Neonatal Quality Improvement
Category: Abstract Submission
Neonatal Quality Improvement V
386 - A quality improvement study to improve rate of expressed breastmilk at discharge at a community level III NICU between 2020-2021 during the challenging COVID pandemic.
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 386
Publication Number: 386.435
Publication Number: 386.435
Sneha Taylor, CHOC Children's Hospital of Orange County, Chino Hills, CA, United States; Susan Wilkinson, Pomona Valley Hospital Medical Center, Pomona, CA, United States; Maria G. Palacios, Pomona Valley Hospital Medical Center, Fontana, CA, United States

Sneha Taylor, MD (she/her/hers)
Attending Neonatologist
Children's Hospital of Orange County, Orange, CA
Chinohills, California, United States
Presenting Author(s)
Background: Our NICU historically has had struggles prior to COVID to improve expressed breastmilk (EBM) at discharge rate given the culture of the unit. COVID pandemic made it worse and it became challenging to even sustain our rate.
Objective: Our aim was to revive the forgotten importance of EBM during COVID pandemic from 55% in 2019 to >60% by December 2021 by a relative change of 5% by implementing potentially better practices(PBP) in compliance with COVID policy, limited resources and inherent challenges with our NICU culture in promoting breastfeeding.
Design/Methods: Participants included all CPQCC eligible NICU infants including inborn, outborn and infants of a substance abuse mother.
In early 2020, we explored the barriers to meaningful breastfeeding, identified interventions and began with awareness and education. However, the COVID pandemic shifted the unit's priorities affecting implementation and reinforcement of our interventions.
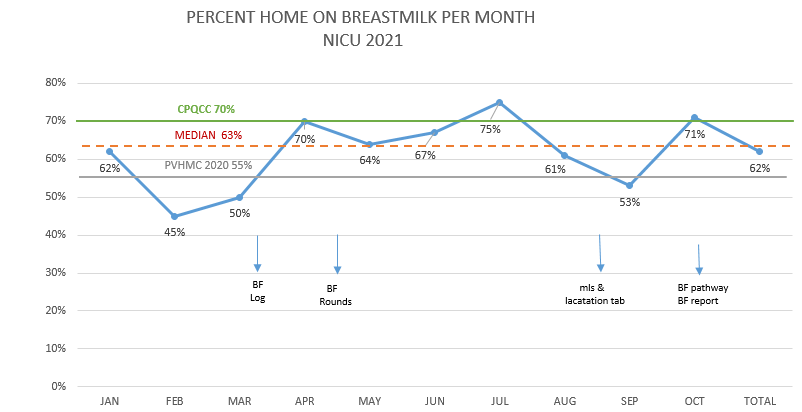
Nonetheless, we bounced back with double efforts and enthusiasm in 2021 with some key interventions such as a breastfeeding log to identify at risk mothers with low EBM supply; new EMR supporting accurate measurement of EBM inventory and progress of lactation journey; nightly team breastfeeding rounds ; implementing a new breastfeeding(BF) script and education for families, a new BF pathway to identify appropriate intervention by staff; and skin-skin to name a few.
Regular data collection, auditing, education, encouragement and reinforcement to staff performed. We measured the rate of EBM at discharge during 2020 and 2021.
Results: Our EBM at discharge rate remained unchanged at 55% by Dec 2020 showing no improvement since 2019. By Oct 2021, our EBM at discharge rate improved to 61.3%. Through this process we have identified barriers related to staffing, challenging hospital visitation policies, challenging home situations for parents during COVID causing less visits, lack of staff and parents’ confidence in performing and promoting skin-skin, and our inherent NICU culture.Conclusion(s): It has been a challenge for us to promote and sustain breastfeeding efforts to improve our EBM at discharge rate in general and more during COVID pandemic but with a consistent focus, education, encouragement, reassurance, multidisciplinary accountability and implementing better practices targeting areas of improvement we are able to improve our outcomes. However, succeeding at a California state level benchmark (70%) and sustainability is our new challenge.
Rate of EBM per month at discharge per month in 2021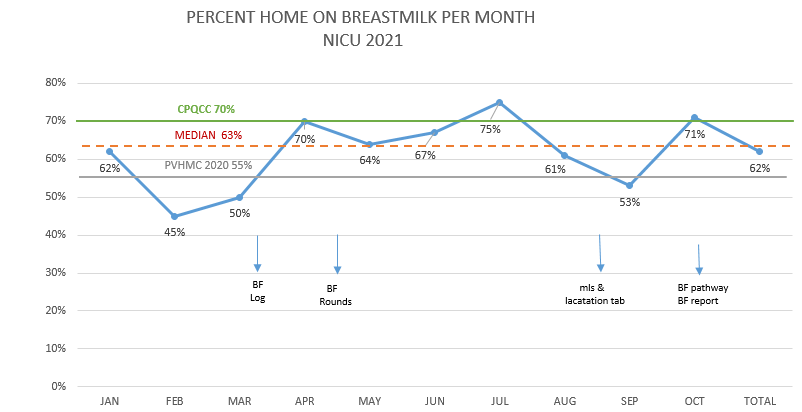
Objective: Our aim was to revive the forgotten importance of EBM during COVID pandemic from 55% in 2019 to >60% by December 2021 by a relative change of 5% by implementing potentially better practices(PBP) in compliance with COVID policy, limited resources and inherent challenges with our NICU culture in promoting breastfeeding.
Design/Methods: Participants included all CPQCC eligible NICU infants including inborn, outborn and infants of a substance abuse mother.
In early 2020, we explored the barriers to meaningful breastfeeding, identified interventions and began with awareness and education. However, the COVID pandemic shifted the unit's priorities affecting implementation and reinforcement of our interventions.
Nonetheless, we bounced back with double efforts and enthusiasm in 2021 with some key interventions such as a breastfeeding log to identify at risk mothers with low EBM supply; new EMR supporting accurate measurement of EBM inventory and progress of lactation journey; nightly team breastfeeding rounds ; implementing a new breastfeeding(BF) script and education for families, a new BF pathway to identify appropriate intervention by staff; and skin-skin to name a few.
Regular data collection, auditing, education, encouragement and reinforcement to staff performed. We measured the rate of EBM at discharge during 2020 and 2021.
Results: Our EBM at discharge rate remained unchanged at 55% by Dec 2020 showing no improvement since 2019. By Oct 2021, our EBM at discharge rate improved to 61.3%. Through this process we have identified barriers related to staffing, challenging hospital visitation policies, challenging home situations for parents during COVID causing less visits, lack of staff and parents’ confidence in performing and promoting skin-skin, and our inherent NICU culture.Conclusion(s): It has been a challenge for us to promote and sustain breastfeeding efforts to improve our EBM at discharge rate in general and more during COVID pandemic but with a consistent focus, education, encouragement, reassurance, multidisciplinary accountability and implementing better practices targeting areas of improvement we are able to improve our outcomes. However, succeeding at a California state level benchmark (70%) and sustainability is our new challenge.
Rate of EBM per month at discharge per month in 2021