Cardiology
Category: Abstract Submission
Cardiology II
98 - Transcatheter Closure of the Patent Ductus Arteriosus Compared to Surgical Ligation: Comparison of Respiratory Outcomes in the Extremely Preterm Infant
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 98
Publication Number: 98.303
Publication Number: 98.303
Valerie Y. Chock, Stanford University School of Medicine, Sunnyvale, CA, United States; Shazia Bhombal, Stanford university, Palo Alto, CA, United States; Alexis Davis, Stanford University School of Medicine, Palo Alto, CA, United States; Meera N. Sankar, Stanford University, Palo Alto, CA, United States; Barbara T. Do, RTI International, Research Triangle Park, NC, United States; Matthew Laughon, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC, United States; Krisa P. Van Meurs, Stanford University School of Medicine, Palo Alto, CA, United States; Carl Backes, Nationwide Children's Hospital, Columbus, OH, United States; Patrick J. McNamara, University of Iowa Roy J. and Lucille A. Carver College of Medicine, Iowa City, IA, United States

Valerie Y. Chock, MD, MS Epi (she/her/hers)
Professor of Pediatrics
Stanford University School of Medicine
Palo Alto, California, United States
Presenting Author(s)
Background: Cardiac transcatheter closure of the patent ductus arteriosus (PDA) in preterm infants has become an increasingly common treatment option. Characterization of the preterm population undergoing transcatheter PDA closure and assessment of respiratory outcomes is critical to understanding the effects of changing approaches to PDA management and for the design of future trials.
Objective: To determine if preterm infants < 29 weeks gestation or with birth weight < 1000 g with a PDA treated with transcatheter closure compared to surgical ligation had improved respiratory outcomes.
Design/Methods: A retrospective analysis of the NICHD Neonatal Research Network’s Generic Database from 1/1/2016 until 12/31/2020 compared infants with transcatheter PDA closure to those treated with surgical ligation with a primary outcome of total days of mechanical ventilation. Additional respiratory outcomes included bronchopulmonary dysplasia (BPD), days on positive pressure, need for home oxygen, and diuretics at discharge. Linear and logistic regression analyses were adjusted for center, birth year, gestational age, and age at PDA intervention.
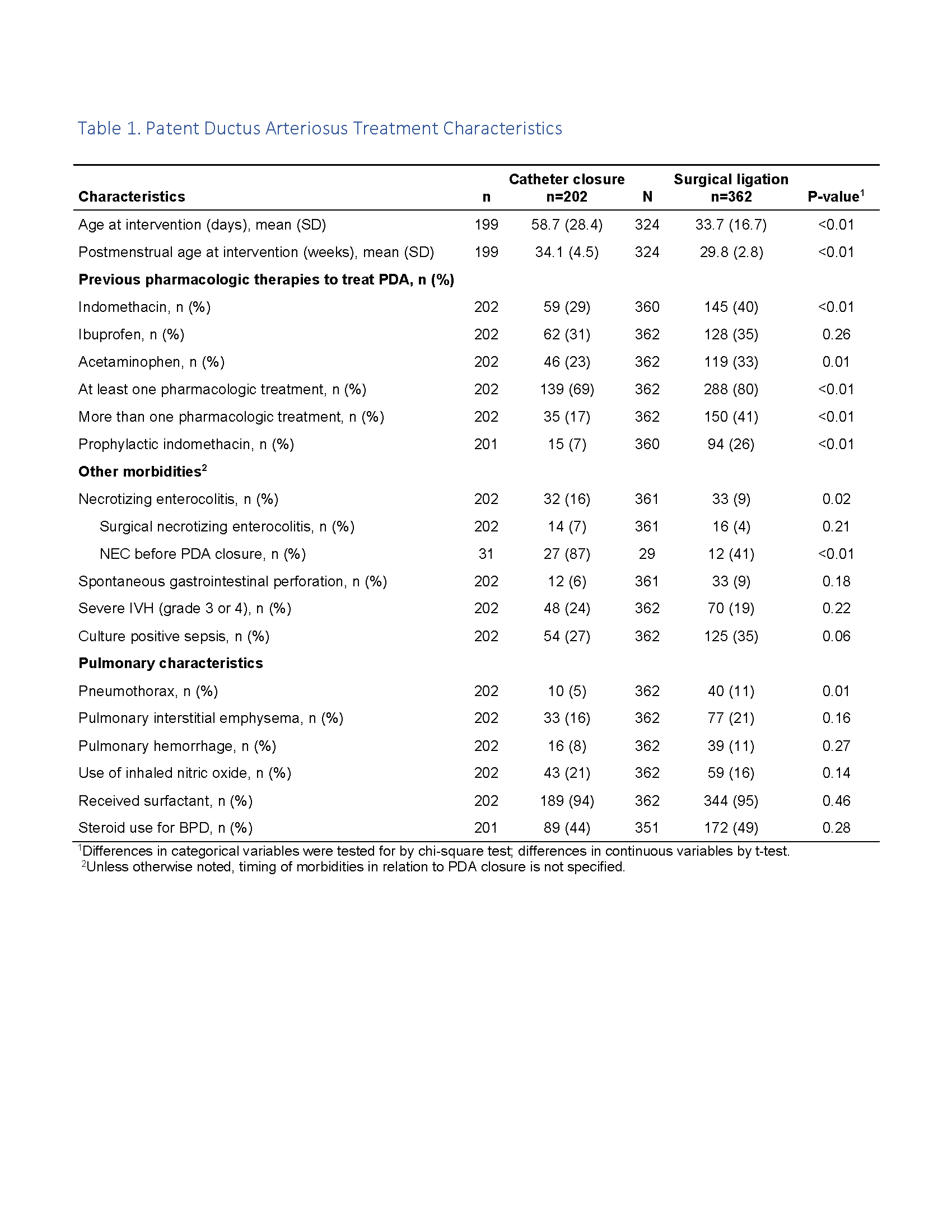
Results: 202 infants (36%) underwent transcatheter PDA closure compared to 362 (64%) who were treated with surgical ligation. Transcatheter closure rate increased over the study period while ligation rate decreased (Fig. 1). Median gestational age was 25.4 weeks (24.1, 27.1) in transcatheter closure group versus 24.9 weeks (24.0, 25.9) in surgical ligation group. Age at transcatheter closure was significantly greater than age at ligation (59 vs. 34 days, p < 0.01). Transcatheter closure group was less likely to have received pharmacologic PDA treatment, less likely to have had a pneumothorax, but more commonly had pre-intervention necrotizing enterocolitis (Table 1). Compared to surgical ligation, infants with transcatheter PDA closure demonstrated no difference in respiratory outcomes including total days of mechanical ventilation, positive pressure support, BPD, home oxygen use, or diuretics at discharge (Table 2).Conclusion(s): Transcatheter PDA closure was not associated with improved respiratory outcomes for extremely preterm infants with a PDA when compared to surgical ligation. Future research is needed to assess the optimal timing of transcatheter PDA closure given the significant difference in age at intervention and to determine if earlier intervention affects outcomes.
Figure 1. PDA Treatment 2016 - 2020.png)
Table 1. Patent Ductus Arteriosus Treatment Characteristics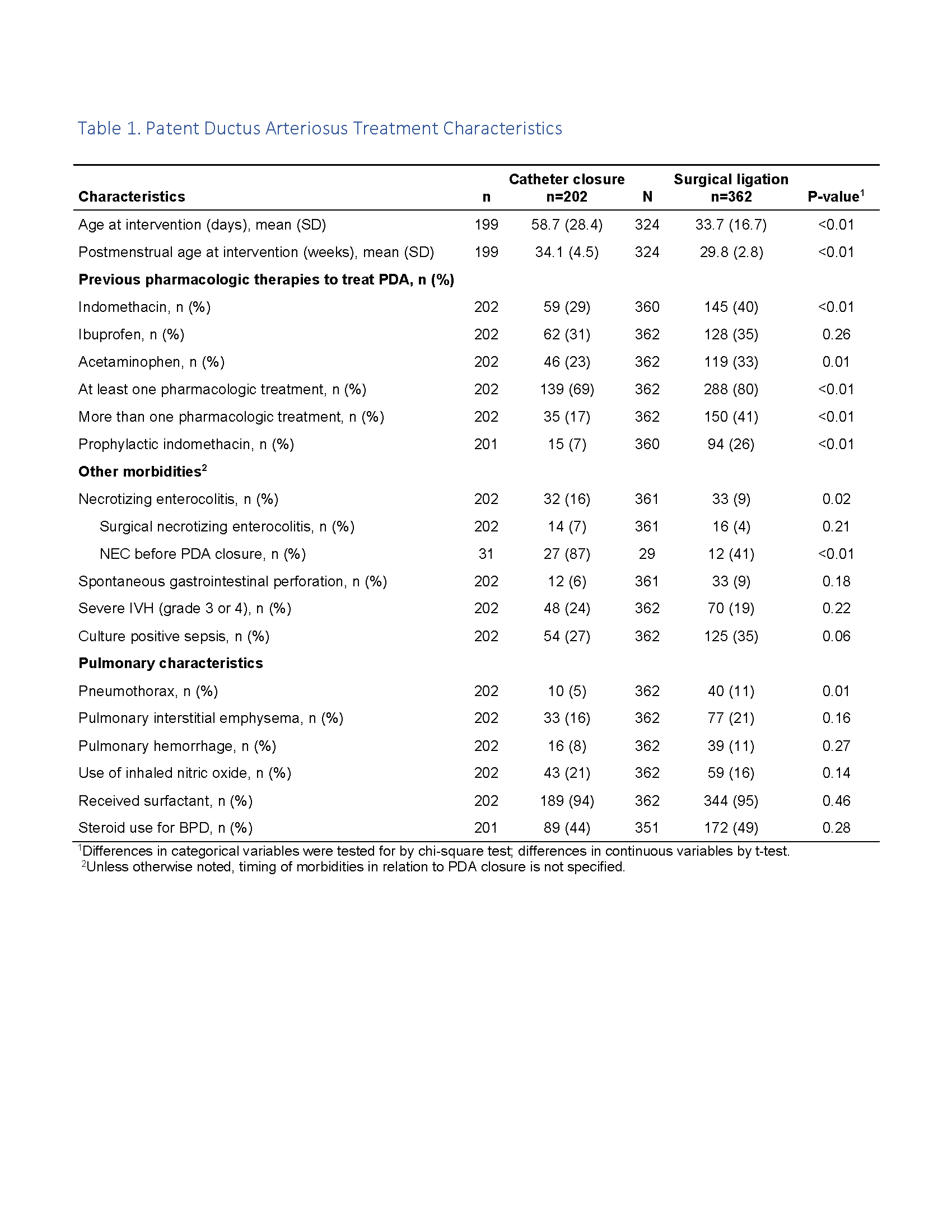
Objective: To determine if preterm infants < 29 weeks gestation or with birth weight < 1000 g with a PDA treated with transcatheter closure compared to surgical ligation had improved respiratory outcomes.
Design/Methods: A retrospective analysis of the NICHD Neonatal Research Network’s Generic Database from 1/1/2016 until 12/31/2020 compared infants with transcatheter PDA closure to those treated with surgical ligation with a primary outcome of total days of mechanical ventilation. Additional respiratory outcomes included bronchopulmonary dysplasia (BPD), days on positive pressure, need for home oxygen, and diuretics at discharge. Linear and logistic regression analyses were adjusted for center, birth year, gestational age, and age at PDA intervention.
Results: 202 infants (36%) underwent transcatheter PDA closure compared to 362 (64%) who were treated with surgical ligation. Transcatheter closure rate increased over the study period while ligation rate decreased (Fig. 1). Median gestational age was 25.4 weeks (24.1, 27.1) in transcatheter closure group versus 24.9 weeks (24.0, 25.9) in surgical ligation group. Age at transcatheter closure was significantly greater than age at ligation (59 vs. 34 days, p < 0.01). Transcatheter closure group was less likely to have received pharmacologic PDA treatment, less likely to have had a pneumothorax, but more commonly had pre-intervention necrotizing enterocolitis (Table 1). Compared to surgical ligation, infants with transcatheter PDA closure demonstrated no difference in respiratory outcomes including total days of mechanical ventilation, positive pressure support, BPD, home oxygen use, or diuretics at discharge (Table 2).Conclusion(s): Transcatheter PDA closure was not associated with improved respiratory outcomes for extremely preterm infants with a PDA when compared to surgical ligation. Future research is needed to assess the optimal timing of transcatheter PDA closure given the significant difference in age at intervention and to determine if earlier intervention affects outcomes.
Figure 1. PDA Treatment 2016 - 2020
.png)
Table 1. Patent Ductus Arteriosus Treatment Characteristics