Neonatal General
Category: Abstract Submission
Neonatology General 8: Health Disparities - Health Services Research
223 - Utilization and cost of laboratory testing in very low birth weight infants hospitalized in the neonatal intensive care unit
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 223
Publication Number: 223.339
Publication Number: 223.339
Megan E. Gross, Rush University Medical Center, Forest Park, IL, United States; Tricia J. Johnson, Rush University, Chicago, IL, United States; Patoula Panagos, University of Central Florida At Nemours Children's Hospital, Orlando, FL, United States; Beverley Robin, Rush Medical College of Rush University Medical Center, Chicago, IL, United States; Aloka L. Patel, Rush Medical College of Rush University Medical Center, Chicago, IL, United States
- MG
Megan E. Gross, MS, PGC
Clinical Research
Rush University Medical Center
Chicago, Illinois, United States
Presenting Author(s)
Background: Phlebotomy for laboratory testing (labs) is a primary contributor to anemia and subsequent blood transfusions for very low birth weight (VLBW) infants hospitalized in the neonatal intensive care unit (NICU). The use of healthcare checklists is a promising method to reduce labs. A checklist was implemented to reduce unnecessary labs and to optimize resource utilization.
Objective: To compare the frequency of labs, blood transfusions, and associated costs for VLBW infants hospitalized in the NICU, pre- and post- checklist implementation.
Design/Methods: This retrospective study included 356 VLBW infants admitted to the NICU in 2008-2010 (pre-checklist; PRE) or 2018-2019 (post-checklist; POST). Data for the PRE group were obtained from a prospective cohort study. POST group data were obtained from electronic medical record chart review and the hospital financial records system. Outcomes were analyzed by time period, and by subgroups of gestational age (GA) and week of life (WOL). Costs were standardized to 2020 US dollars. Nonparametric tests were used to compare the outcomes between time periods and for subgroup analyses. Bonferroni correction was used to adjust the significance levels for multiple comparisons.
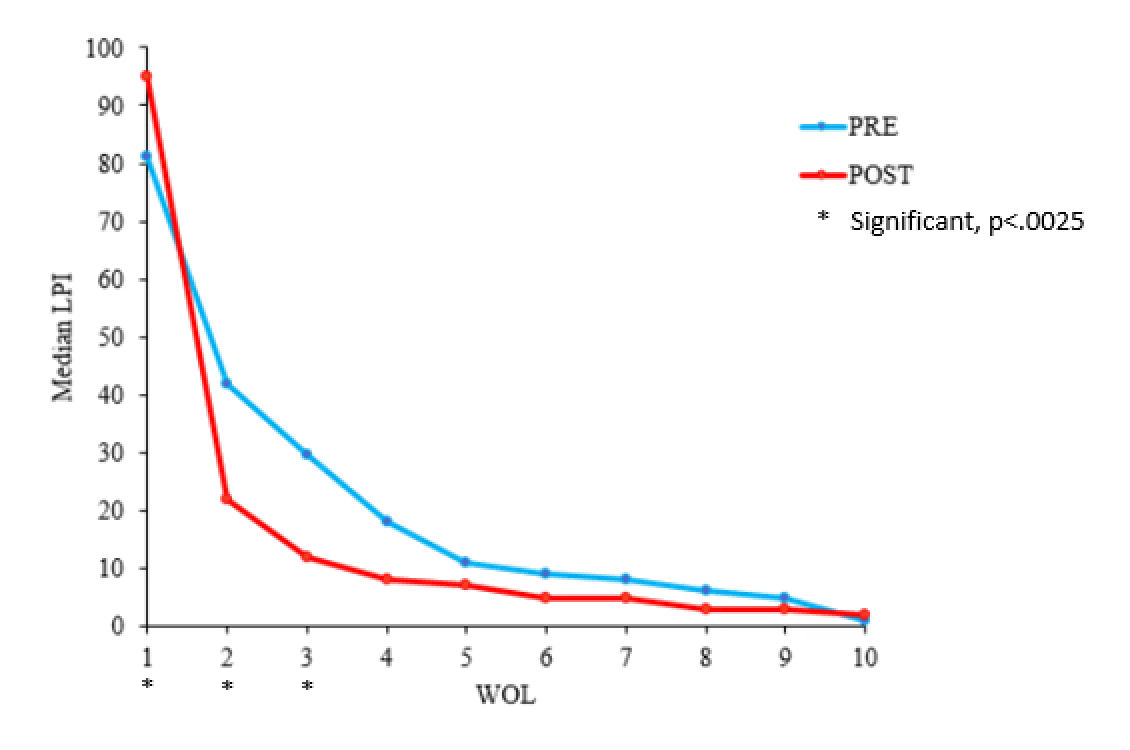
Results: A total of 130,998 labs were performed during the study period (PRE=60,711, POST=70,287). The median daily rate of labs per infant was significantly lower in the POST group overall and for GA subgroups 24-25 weeks and 28-29 weeks. The median number of labs per infant for WOL 2-3 was significantly lower in the POST group. A total of 1,602 transfusions were completed (PRE=1064, POST=601). Overall, 282 (79%) of infants received at least one transfusion during the NICU hospitalization, and 245 (69%) infants received two or more transfusions. Significant reductions in the POST group in median transfusions per infant in the subgroup analyses were observed for infants born 24-25 weeks and 26-27 weeks GA. Median lab and transfusion costs were significantly reduced in the POST group. The subgroup cost analyses revealed significant reductions in lab and transfusion costs for 3 of the 4 GA groups.Conclusion(s): This study suggest that limiting labs may be a promising strategy to reduce the number of transfusions and NICU costs for VLBW infants. The implementation of a checklist guiding team awareness of lab orders may be a promising method to reduce the number of labs, transfusions, and their associated costs.
Table 1: Results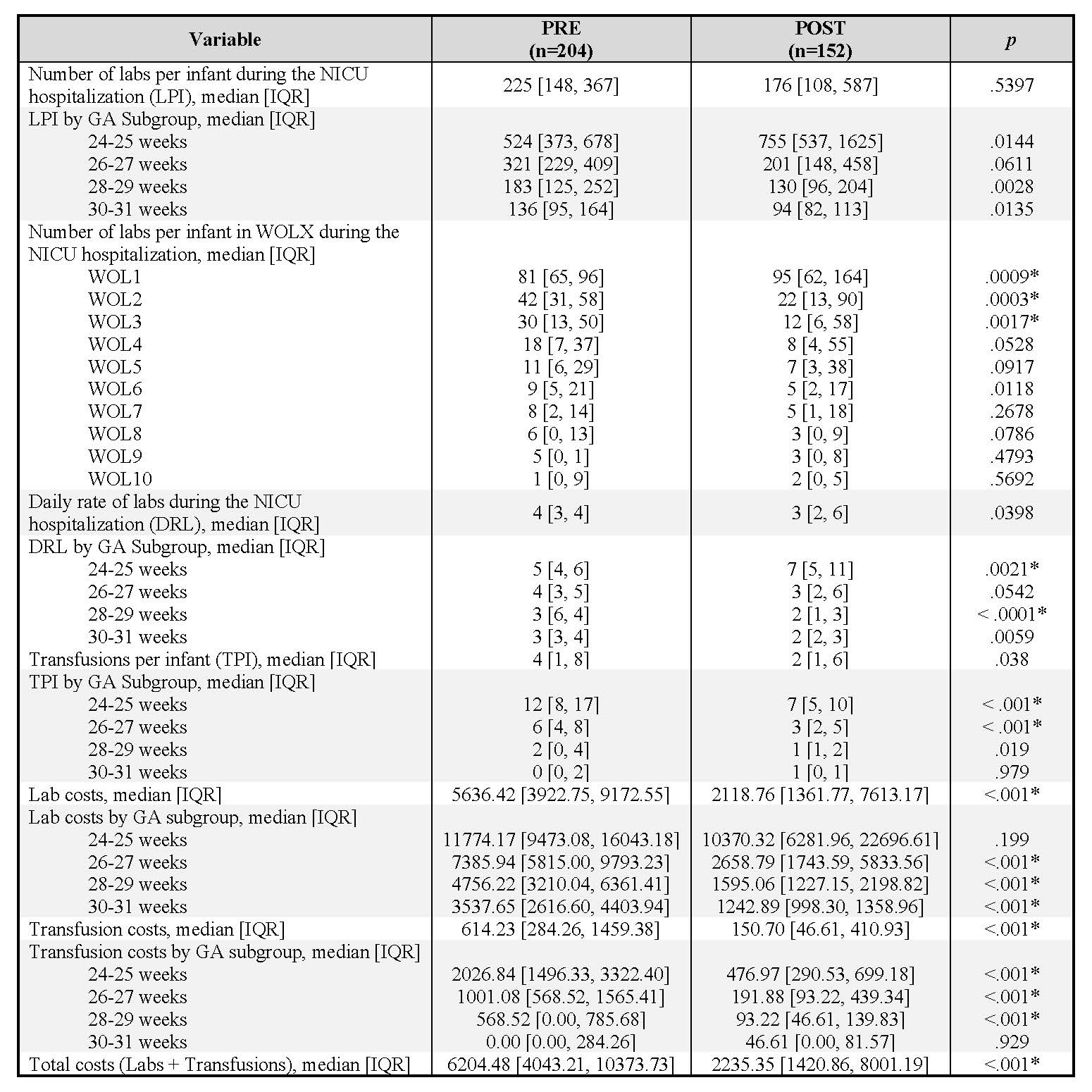
Figure 1: Median labs per infant (LPI) by week of life (WOL)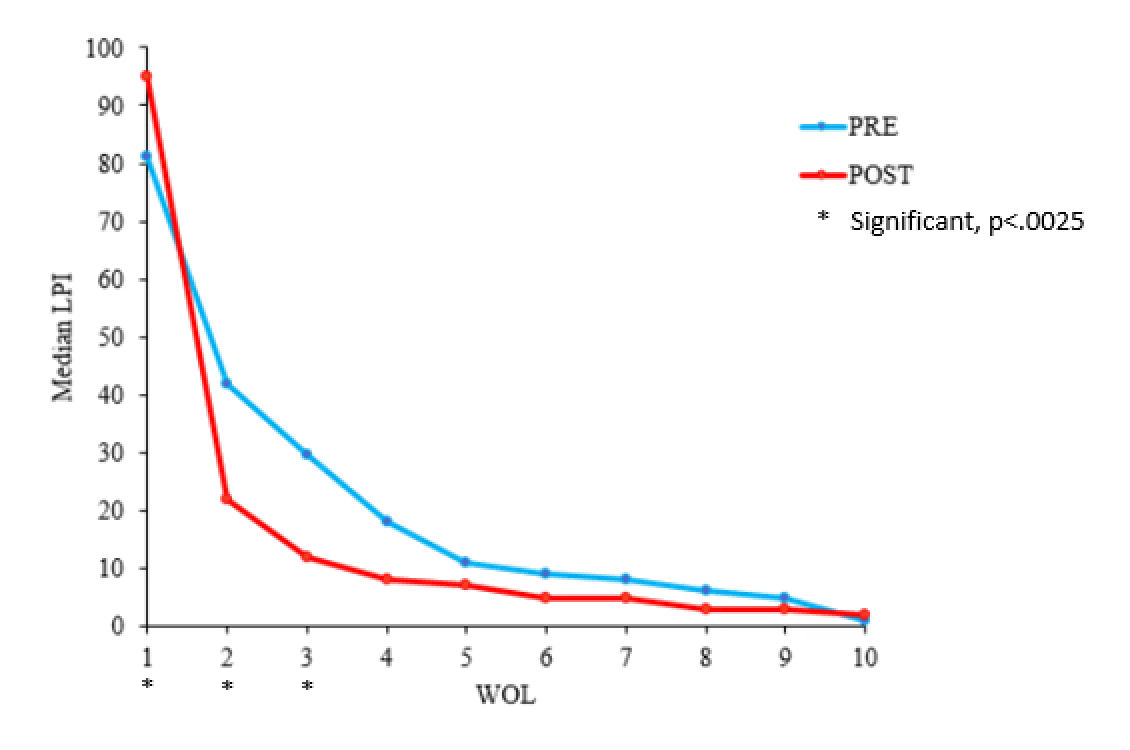
Objective: To compare the frequency of labs, blood transfusions, and associated costs for VLBW infants hospitalized in the NICU, pre- and post- checklist implementation.
Design/Methods: This retrospective study included 356 VLBW infants admitted to the NICU in 2008-2010 (pre-checklist; PRE) or 2018-2019 (post-checklist; POST). Data for the PRE group were obtained from a prospective cohort study. POST group data were obtained from electronic medical record chart review and the hospital financial records system. Outcomes were analyzed by time period, and by subgroups of gestational age (GA) and week of life (WOL). Costs were standardized to 2020 US dollars. Nonparametric tests were used to compare the outcomes between time periods and for subgroup analyses. Bonferroni correction was used to adjust the significance levels for multiple comparisons.
Results: A total of 130,998 labs were performed during the study period (PRE=60,711, POST=70,287). The median daily rate of labs per infant was significantly lower in the POST group overall and for GA subgroups 24-25 weeks and 28-29 weeks. The median number of labs per infant for WOL 2-3 was significantly lower in the POST group. A total of 1,602 transfusions were completed (PRE=1064, POST=601). Overall, 282 (79%) of infants received at least one transfusion during the NICU hospitalization, and 245 (69%) infants received two or more transfusions. Significant reductions in the POST group in median transfusions per infant in the subgroup analyses were observed for infants born 24-25 weeks and 26-27 weeks GA. Median lab and transfusion costs were significantly reduced in the POST group. The subgroup cost analyses revealed significant reductions in lab and transfusion costs for 3 of the 4 GA groups.Conclusion(s): This study suggest that limiting labs may be a promising strategy to reduce the number of transfusions and NICU costs for VLBW infants. The implementation of a checklist guiding team awareness of lab orders may be a promising method to reduce the number of labs, transfusions, and their associated costs.
Table 1: Results
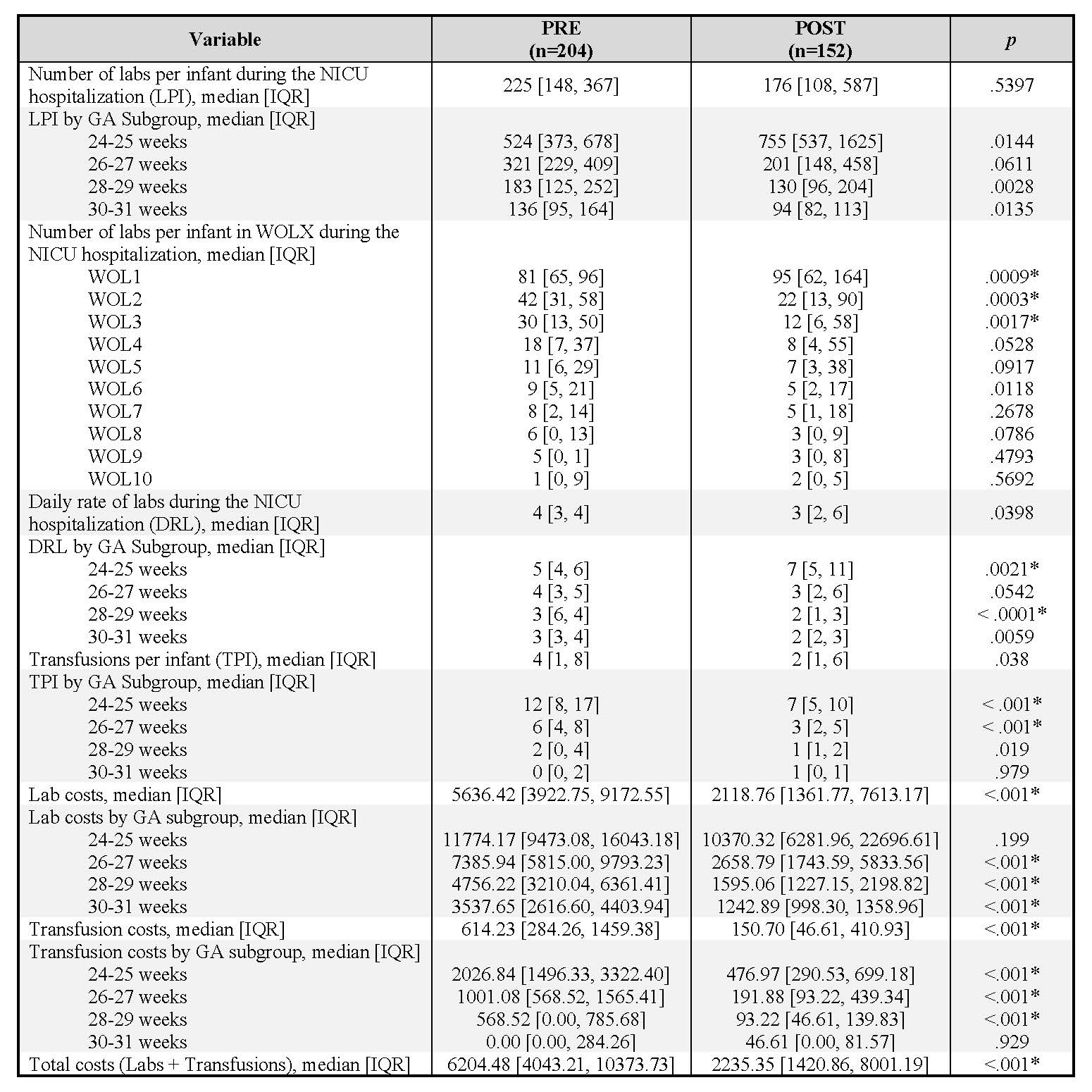
Figure 1: Median labs per infant (LPI) by week of life (WOL)