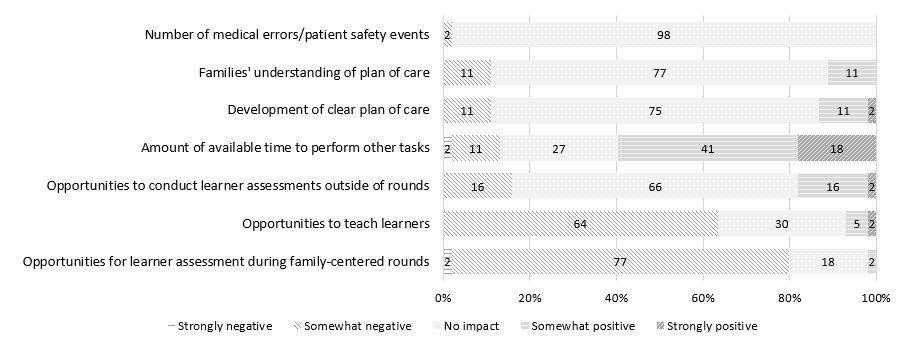 Attending Physicians’ Perspectives Regarding the Impact of Resident-Independent Rounds
Attending Physicians’ Perspectives Regarding the Impact of Resident-Independent Rounds