Telemedicine/EHR/Medical Informatics
Category: Abstract Submission
Telemedicine/EHR/Medical Informatics I
289 - Transitions of Care Barriers Addressed through Novel Nurse-led Telehealth for Children with Medical Complexity
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 289
Publication Number: 289.346
Publication Number: 289.346
Mark Brittan, Children's Hospital Colorado, Aurora, CO, United States; Susan Fisk, Children's Hospital Colorado, Frederick, CO, United States; Fidelity Dominguez, Children's Hospital Colorado, Brighton, CO, United States; Brooke Geyer, University of Colorado School of Medicine, Colorado Springs, CO, United States; Christina Olson, University of Colorado School of Medicine, Aurora, CO, United States
- MB
Mark Brittan, MD, MPH
Associate Professor
University of Colorado
Aurora, Colorado, United States
Presenting Author(s)
Background: In 1/2020 we implemented a nurse-led telehealth program to bridge transitions to home/ambulatory care for children with medical complexity (CMC).
Objective: We aimed to characterize transitions of care (TOC) barriers and successes identified by the program to provide insight into discharge challenges faced by families of CMC.
Design/Methods: Eligible CMC from multiple inpatient services and two distinct hospitals in our system were enrolled via a newly developed registry. Eligibility criteria included: ≥1 home health order (excluding oxygen), hospital length of stay ≥7 days, and ≥1 hospitalization or ED encounter in preceding 12 months (NICU patients excepted). For each patient, the telehealth nurse (RN) met with the family prior to discharge and conducted 1 in-home telehealth visit within 7 days and additional contacts as needed up to 30 days after discharge. All existing peri-discharge/case management services and follow-up visits remained in place. Primary care providers (PCP), care coordinators, and home health nurses were invited to join telehealth visits to enhance the transition to ambulatory care. During these visits, the telehealth RN documented TOC barriers in the domains of follow up appointments, supply issues, home care services, medication problems, clinical concerns and other. Pertinent successes were also recorded from the onset of data collection in 4/2021.
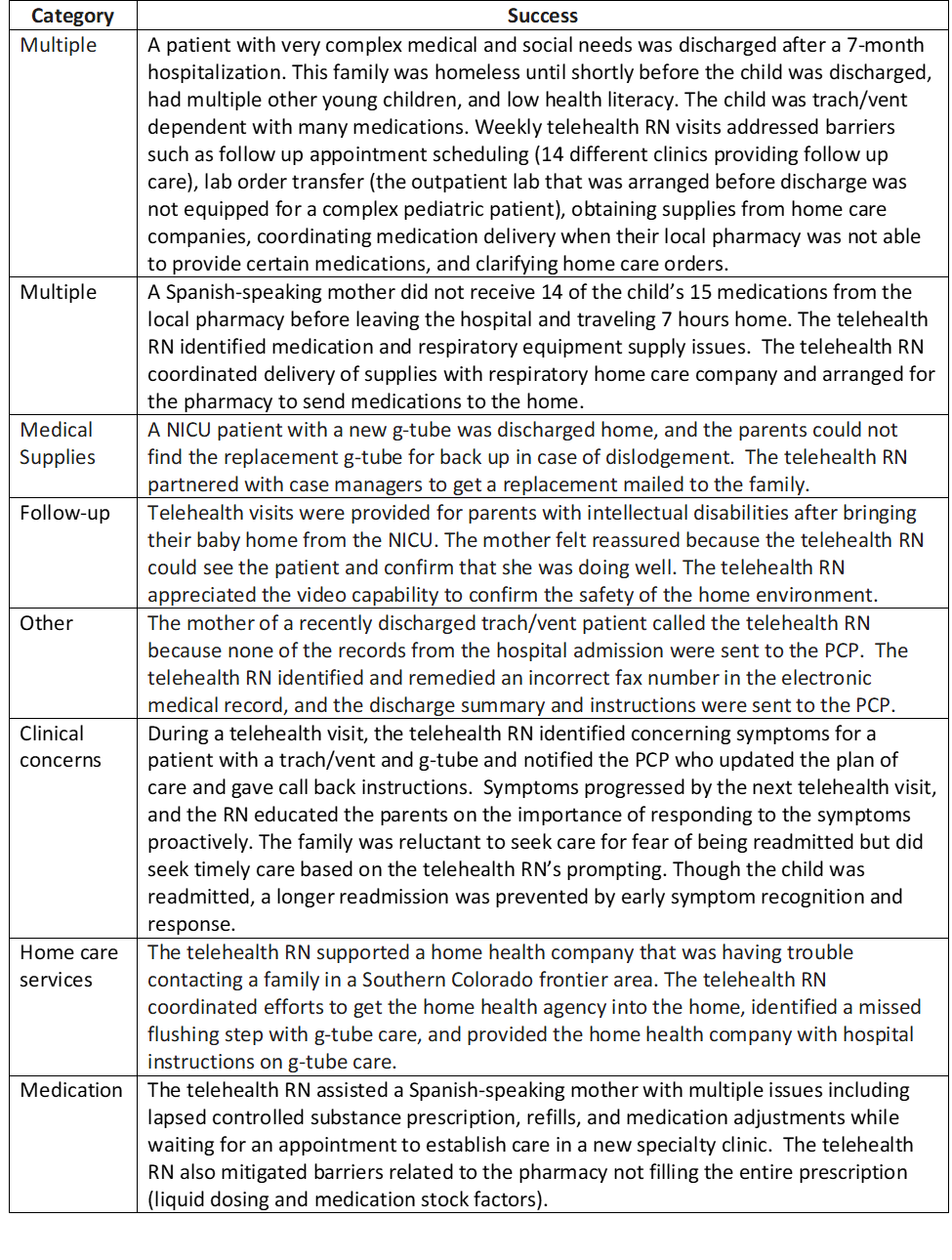
Results: For 111 patients with 144 completed telehealth visits (April – November 2021), 100 TOC barriers were identified and addressed; 22 patients had barriers in 2 categories and 14 patients had ≥3 categories. Problems with appointment follow-up (36%) were most common, followed by medical supply issues (23%), other (16%), home care services (11%), medications (11%), and clinical concerns (3%). Examples of “other” problems included a home health RN needing feeding order clarification, PCP without hospital records, and incorrectly mixed formula. Success stories (Table) highlighted additional advantages of telehealth follow-up such as assessment of the home environment and supplies.Conclusion(s): Our program identified and remedied numerous TOC barriers for hospitalized CMC that occurred despite robust discharge processes, demonstrating the significant burden endured by these families and the potential for RN-led telehealth to innovate and improve on their transitions of care. In our setting, problems with follow-up appointments and medical supply issues were most common. Future work will assess the impact of this program on healthcare utilization and costs in the 60 days following discharge.
TABLE: Patient and Family Successes attributed to the Telehealth RN Program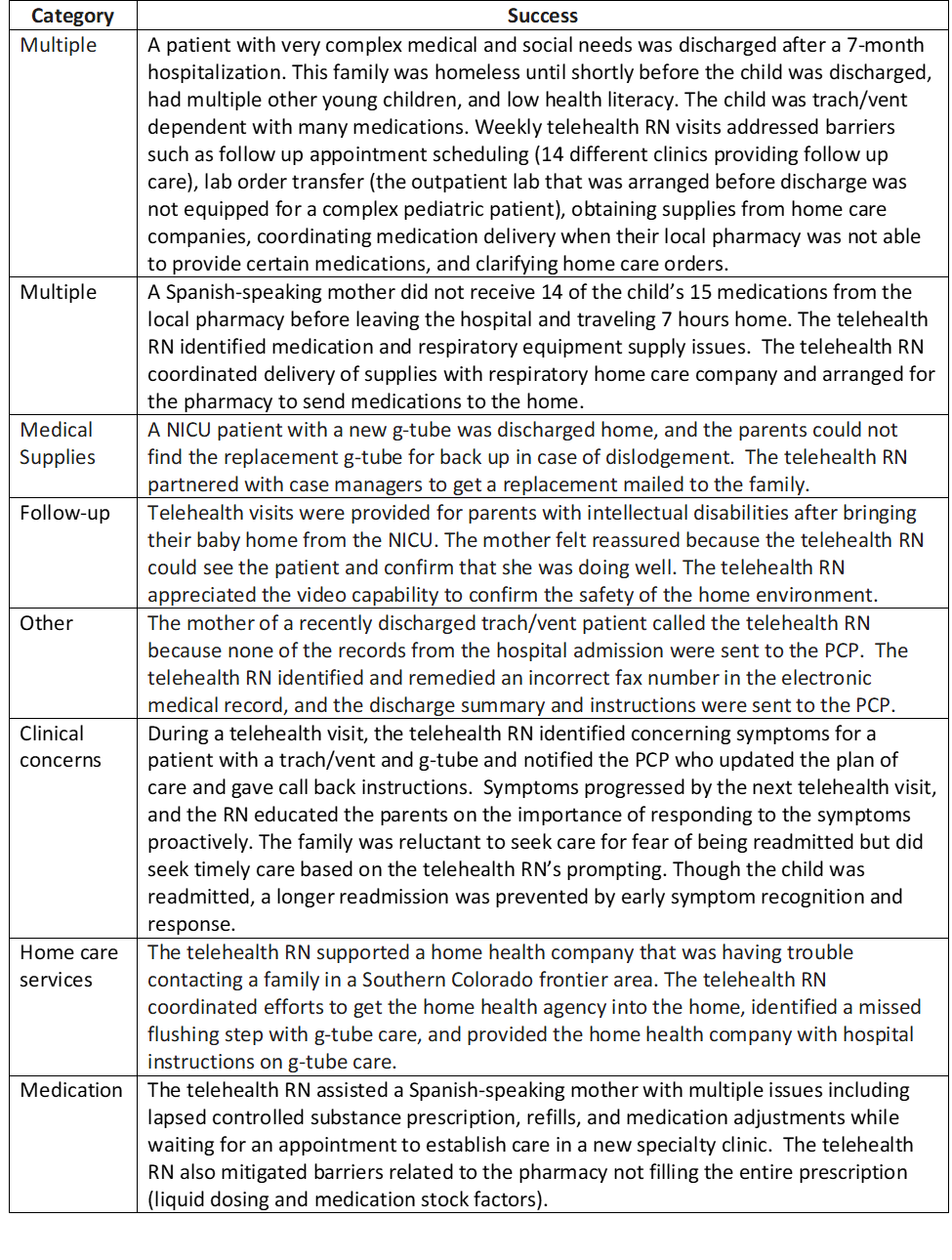
Objective: We aimed to characterize transitions of care (TOC) barriers and successes identified by the program to provide insight into discharge challenges faced by families of CMC.
Design/Methods: Eligible CMC from multiple inpatient services and two distinct hospitals in our system were enrolled via a newly developed registry. Eligibility criteria included: ≥1 home health order (excluding oxygen), hospital length of stay ≥7 days, and ≥1 hospitalization or ED encounter in preceding 12 months (NICU patients excepted). For each patient, the telehealth nurse (RN) met with the family prior to discharge and conducted 1 in-home telehealth visit within 7 days and additional contacts as needed up to 30 days after discharge. All existing peri-discharge/case management services and follow-up visits remained in place. Primary care providers (PCP), care coordinators, and home health nurses were invited to join telehealth visits to enhance the transition to ambulatory care. During these visits, the telehealth RN documented TOC barriers in the domains of follow up appointments, supply issues, home care services, medication problems, clinical concerns and other. Pertinent successes were also recorded from the onset of data collection in 4/2021.
Results: For 111 patients with 144 completed telehealth visits (April – November 2021), 100 TOC barriers were identified and addressed; 22 patients had barriers in 2 categories and 14 patients had ≥3 categories. Problems with appointment follow-up (36%) were most common, followed by medical supply issues (23%), other (16%), home care services (11%), medications (11%), and clinical concerns (3%). Examples of “other” problems included a home health RN needing feeding order clarification, PCP without hospital records, and incorrectly mixed formula. Success stories (Table) highlighted additional advantages of telehealth follow-up such as assessment of the home environment and supplies.Conclusion(s): Our program identified and remedied numerous TOC barriers for hospitalized CMC that occurred despite robust discharge processes, demonstrating the significant burden endured by these families and the potential for RN-led telehealth to innovate and improve on their transitions of care. In our setting, problems with follow-up appointments and medical supply issues were most common. Future work will assess the impact of this program on healthcare utilization and costs in the 60 days following discharge.
TABLE: Patient and Family Successes attributed to the Telehealth RN Program