Adolescent Medicine: Disordered Eating
Category: Abstract Submission
Adolescent Medicine III
202 - Eating Disorder Hospitalizations: Disparities Among Adolescent and Young Adult Patients in California, 2014-2018
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 202
Publication Number: 202.400
Publication Number: 202.400
Lauren Wozniak, Stanford University School of Medicine, Redwood City, CA, United States; Rachel L. Goldstein, Stanford University School of Medicine, Palo Alto, CA, United States; Olga Saynina, Stanford University School of Medicine, Palo Alto, CA, United States; Nancy Ewen Wang, Stanford School of Medicine, Palo Alto, CA, United States; Susan Fernandes, Stanford University School of Medicine, Stanford, CA, United States; Ananta Addala, Stanford University, Stanford, CA, United States; Paul H. Wise, Stanford University, stanford, CA, United States; Lisa J. Chamberlain, Stanford University School of Medicine, Stanford, CA, United States

Lauren Wozniak, MD MPH
Clinical Fellow
Stanford University School of Medicine
Redwood City, California, United States
Presenting Author(s)
Background: Eating disorders (EDs) impact 9% of the population and have the highest mortality of any mental illness. Peak age of onset for EDs is 13-22 years and they occur in all racial and socioeconomic groups similarly. 20-40% of hospitalized patients will require readmission, which is associated with poorer outcomes. It is unknown how socioeconomic factors impact admission and readmission rates.
Objective: To examine how sociodemographic factors influence admission and readmission rates for adolescent and young adults (AYA) with EDs.
Design/Methods: This 5-year retrospective analysis of ED hospital discharges utilized California’s Office of Statewide Health Planning and Development (OSHPD) database, 2014-2018. Patients included were 10-26 years-old and hospitalized in acute care hospitals with an ED related ICD-10. Analyses include descriptive statistics as well as chi-square test to explore differences in admissions and readmissions over time. P < 0.05 was deemed statistically significant. Multivariable logistic regression generated odds ratios (OR) and 95% confidence limits (Cl) for factors associated with hospital readmissions.
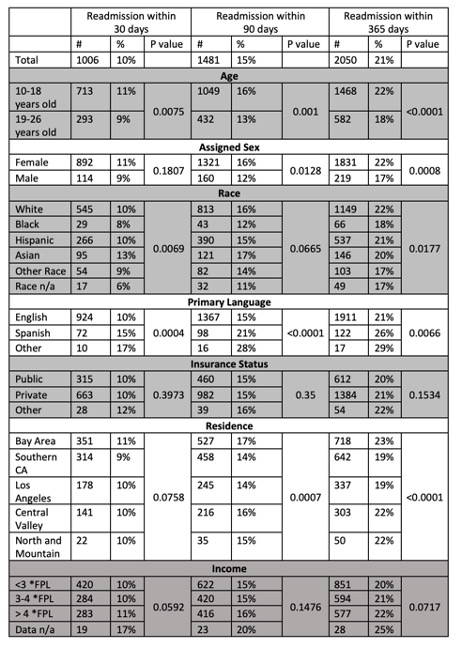
Results: There were 9,767 total ED related admissions in the state of California in the study cohort (Table 1). The majority of admissions were female (87%) and white (54%), followed by Hispanic (26%), Asian (7%), other race (6%), black (4%), and race n/a (3%). The vast majority were English speaking (95%) and privately insured (66%), with 44% living below three times federal poverty level (FPL). It was reassuring that there was no difference in readmission rates at 30, 90, and 365 days from index admission based on insurance type (P=0.39, 0.35, 0.15) or poverty level (P=0.06, 0.15, 0.07)(Table 2). However, non-English speaking patients were more likely to be readmitted at all time intervals (P=0.0004, < 0.0001, 0.0066). Multivariate analysis suggested that Spanish language was associated with higher rates of readmission (OR = 1.75, CI 1.30-2.37) compared to English. There was significant regional variation in readmission rates as well with patients in Southern California / LA regions less likely to be readmitted compared to the Bay Area (Table 3).Conclusion(s):
We found that primary Spanish language was associated with higher rates of ED readmission and that significant regional readmission variation exists. The next steps include evaluation of barriers that might be driving inequitable readmission rates.
Table 1: Eating disorder related admissions in the state of California between the years 2014-2017 for patients aged 10-26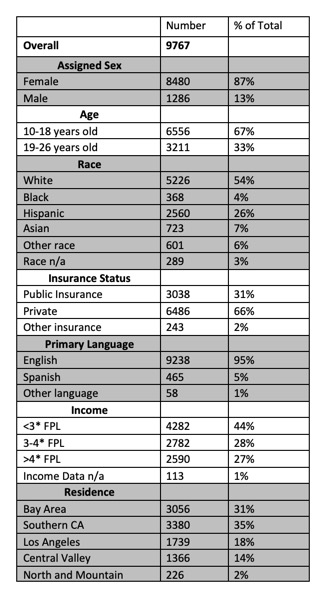
Table 2: Readmissions at 30, 90, and 365 days for patients discharged with eating disorder related diagnoses in top 5 ICD-10 codes between 2014-2018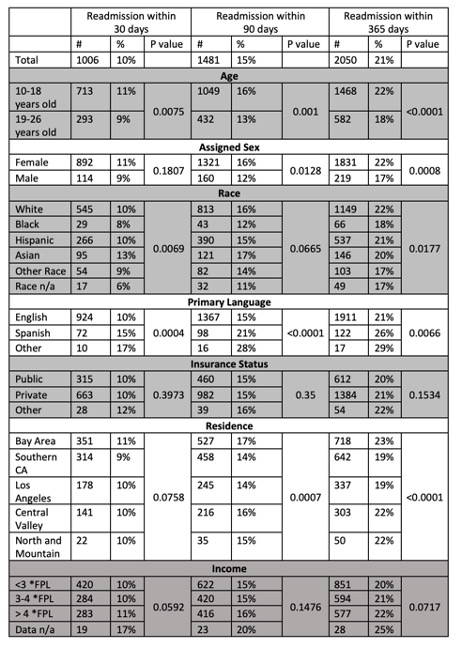
Objective: To examine how sociodemographic factors influence admission and readmission rates for adolescent and young adults (AYA) with EDs.
Design/Methods: This 5-year retrospective analysis of ED hospital discharges utilized California’s Office of Statewide Health Planning and Development (OSHPD) database, 2014-2018. Patients included were 10-26 years-old and hospitalized in acute care hospitals with an ED related ICD-10. Analyses include descriptive statistics as well as chi-square test to explore differences in admissions and readmissions over time. P < 0.05 was deemed statistically significant. Multivariable logistic regression generated odds ratios (OR) and 95% confidence limits (Cl) for factors associated with hospital readmissions.
Results: There were 9,767 total ED related admissions in the state of California in the study cohort (Table 1). The majority of admissions were female (87%) and white (54%), followed by Hispanic (26%), Asian (7%), other race (6%), black (4%), and race n/a (3%). The vast majority were English speaking (95%) and privately insured (66%), with 44% living below three times federal poverty level (FPL). It was reassuring that there was no difference in readmission rates at 30, 90, and 365 days from index admission based on insurance type (P=0.39, 0.35, 0.15) or poverty level (P=0.06, 0.15, 0.07)(Table 2). However, non-English speaking patients were more likely to be readmitted at all time intervals (P=0.0004, < 0.0001, 0.0066). Multivariate analysis suggested that Spanish language was associated with higher rates of readmission (OR = 1.75, CI 1.30-2.37) compared to English. There was significant regional variation in readmission rates as well with patients in Southern California / LA regions less likely to be readmitted compared to the Bay Area (Table 3).Conclusion(s):
We found that primary Spanish language was associated with higher rates of ED readmission and that significant regional readmission variation exists. The next steps include evaluation of barriers that might be driving inequitable readmission rates.
Table 1: Eating disorder related admissions in the state of California between the years 2014-2017 for patients aged 10-26
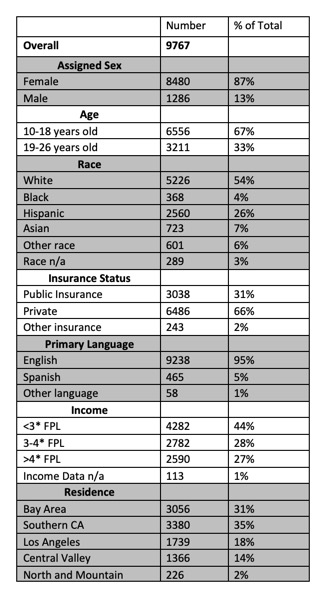
Table 2: Readmissions at 30, 90, and 365 days for patients discharged with eating disorder related diagnoses in top 5 ICD-10 codes between 2014-2018