Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: Potpourri
566 - Urinary Tract Infection (UTI) Epidemiology in United States Neonatal Intensive Care Units
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 566
Publication Number: 566.336
Publication Number: 566.336
Ryan Kilpatrick, Duke University School of Medicine, Durham, NC, United States; Angelique E. Boutzoukas, Duke University School of Medicine, Durham, NC, United States; Elizabeth Chan, Duke Clinical Research Institute, Holly Springs, NC, United States; Valerie Girgis, Duke Clinical Research Institute, Chapel Hill, NC, United States; Vincent M. Kinduelo, Duke Clinical Research Institute, Raleigh, NC, United States; Sarah A. Kwabia, Duke Clinical Research Institute, Raleigh, NC, United States; Jenny Yan, Duke Clinical Research Institute, Durham, NC, United States; Reese H. Clark, MEDNAX, Myrtle Beach, SC, United States; Kanecia O. Zimmerman, Duke Clinical Research Institute, Durham, NC, United States; Rachel G. Greenberg, Duke Clinical Research Institute, Durham, NC, United States

Ryan Kilpatrick, MD (he/him/his)
Fellow
Duke University School of Medicine
Durham, North Carolina, United States
Presenting Author(s)
Background: UTI is a common cause and occasional complication of late onset sepsis in very low birth weight infants (VLBW, birth weight < 1500g). Incidence, risk factors, timing of infection, and microbiology of UTI in VLBW infants are not well described in the medical literature.
Objective: Characterize the incidence, risk factors, timing of infection, microbiology, and rate of concordant blood culture for UTI in VLBW infants.
Design/Methods: We performed a multicenter cohort study of VLBW infants with gestational age (GA) < 32 weeks, still hospitalized on postnatal day 7, and discharged 2010-2018 from Pediatrix Medical Group neonatal intensive care units. Infants with major urinary tract abnormalities were excluded. We compared demographic and clinical characteristics of infants with and without UTI. We described the microbiology of urine cultures and incidence of concordant blood culture. UTI was defined as isolation of a single pathogenic organism from collected urine culture. Concordant positive blood culture was defined as isolation of the same pathogenic organism in blood within 3 days before or after a UTI diagnosis.
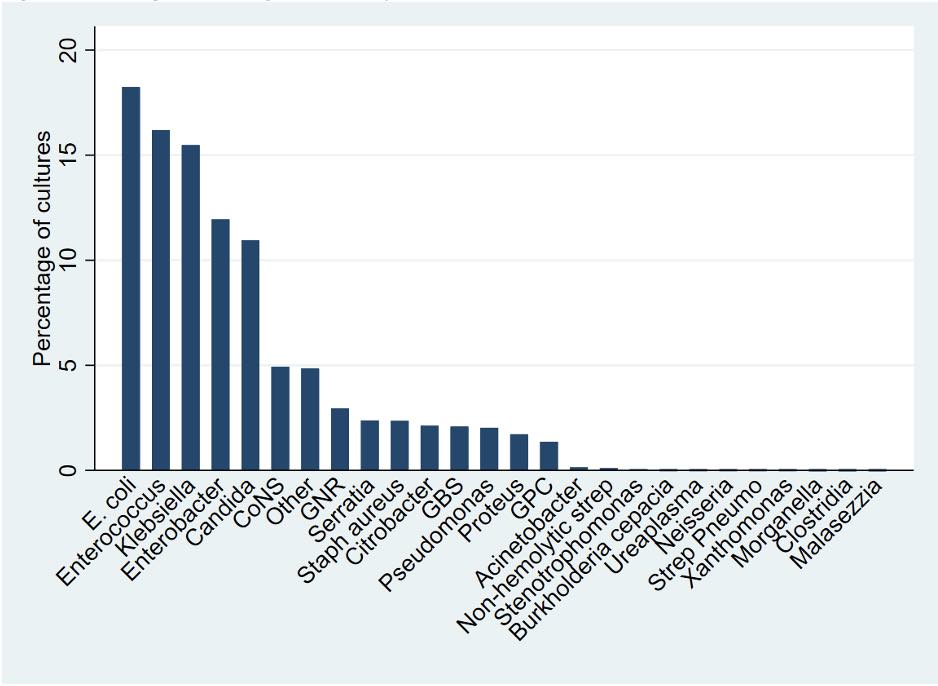
Results: Of 170,552 included infants, 10,240 (6%) infants had a UTI (Table 1). Positive urine cultures were most common in infants postnatal age 8–30 days (4,289 [42%]). E. coli was the most common pathogen (18%), followed by Enterococcus (16%), and Klebsiella (16%) (Figure 1). Candida (11%) was the most common non-bacterial pathogen. Concordant positive blood culture was present with 1,064 (10%) of these UTI diagnoses. Infants < 24 weeks GA had the highest risk of UTI (Table 2). Compared to infants < 24 weeks GA, infants 25-28 weeks GA had an odds ratio (OR) of 0.63 (95% CI 0.59-0.66) and infants 29-32 weeks GA had OR 0.22 (95% CI 0.20-0.23). Other factors associated with UTI included male sex (OR 2.17 (95% CI 2.08-2.28)), small for gestational age (SGA) status (OR 1.15 (95% CI 1.09-1.22)), prenatal steroid exposure (OR 1.15 (95% CI 1.09-1.22)). C-section delivery (OR 0.91 (95% CI 0.87–0.96)) was associated with decreased odds of UTI compared to vaginal delivery.Conclusion(s): In this large cohort of VLBW infants, UTI was associated with lower GA, male sex, SGA status, prenatal steroid exposure, and vaginal delivery.
Ryan Kilpatrick CVRyan Kilpatrick - CV 12.23.2021.pdf
Figure 1: Pathogens causing first urinary tract infection.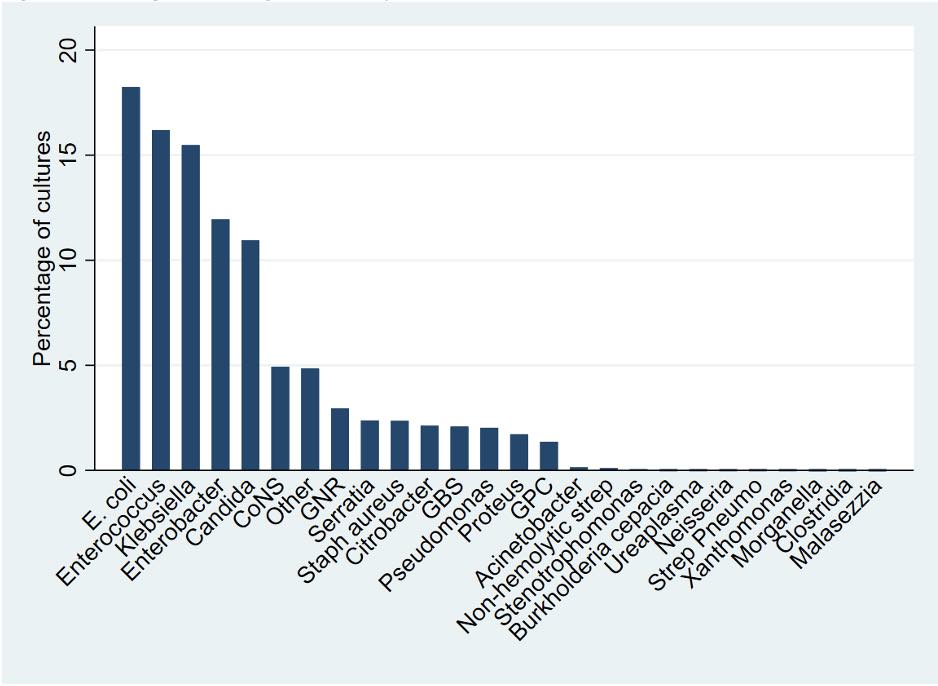
Objective: Characterize the incidence, risk factors, timing of infection, microbiology, and rate of concordant blood culture for UTI in VLBW infants.
Design/Methods: We performed a multicenter cohort study of VLBW infants with gestational age (GA) < 32 weeks, still hospitalized on postnatal day 7, and discharged 2010-2018 from Pediatrix Medical Group neonatal intensive care units. Infants with major urinary tract abnormalities were excluded. We compared demographic and clinical characteristics of infants with and without UTI. We described the microbiology of urine cultures and incidence of concordant blood culture. UTI was defined as isolation of a single pathogenic organism from collected urine culture. Concordant positive blood culture was defined as isolation of the same pathogenic organism in blood within 3 days before or after a UTI diagnosis.
Results: Of 170,552 included infants, 10,240 (6%) infants had a UTI (Table 1). Positive urine cultures were most common in infants postnatal age 8–30 days (4,289 [42%]). E. coli was the most common pathogen (18%), followed by Enterococcus (16%), and Klebsiella (16%) (Figure 1). Candida (11%) was the most common non-bacterial pathogen. Concordant positive blood culture was present with 1,064 (10%) of these UTI diagnoses. Infants < 24 weeks GA had the highest risk of UTI (Table 2). Compared to infants < 24 weeks GA, infants 25-28 weeks GA had an odds ratio (OR) of 0.63 (95% CI 0.59-0.66) and infants 29-32 weeks GA had OR 0.22 (95% CI 0.20-0.23). Other factors associated with UTI included male sex (OR 2.17 (95% CI 2.08-2.28)), small for gestational age (SGA) status (OR 1.15 (95% CI 1.09-1.22)), prenatal steroid exposure (OR 1.15 (95% CI 1.09-1.22)). C-section delivery (OR 0.91 (95% CI 0.87–0.96)) was associated with decreased odds of UTI compared to vaginal delivery.Conclusion(s): In this large cohort of VLBW infants, UTI was associated with lower GA, male sex, SGA status, prenatal steroid exposure, and vaginal delivery.
Ryan Kilpatrick CVRyan Kilpatrick - CV 12.23.2021.pdf
Figure 1: Pathogens causing first urinary tract infection.