Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement IV: Respiratory and Temperature Regulation
372 - A Quality Improvement Project to Reduce the Incidence of Hypothermia in Newborns
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 372
Publication Number: 372.434
Publication Number: 372.434
Kelsey Legro, OSF Healthcare Children's Hospital of Illinois, Peoria, IL, United States; Ashley Fischer, University of Illinois College of Medicine Peoria; OSF Children's Hospital of Illinois, Peoria, IL, United States; Gretchen Kopec, OSF Healthcare Children's Hospital of Illinois, Peoria, IL, United States; Shelly Shallat, OSF Healthcare Children's Hospital of Illinois, Peoria, IL, United States
Kelsey Legro, DO
Resident
OSF Healthcare Children's Hospital of Illinois
Peoria, Illinois, United States
Presenting Author(s)
Background: Hypothermia is an important cause of morbidity and mortality in newborns. Our institution has a high incidence of hypothermia; higher than other type C centers in Vermont Oxford Network.
Objective: A multidisciplinary quality improvement project was implemented with the aim to reduce the incidence of hypothermia < 97 F in the first two hours of life in all inborn newborns from a baseline of 16.2% to 12% by June 2021.
Design/Methods: A multidisciplinary group including personnel from obstetrics, nursery, NICU, and anesthesia worked to create process maps and a driver diagram based upon the four major sources of heat loss. Five plan-do-study-act cycles were completed over six months. NICU staff utilized debriefing forms to identify further change ideas and address issues with subsequent cycles. Major changes included increasing baseline temperatures in operating rooms, vaginal delivery rooms, and resuscitation room and ensuring they remained above the designated temperature. Education was provided on using warmed blankets over scales and isolettes while in transport. It was found that the disposable thermometers the institution had been using were consistently inaccurate and therefore were replaced. Throughout the project, education was provided to staff and monthly meetings were held to discuss progress. The primary outcome measure was the incidence of hypothermia < 97 F in the first two hours of life. Hyperthermia (core temperature >99.7F) and OR temperatures above JCAHO standards were designated as the balancing measure. Process measures included monitoring operating room, vaginal delivery room, and resuscitation room temperatures.
Results: The incidence of hypothermia in the first two hours of life was reduced from a baseline of 16.2% to 5.5% within the designated time frame and results were sustained through November (Figure 1). When further broken down by gestational age, the biggest improvement was identified in term babies while there was no significant improvement in the preterm or late-preterm populations (Figure 2). Incidentally, a racial disparity was discovered with black babies having higher baseline hypothermia rates, which improved over time, however still remains (Figure 3). The balancing measure, the incidence of hyperthermia, remained unchanged.Conclusion(s): The incidence of hypothermia < 97F in newborns in the first two hours of life was successfully reduced. Future directions include raising the goal to 97.7 F, tackling the premature infants, and addressing the racial disparity.
Figure 1: Total Incidence of Hypothermia.png) The total incidence of hypothermia in the first two hours of life was successfully reduced from 16.2% to 5.5% within the designated timeframe.
The total incidence of hypothermia in the first two hours of life was successfully reduced from 16.2% to 5.5% within the designated timeframe.
Figure 2: Hypothermia by Gestational Age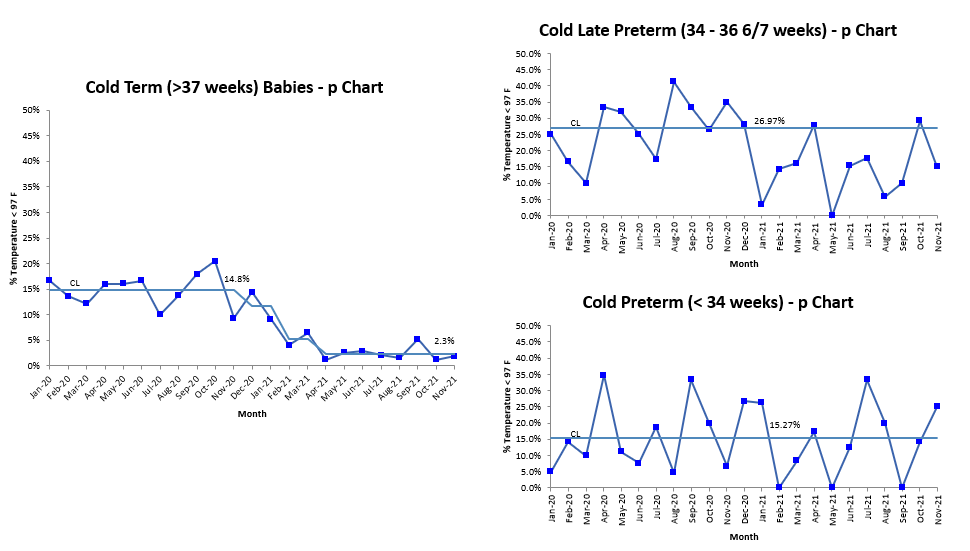 When broken down by gestational age, the greatest improvement was in the term babies while there was no improvement in the late pre-term or preterm babies.
When broken down by gestational age, the greatest improvement was in the term babies while there was no improvement in the late pre-term or preterm babies.
Objective: A multidisciplinary quality improvement project was implemented with the aim to reduce the incidence of hypothermia < 97 F in the first two hours of life in all inborn newborns from a baseline of 16.2% to 12% by June 2021.
Design/Methods: A multidisciplinary group including personnel from obstetrics, nursery, NICU, and anesthesia worked to create process maps and a driver diagram based upon the four major sources of heat loss. Five plan-do-study-act cycles were completed over six months. NICU staff utilized debriefing forms to identify further change ideas and address issues with subsequent cycles. Major changes included increasing baseline temperatures in operating rooms, vaginal delivery rooms, and resuscitation room and ensuring they remained above the designated temperature. Education was provided on using warmed blankets over scales and isolettes while in transport. It was found that the disposable thermometers the institution had been using were consistently inaccurate and therefore were replaced. Throughout the project, education was provided to staff and monthly meetings were held to discuss progress. The primary outcome measure was the incidence of hypothermia < 97 F in the first two hours of life. Hyperthermia (core temperature >99.7F) and OR temperatures above JCAHO standards were designated as the balancing measure. Process measures included monitoring operating room, vaginal delivery room, and resuscitation room temperatures.
Results: The incidence of hypothermia in the first two hours of life was reduced from a baseline of 16.2% to 5.5% within the designated time frame and results were sustained through November (Figure 1). When further broken down by gestational age, the biggest improvement was identified in term babies while there was no significant improvement in the preterm or late-preterm populations (Figure 2). Incidentally, a racial disparity was discovered with black babies having higher baseline hypothermia rates, which improved over time, however still remains (Figure 3). The balancing measure, the incidence of hyperthermia, remained unchanged.Conclusion(s): The incidence of hypothermia < 97F in newborns in the first two hours of life was successfully reduced. Future directions include raising the goal to 97.7 F, tackling the premature infants, and addressing the racial disparity.
Figure 1: Total Incidence of Hypothermia
.png) The total incidence of hypothermia in the first two hours of life was successfully reduced from 16.2% to 5.5% within the designated timeframe.
The total incidence of hypothermia in the first two hours of life was successfully reduced from 16.2% to 5.5% within the designated timeframe.Figure 2: Hypothermia by Gestational Age
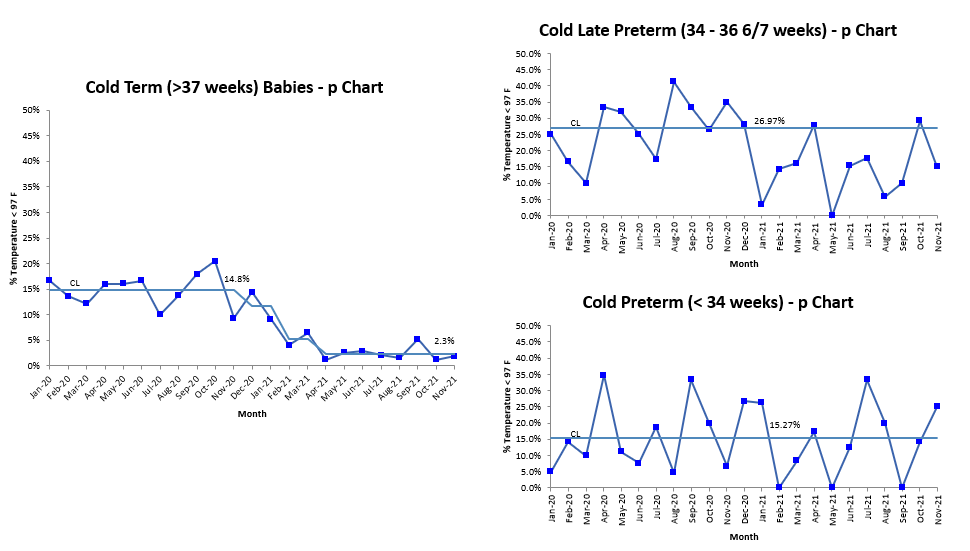 When broken down by gestational age, the greatest improvement was in the term babies while there was no improvement in the late pre-term or preterm babies.
When broken down by gestational age, the greatest improvement was in the term babies while there was no improvement in the late pre-term or preterm babies.