Emergency Medicine: All Areas
Category: Abstract Submission
Emergency Medicine XII
19 - Evaluation of a Fast-Screening Brain MRI protocol in a Pediatric Emergency Department
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 19
Publication Number: 19.405
Publication Number: 19.405
Richard F. Latuska, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Naomi Hughes, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States; Jessica A. Saunders, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Marissa Anto, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Arastoo Vossough, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Madeline Chadehumbe, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Jane Lavelle, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States

Richard F. Latuska, Jr., MD
Pediatric Emergency Medicine Fellow
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Obtaining neuroimaging in a pediatric Emergency Department (PED) poses a challenging risk versus benefit analysis given the risks of radiation-induced cancer with CT scans compared to the long scan times, often requiring sedation, with conventional magnetic resonance imaging (MRI). Advances have been made in MRI protocols, commonly referred as a fast-screening brain MRI’s (fsMRI), particularly for evaluation of hydrocephalus in VP shunts, but there is limited data on the effectiveness of their use in evaluation of non-traumatic neurologic complaints such as headache, seizure, altered mental status, or syncope.
Objective: The primary objective of this study was to document the frequency of and indications for which a fsMRI protocol was obtained for the evaluation of non-traumatic neurologic complaints in a PED and the incidence of clinically significant abnormal findings detected. Secondary objectives were to review various patient characteristics, process metrics, and radiographic and clinical outcomes.
Design/Methods: A retrospective electronic medical record review was conducted on all patients who presented to the PED between October 2018 - October 2019 and had a fsMRI obtained. Any abnormal fsMRI impressions were reviewed by group of physicians from pediatric emergency medicine, neurology, and neuroradiology to determine which were considered ‘clinically significant’, defined as findings felt to require further clinical intervention, follow-up, or management.
Results: A total of 418 fsMRIs were obtained over a one year period. Baseline patient demographics are listed in Table 1. The median time to completion for the fsMRI was 16 min (range 3 – 84 min). Sedation (whether po, IN, or IV) was required for 8.9% of patients (Figure 1). The most common indication was headache (n = 276, 42.9%) and over half of these patients had at least one other associated symptom (n=150) or was described as ‘positional’ in nature (n=9). An abnormal result was reported in 28% of cases (n=171) with 11.2% of those (n=47) considered ‘clinically significant’ (listed in Table 2). Only 1.4% of patients had follow-up imaging within three months that revealed an abnormality not detected on the initial fsMRI, none of which required urgent intervention. Conclusion(s): Results suggest this technique is feasible as a fast and successful tool in a PED for screening patients with non-traumatic neurologic complaints across a wide age range of patients. It has been able to detect a variety of underlying pathology with low frequency of missed findings or need for conversion to different neuroimaging or short-term follow-up exams.
Table 1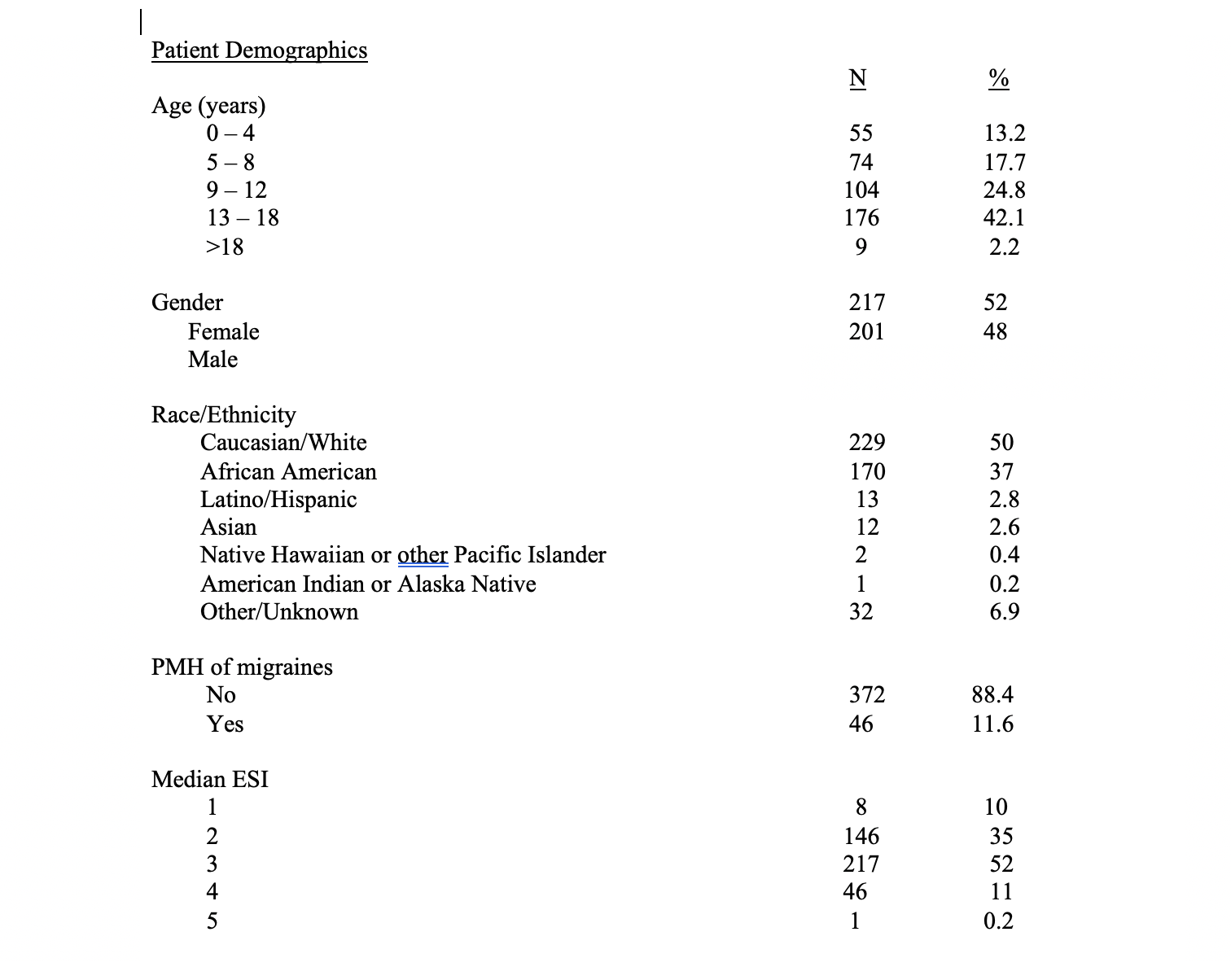 Demographic Characteristics of Patients Undergoing Evaluation with a Fast-Screening Brain MRI
Demographic Characteristics of Patients Undergoing Evaluation with a Fast-Screening Brain MRI
Table 1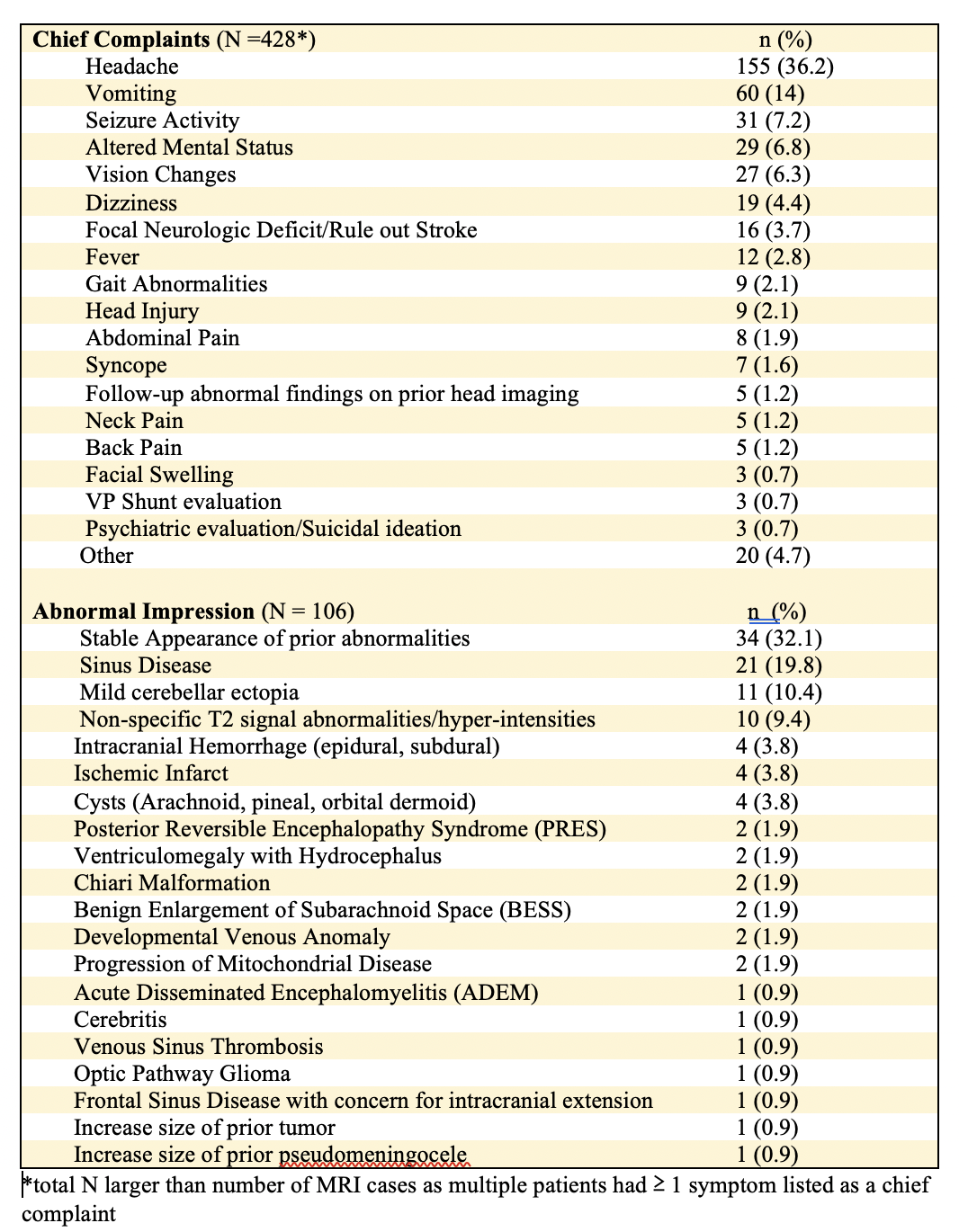 Neurologic indications identified for patients undergoing evaluation with a fast-screening brain MRI
Neurologic indications identified for patients undergoing evaluation with a fast-screening brain MRI
Objective: The primary objective of this study was to document the frequency of and indications for which a fsMRI protocol was obtained for the evaluation of non-traumatic neurologic complaints in a PED and the incidence of clinically significant abnormal findings detected. Secondary objectives were to review various patient characteristics, process metrics, and radiographic and clinical outcomes.
Design/Methods: A retrospective electronic medical record review was conducted on all patients who presented to the PED between October 2018 - October 2019 and had a fsMRI obtained. Any abnormal fsMRI impressions were reviewed by group of physicians from pediatric emergency medicine, neurology, and neuroradiology to determine which were considered ‘clinically significant’, defined as findings felt to require further clinical intervention, follow-up, or management.
Results: A total of 418 fsMRIs were obtained over a one year period. Baseline patient demographics are listed in Table 1. The median time to completion for the fsMRI was 16 min (range 3 – 84 min). Sedation (whether po, IN, or IV) was required for 8.9% of patients (Figure 1). The most common indication was headache (n = 276, 42.9%) and over half of these patients had at least one other associated symptom (n=150) or was described as ‘positional’ in nature (n=9). An abnormal result was reported in 28% of cases (n=171) with 11.2% of those (n=47) considered ‘clinically significant’ (listed in Table 2). Only 1.4% of patients had follow-up imaging within three months that revealed an abnormality not detected on the initial fsMRI, none of which required urgent intervention. Conclusion(s): Results suggest this technique is feasible as a fast and successful tool in a PED for screening patients with non-traumatic neurologic complaints across a wide age range of patients. It has been able to detect a variety of underlying pathology with low frequency of missed findings or need for conversion to different neuroimaging or short-term follow-up exams.
Table 1
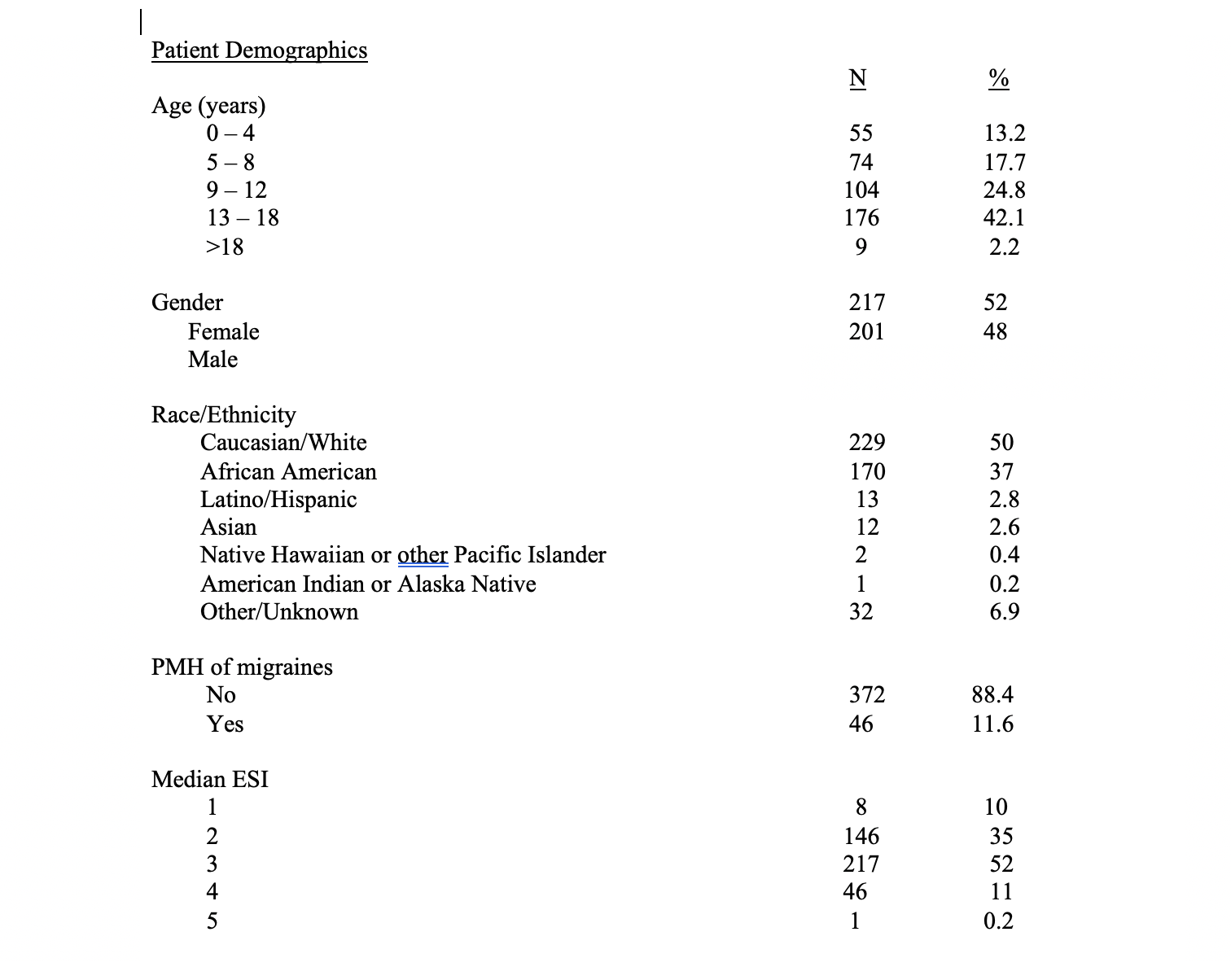 Demographic Characteristics of Patients Undergoing Evaluation with a Fast-Screening Brain MRI
Demographic Characteristics of Patients Undergoing Evaluation with a Fast-Screening Brain MRITable 1
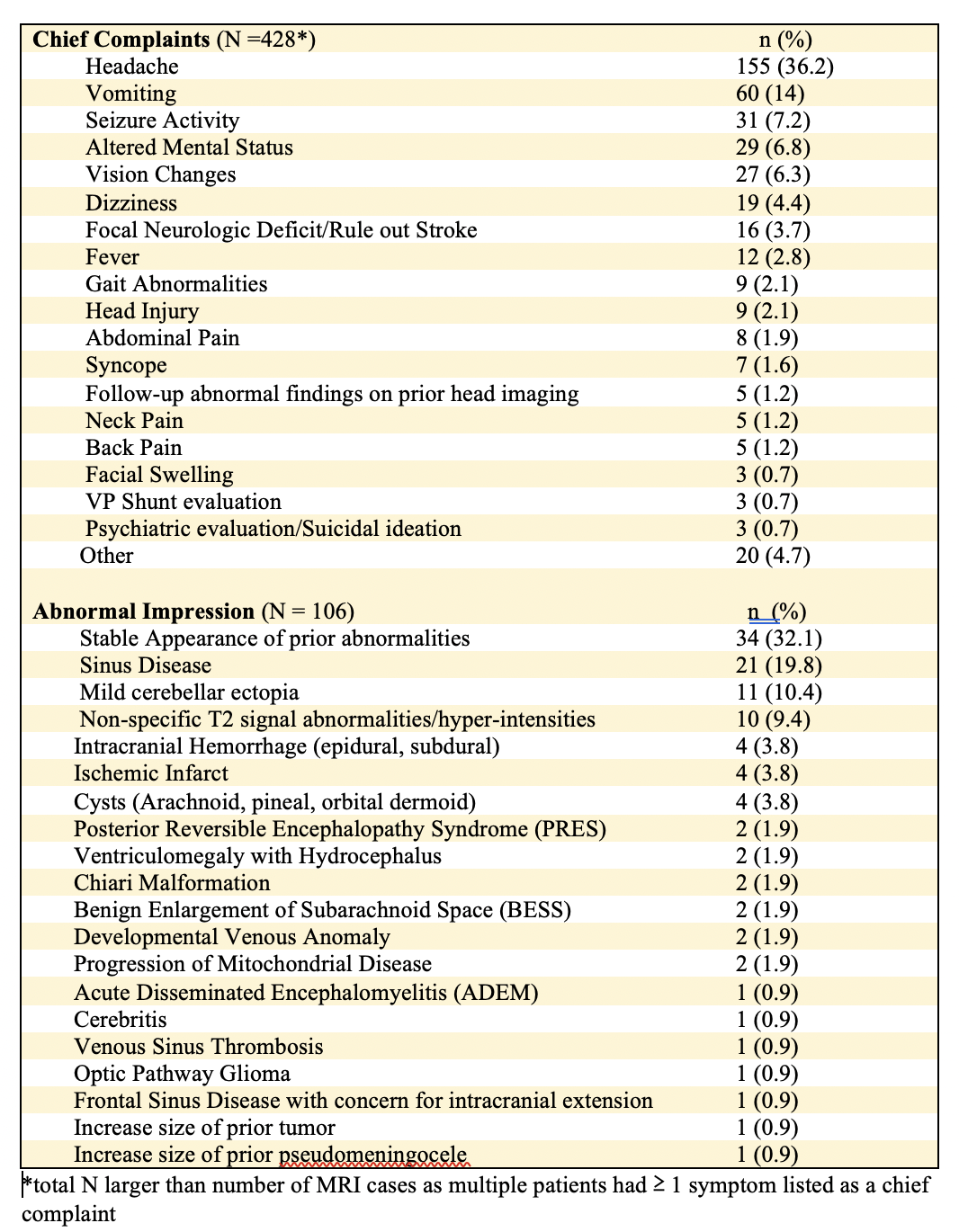 Neurologic indications identified for patients undergoing evaluation with a fast-screening brain MRI
Neurologic indications identified for patients undergoing evaluation with a fast-screening brain MRI