Hematology/Oncology
Category: Abstract Submission
Hematology/Oncology II
579 - Transfusion and Survival among Childhood, Adolescent, and Young Adult Patients with Osteosarcoma: A Research Network Analysis
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 579
Publication Number: 579.321
Publication Number: 579.321
Sukjoo Cho, USF Health Morsani College of Medicine, Tampa, FL, United States; Racha T. Khalaf, University of South Florida, Tampa, FL, United States; Jamie L. Fierstein, Johns Hopkins All Children's Hospital, St. Petersburg, FL, United States; John M. Morrison, Johns Hopkins All Children's Hospital, Saint Petersburg, FL, United States; juan f. rico, USF Health Morsani College of Medicine, Tampa, FL, United States; Jonathan Metts, Johns Hopkins All Children's Hospital, St Petersburg, FL, FL, United States
Sukjoo Cho, MD
Resident
USF Health Morsani College of Medicine
Tampa, Florida, United States
Presenting Author(s)
Background: Prior data suggest that pretransplant blood transfusion is associated with decreased renal allograft rejection. Blood transfusion may suppress the immune system of recipients, thereby promoting cancer growth. It is accepted that blood transfusion is associated with decreased survival and increased recurrence of certain tumors such as colorectal cancer. However, little is known about the relationship between blood transfusion and childhood, adolescent, and young adult (CAYA; i.e., ≤ 39 years of age) cancer. We thus chose to study this relationship in osteosarcoma, a cancer seen in CAYA patients that frequently requires transfusion due to local control measures and systemic chemotherapy exposure.
Objective: To evaluate the association between post-diagnosis blood transfusion and 3- and 5-year overall survival (OS) among CAYA patients with osteosarcoma
Design/Methods: This retrospective, multicenter cohort study utilized the TriNetX (TriNetX, LLC, Cambridge, MA) research network of de-identified electronic medical records with real-time updates from 57 healthcare organizations, last accessed on 1/3/2022. We queried CAYA osteosarcoma patients using diagnostic codes for bone cancer (C40-C41) and medication/procedure codes (2555, J9060) for cisplatin, a first-line chemotherapy for osteosarcoma, infrequently given for other sarcomas. Our primary exposure was post-diagnosis blood transfusion. OS rates at 3 and 5 years were calculated using Kaplan-Meier analysis. OS curves were compared using the log-rank test. Two-sided p-values < 0.05 were considered statistically significant.
Results: At the time of our search query, 26.9% (168/623) of 623 CAYA patients with osteosarcoma were transfused post-diagnosis. Eight patients in the non-transfused group were excluded due to receiving an osteosarcoma diagnosis (i.e., the index event) > 20 years ago. Patient characteristics are shown in Table 1. The mean age at diagnosis did not differ significantly between transfused and non-transfused groups (19.1 vs 21.0 years; p = 0.05). We found significant differences in 3- and 5-year OS between the transfused and non-transfused groups (Figure 1). The 3-year OS rates were 62.6% and 78.2% in the transfused and non-transfused groups, respectively (p < 0.01). The 5-year OS rates were 54.3% and 71.3%, respectively (p < 0.01).Conclusion(s): We observed that blood transfusion was associated with decreased OS rates at 3 and 5 years among CAYA patients with osteosarcoma. Further in-depth analyses accounting for potential confounders including surgery, radiation, and other chemotherapy exposures will be performed.
CV_Sukjoo Cho.pdf
Figure 1. Kaplan-Meier Curve for Overall Survival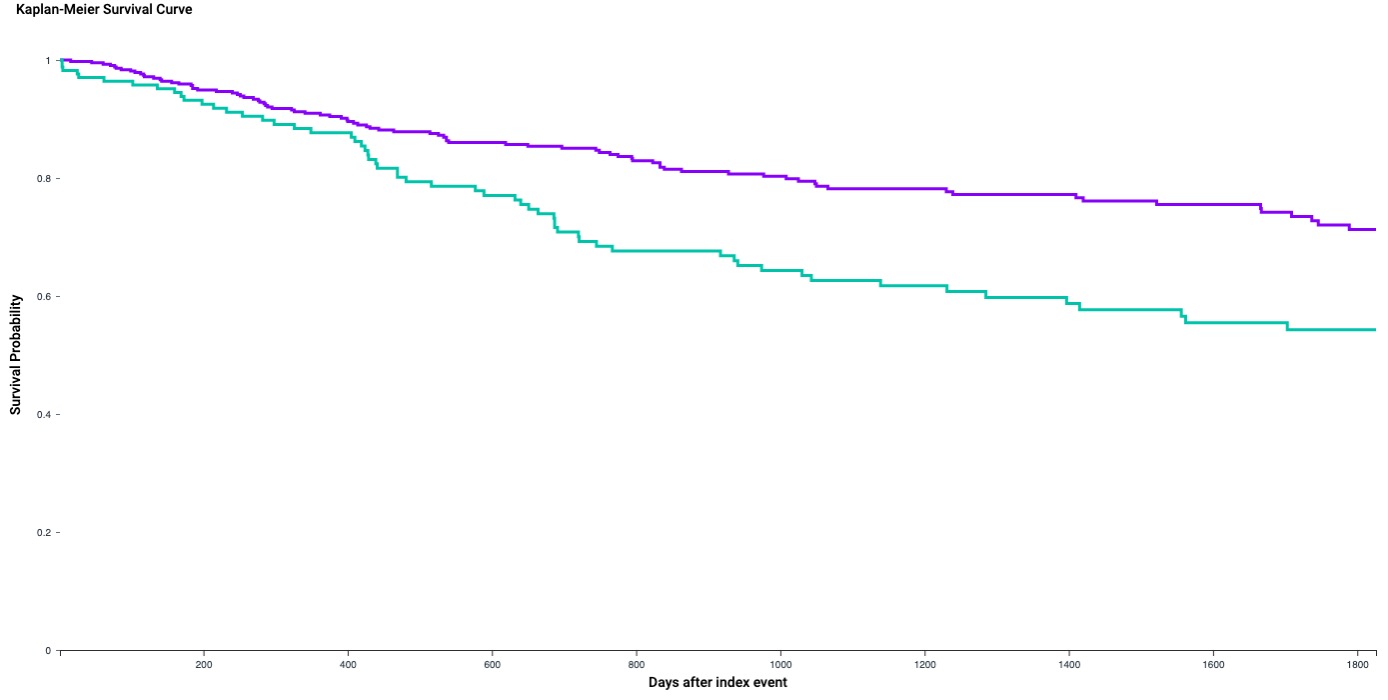 Significant differences in 3- and 5-year OS between the transfused and non-transfused groups were observed. The 3-year OS rates were 62.6% and 78.2% in the transfused and non-transfused groups, respectively (p < 0.01). The 5-year OS rates were 54.3% and 71.3%, respectively (p < 0.01).
Significant differences in 3- and 5-year OS between the transfused and non-transfused groups were observed. The 3-year OS rates were 62.6% and 78.2% in the transfused and non-transfused groups, respectively (p < 0.01). The 5-year OS rates were 54.3% and 71.3%, respectively (p < 0.01).
Objective: To evaluate the association between post-diagnosis blood transfusion and 3- and 5-year overall survival (OS) among CAYA patients with osteosarcoma
Design/Methods: This retrospective, multicenter cohort study utilized the TriNetX (TriNetX, LLC, Cambridge, MA) research network of de-identified electronic medical records with real-time updates from 57 healthcare organizations, last accessed on 1/3/2022. We queried CAYA osteosarcoma patients using diagnostic codes for bone cancer (C40-C41) and medication/procedure codes (2555, J9060) for cisplatin, a first-line chemotherapy for osteosarcoma, infrequently given for other sarcomas. Our primary exposure was post-diagnosis blood transfusion. OS rates at 3 and 5 years were calculated using Kaplan-Meier analysis. OS curves were compared using the log-rank test. Two-sided p-values < 0.05 were considered statistically significant.
Results: At the time of our search query, 26.9% (168/623) of 623 CAYA patients with osteosarcoma were transfused post-diagnosis. Eight patients in the non-transfused group were excluded due to receiving an osteosarcoma diagnosis (i.e., the index event) > 20 years ago. Patient characteristics are shown in Table 1. The mean age at diagnosis did not differ significantly between transfused and non-transfused groups (19.1 vs 21.0 years; p = 0.05). We found significant differences in 3- and 5-year OS between the transfused and non-transfused groups (Figure 1). The 3-year OS rates were 62.6% and 78.2% in the transfused and non-transfused groups, respectively (p < 0.01). The 5-year OS rates were 54.3% and 71.3%, respectively (p < 0.01).Conclusion(s): We observed that blood transfusion was associated with decreased OS rates at 3 and 5 years among CAYA patients with osteosarcoma. Further in-depth analyses accounting for potential confounders including surgery, radiation, and other chemotherapy exposures will be performed.
CV_Sukjoo Cho.pdf
Figure 1. Kaplan-Meier Curve for Overall Survival
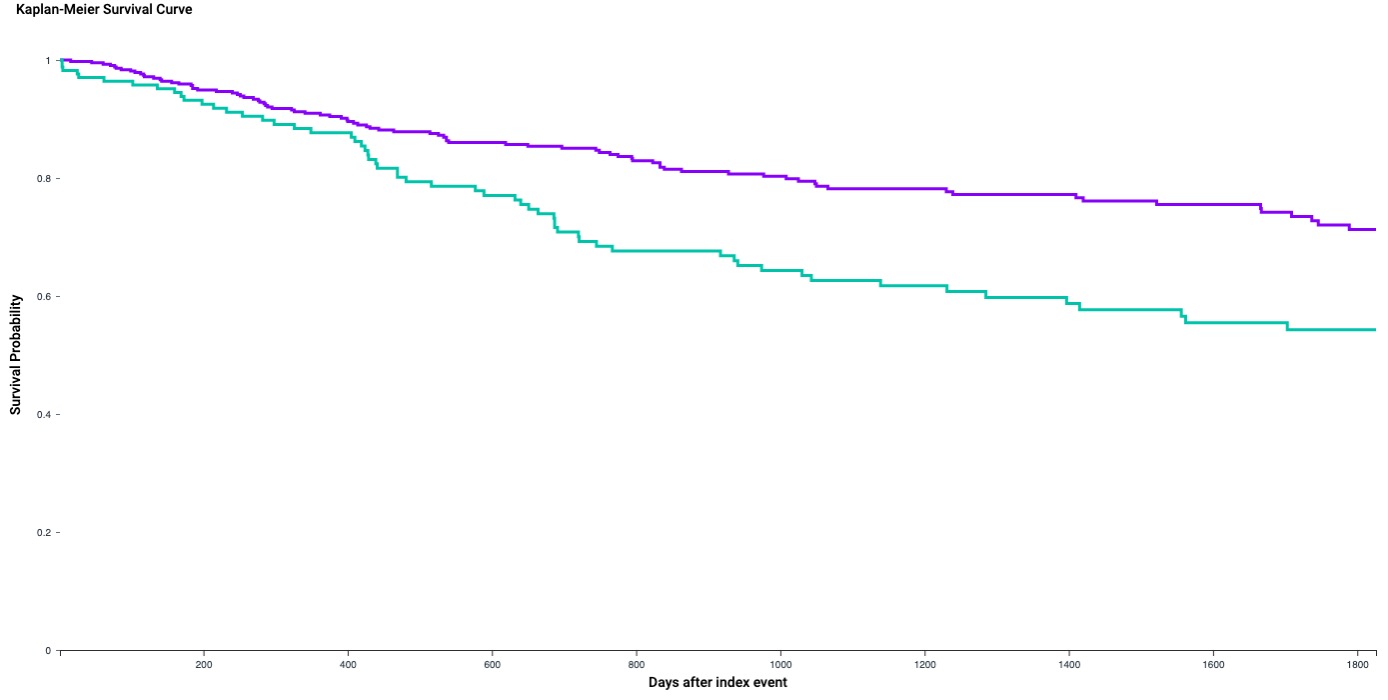 Significant differences in 3- and 5-year OS between the transfused and non-transfused groups were observed. The 3-year OS rates were 62.6% and 78.2% in the transfused and non-transfused groups, respectively (p < 0.01). The 5-year OS rates were 54.3% and 71.3%, respectively (p < 0.01).
Significant differences in 3- and 5-year OS between the transfused and non-transfused groups were observed. The 3-year OS rates were 62.6% and 78.2% in the transfused and non-transfused groups, respectively (p < 0.01). The 5-year OS rates were 54.3% and 71.3%, respectively (p < 0.01).