Neonatal General
Category: Abstract Submission
Neonatology General 9: Congenital Anomalies - CV
303 - Esophageal Atresia with or without Tracheoesophageal Fistula: How often is a genetic evaluation performed and what are we finding?
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 303
Publication Number: 303.441
Publication Number: 303.441
Divya Khattar, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States; Kristen Suhrie, Indiana University School of Medicine, Indianapolis, IN, United States

Divya Khattar, MD (she/her/hers)
Clinical Fellow
CCHMC
Cincinnati, Ohio, United States
Presenting Author(s)
Background: Esophageal atresia (EA) with or without Tracheoesophageal Fistula (TEF) has a reported incidence of 1 in 3500 live births and requires intensive care and surgery in the neonatal period. It is reported to occur both as an isolated defect and with a variety of other anomalies. Historically, a genetic cause has not been identified for most of the cases of EA/TEF.
Objective: We conducted this study to find the prevalence of a molecularly confirmed genetic etiology of EA/TEF in our cohort, focusing on genetic evaluation, diagnostic yield, and clinical outcomes of these neonates.
Design/Methods: A retrospective cohort study was performed for all patients admitted to the Cincinnati Children’s Hospital Medical Center (CCHMC) NICU between January 2013 to December 2019 with a diagnosis of EA/TEF to determine the frequency of associated anomalies, frequency, and type of genetic evaluations and diagnoses, and outcomes at NICU discharge.
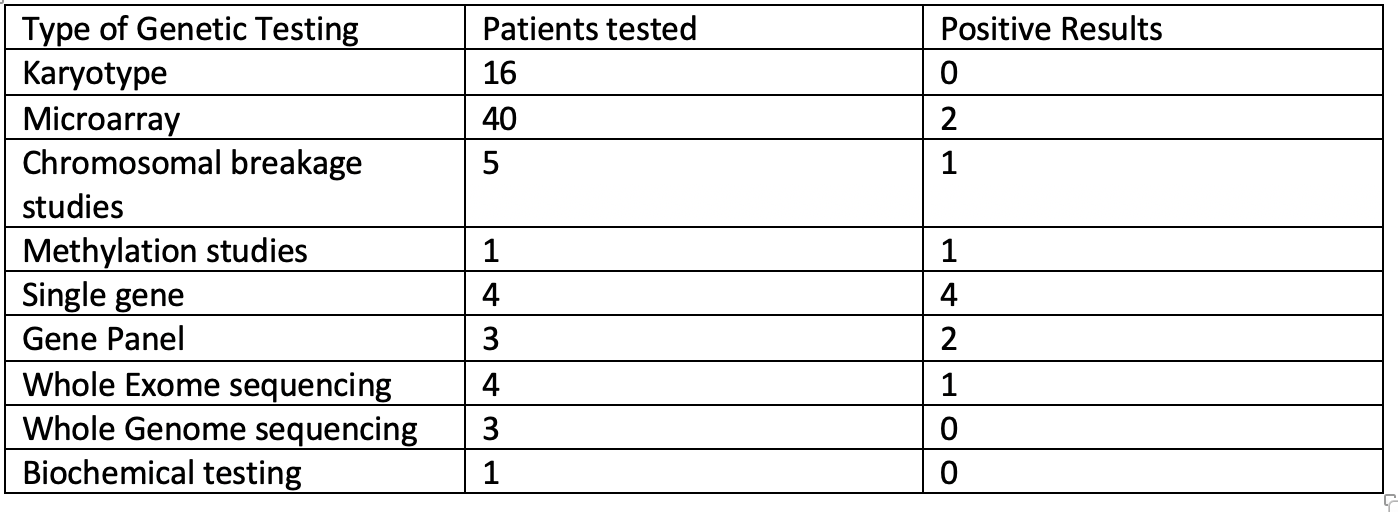
Results: Sixty-eight infants met inclusion criteria. A majority were male (62%), born at >37 weeks’ gestation (53%), had EA with distal TEF (79%), and had other associated congenital anomalies (78%). A medical genetics consult was performed for 47 (69%) infants and 44 underwent some form of molecular or cytogenetic testing. The most common testing performed was microarray (59%), karyotype (16%), and only 7 patients (10%) underwent whole exome/genome sequencing. Five unique genetic diagnoses were made for 9 (13%) patients in our cohort. Overall, the cohort suffered a high rate of morbidity and mortality during their NICU say. Twelve infants (18%) died prior to NICU discharge. Of those surviving, 40 (71%) had a primary repair, 37 (66%) required G or GJ feedings at NICU discharge, and 8 (14%) were discharged on respiratory support. The average length of stay for patients with an identified genetic etiology of EA/TEF was longer, 140 days compared to 64 days.Conclusion(s): In this high-risk cohort of EA/TEF patients cared for at a quaternary NICU, a majority had some form of a genetic evaluation, but a minority underwent WES, which is now the recommended test for all infants with a congenital anomaly per the American College of Medical Genetics. Given the diagnostic yield for WES in infants with congenital anomalies is best estimated to be 30%, we predict that as many as 11 patients may have had an undiagnosed genetic disorder at NICU discharge. Standardization of genetic testing for this cohort of patients can help better direct care, identify risk for increased morbidity and mortality, and give better expectations for long-term outcomes.
Demographics of patients with EA with or without TEF.png)
Genetic Testing performed for patients with EA with or without TEF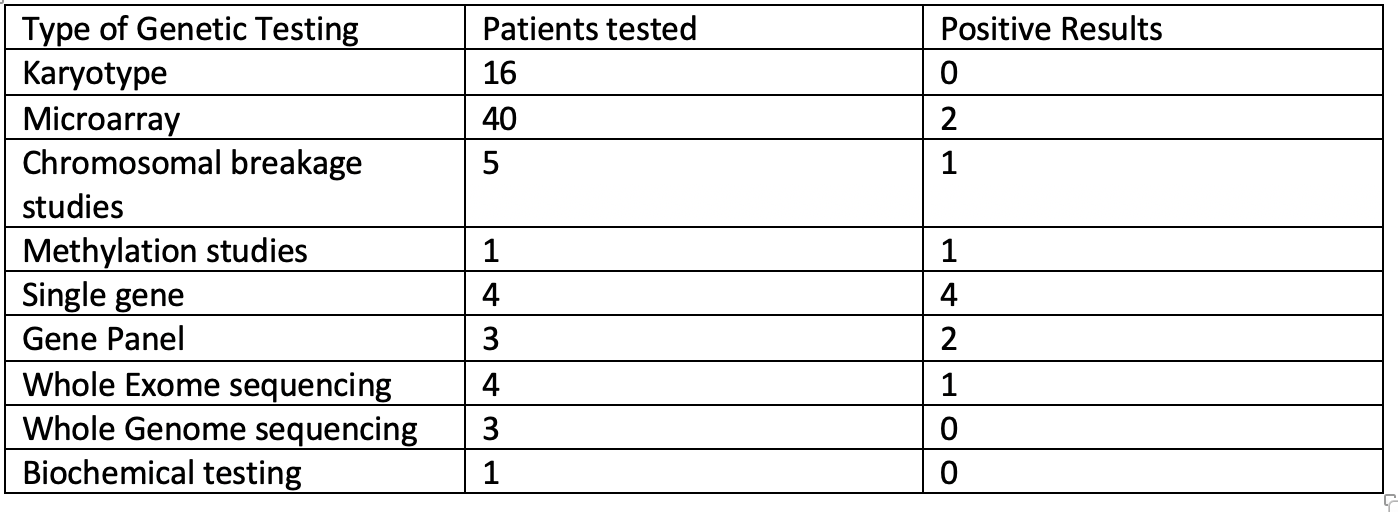
Objective: We conducted this study to find the prevalence of a molecularly confirmed genetic etiology of EA/TEF in our cohort, focusing on genetic evaluation, diagnostic yield, and clinical outcomes of these neonates.
Design/Methods: A retrospective cohort study was performed for all patients admitted to the Cincinnati Children’s Hospital Medical Center (CCHMC) NICU between January 2013 to December 2019 with a diagnosis of EA/TEF to determine the frequency of associated anomalies, frequency, and type of genetic evaluations and diagnoses, and outcomes at NICU discharge.
Results: Sixty-eight infants met inclusion criteria. A majority were male (62%), born at >37 weeks’ gestation (53%), had EA with distal TEF (79%), and had other associated congenital anomalies (78%). A medical genetics consult was performed for 47 (69%) infants and 44 underwent some form of molecular or cytogenetic testing. The most common testing performed was microarray (59%), karyotype (16%), and only 7 patients (10%) underwent whole exome/genome sequencing. Five unique genetic diagnoses were made for 9 (13%) patients in our cohort. Overall, the cohort suffered a high rate of morbidity and mortality during their NICU say. Twelve infants (18%) died prior to NICU discharge. Of those surviving, 40 (71%) had a primary repair, 37 (66%) required G or GJ feedings at NICU discharge, and 8 (14%) were discharged on respiratory support. The average length of stay for patients with an identified genetic etiology of EA/TEF was longer, 140 days compared to 64 days.Conclusion(s): In this high-risk cohort of EA/TEF patients cared for at a quaternary NICU, a majority had some form of a genetic evaluation, but a minority underwent WES, which is now the recommended test for all infants with a congenital anomaly per the American College of Medical Genetics. Given the diagnostic yield for WES in infants with congenital anomalies is best estimated to be 30%, we predict that as many as 11 patients may have had an undiagnosed genetic disorder at NICU discharge. Standardization of genetic testing for this cohort of patients can help better direct care, identify risk for increased morbidity and mortality, and give better expectations for long-term outcomes.
Demographics of patients with EA with or without TEF
.png)
Genetic Testing performed for patients with EA with or without TEF