Telemedicine/EHR/Medical Informatics
Category: Abstract Submission
Telemedicine/EHR/Medical Informatics I
288 - Telemedicine and Pediatric Access to Care Among Low Income Populations during COVID-19
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 288
Publication Number: 288.346
Publication Number: 288.346
Betty Del Rio Rodriguez, Baylor College of Medicine, Pasadena, TX, United States; Linessa Zuniga, Baylor College of Medicine, Houston, TX, United States; Margaret Wood, Baylor College of Medicine, Houston, TX, United States; Deepa Dongarwar, Baylor College of Medicine, Houston, TX, United States; Teresa Duryea, Baylor College of Medicine, Bellaire, TX, United States; Teresia M. O'Connor, Baylor College of Medicine, Houston, TX, United States

Betty Del Rio Rodriguez, MD, MPH (she/her/hers)
Assistant Professor of Pediatrics
Baylor College of Medicine
Pasadena, Texas, United States
Presenting Author(s)
Background: The COVID-19 epidemic accelerated the adoption of telemedicine for health care delivery. Although intended to increase access to care during the pandemic, lack of data on its acceptability among low income, underserved populations could undermine the efforts to reach those who already have difficulty accessing care.
Objective: To assess the varied experiences using telemedicine services during the COVID-19 pandemic across three pediatric primary care sites serving low-income families and to describe clinic implementation, patient use and perceptions of telemedicine services.
Design/Methods: We surveyed parental perceptions of telemedicine using the “Access to Health Care” framework. Two surveys, one for in-person visits and another for video encounters, were developed to assess the dimensions and theoretical constructs in this framework (Table 1). Additional questions were added to the video survey to evaluate access and use of technology needed for video encounters. The survey was sent electronically to all parents of patients seen for in-person or video visits at the 3 clinics from January to June 2021. Bivariate analysis was conducted to assess patients’ perceptions and attitudes about telemedicine and their intention to use telemedicine in the future.
Results: A total of 173 parents consented for the study, 95 completed the survey; 49 for in-person visits and 46 for video visits. Seventy-two percent of parents identified as Hispanic, 41% speak only Spanish at home, 72% had Medicaid and 69% had done a video visit before. Most parents had access to internet through Wi-fi (75%) and cellular data (28%), of which most of them had unlimited data plans (66%). Among constructs from the Access to Care Framework, parents doing video visits believed that in-person visits cost more money (affordability) (p < .01). Parents who did video visits believed the same quality of care could be provided via video or in-person visit (ability to perceive) (p < .01). Parents who attended in-person visits were more likely to wait for an in-person visit if not available as compared to parents that had video visits (ability to seek) (p < .03) (Table 2). Satisfaction was high for both the in-person and video visits. Satisfaction was not significantly different between the two groups. We did not find any barriers to accessing care via telemedicine in our population.Conclusion(s): Our findings indicate that telemedicine is perceived as affordable and well accepted to increase access to care among low income, Spanish speaking populations.
Table 1. Conceptualization of the Access to Care Framework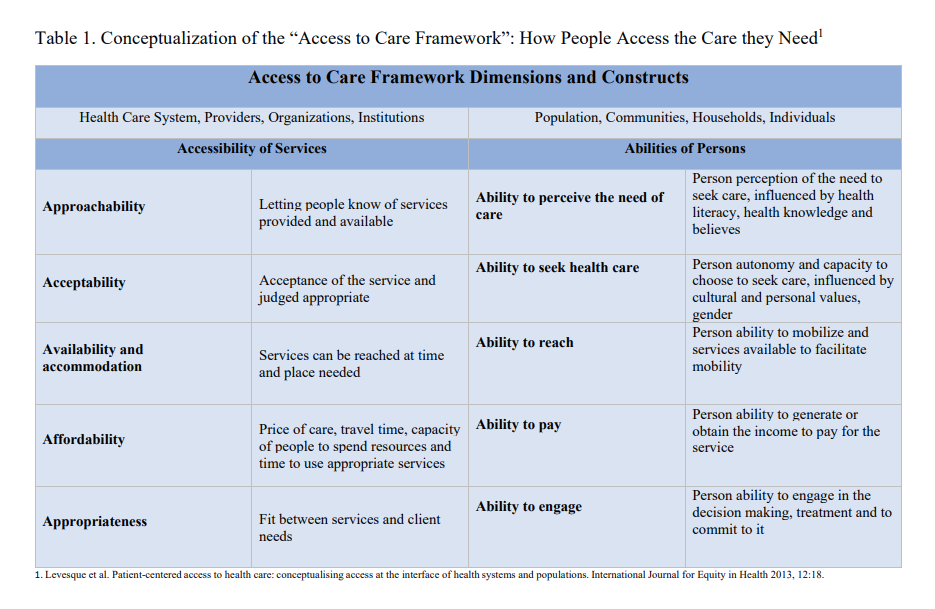 This table illustrates the conceptualization of the Access to Care framework , its dimensions, theoretical construct and definitions.
This table illustrates the conceptualization of the Access to Care framework , its dimensions, theoretical construct and definitions.
Table 2. Application of the "Access to Care Framework" to Telemedicine Services to Pediatric Low-Income Population: dimensions and selected survey questions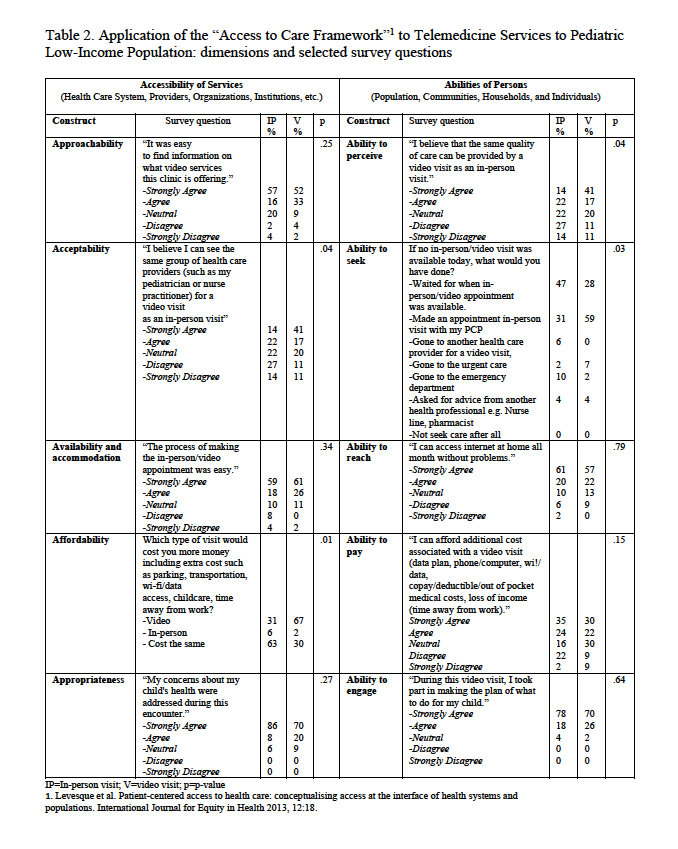 This table illustrates the results for selected survey questions based on the Access to Care Framework.
This table illustrates the results for selected survey questions based on the Access to Care Framework.
Objective: To assess the varied experiences using telemedicine services during the COVID-19 pandemic across three pediatric primary care sites serving low-income families and to describe clinic implementation, patient use and perceptions of telemedicine services.
Design/Methods: We surveyed parental perceptions of telemedicine using the “Access to Health Care” framework. Two surveys, one for in-person visits and another for video encounters, were developed to assess the dimensions and theoretical constructs in this framework (Table 1). Additional questions were added to the video survey to evaluate access and use of technology needed for video encounters. The survey was sent electronically to all parents of patients seen for in-person or video visits at the 3 clinics from January to June 2021. Bivariate analysis was conducted to assess patients’ perceptions and attitudes about telemedicine and their intention to use telemedicine in the future.
Results: A total of 173 parents consented for the study, 95 completed the survey; 49 for in-person visits and 46 for video visits. Seventy-two percent of parents identified as Hispanic, 41% speak only Spanish at home, 72% had Medicaid and 69% had done a video visit before. Most parents had access to internet through Wi-fi (75%) and cellular data (28%), of which most of them had unlimited data plans (66%). Among constructs from the Access to Care Framework, parents doing video visits believed that in-person visits cost more money (affordability) (p < .01). Parents who did video visits believed the same quality of care could be provided via video or in-person visit (ability to perceive) (p < .01). Parents who attended in-person visits were more likely to wait for an in-person visit if not available as compared to parents that had video visits (ability to seek) (p < .03) (Table 2). Satisfaction was high for both the in-person and video visits. Satisfaction was not significantly different between the two groups. We did not find any barriers to accessing care via telemedicine in our population.Conclusion(s): Our findings indicate that telemedicine is perceived as affordable and well accepted to increase access to care among low income, Spanish speaking populations.
Table 1. Conceptualization of the Access to Care Framework
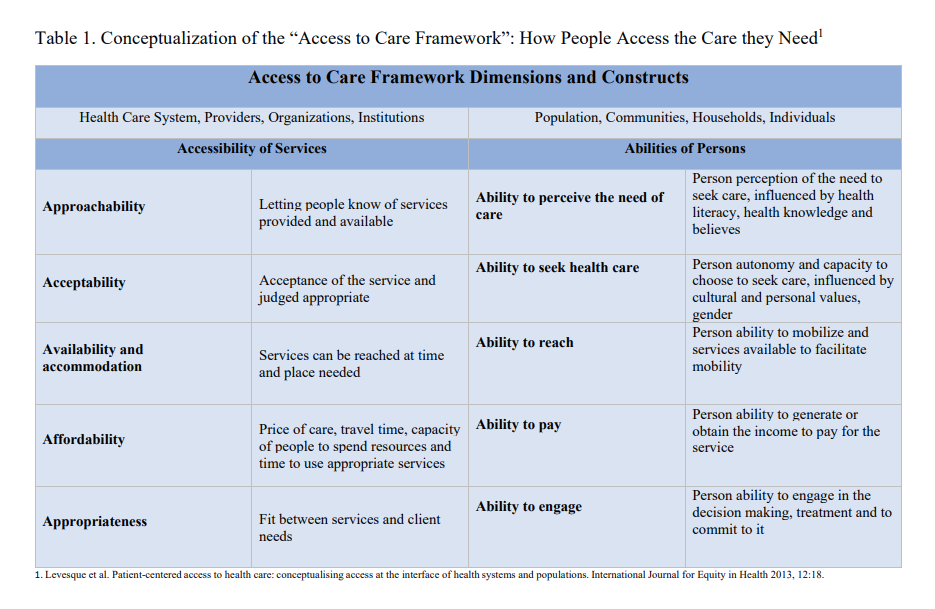 This table illustrates the conceptualization of the Access to Care framework , its dimensions, theoretical construct and definitions.
This table illustrates the conceptualization of the Access to Care framework , its dimensions, theoretical construct and definitions.Table 2. Application of the "Access to Care Framework" to Telemedicine Services to Pediatric Low-Income Population: dimensions and selected survey questions
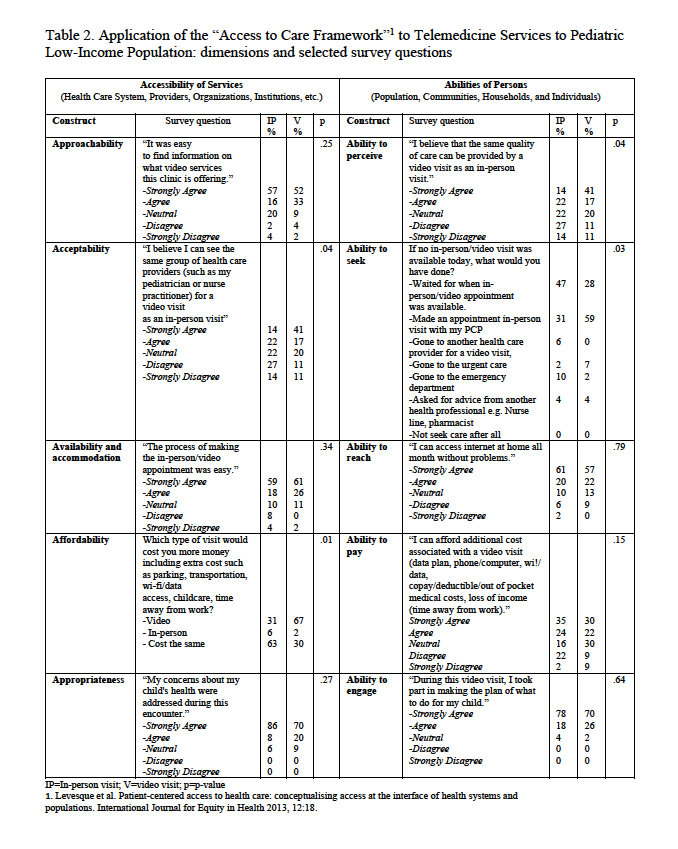 This table illustrates the results for selected survey questions based on the Access to Care Framework.
This table illustrates the results for selected survey questions based on the Access to Care Framework.