Neonatal Pulmonology
Category: Abstract Submission
Neonatal Pulmonology III: Molecular Markers and Clinical Prediction Models/Outcomes
447 - Higher Weight for Length is Associated with Increased Severity in Bronchopulmonary Dysplasia in Preterm Infants
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 447
Publication Number: 447.431
Publication Number: 447.431
Pradeep Alur, University of Mississippi Medical Center, Brandon, MS, United States; Renjithkumar Kalikkot, University of Mississippi School of Medicine, Madison, MS, United States; Kristen Harvey, University of Mississippi Medical Center School of Medicine, Columbus, MS, United States; Kyle Hart, University of Mississippi Medical Center, Brandon, MS, United States; Heather M. Williams, University of Mississippi Medical Center, Jackson, MS, United States; Wondwosen Yimer, University of Mississippi School of Population Health, Jackson, MS, United States
Pradeep Alur, MD (he/him/his)
Professor
Penn State Health
Camp Hill, PA, Pennsylvania, United States
Presenting Author(s)
Background: Obesity negatively impacts lung function in children and adolescents. Intergrowth 21st study concluded that weight for length (W/L) is more accurate in predicting fat-free mass and fat mass in premature infants. It is a widespread practice to restrict calories when the weight for length exceeds 50th percentiles in preterm infants with bronchopulmonary dysplasia (BPD). However, there are no studies correlating anthropometric measurements such as W/L or the body mass index (BMI) in preterm infants with higher Respiratory Severity Scores (RSS) in BPD.
Objective: To explore with a prospective observational study if higher W/L z-scores at 33-36 weeks of gestation correlate with higher RSS at 36 & 40 weeks corrected gestational age in preterm infants with BPD.
Design/Methods: Supported by NIH (Award # 1U54GM115428). Preterm infants born @ < 30 weeks requiring respiratory support for >2 days @ 30-33 weeks were enrolled. Weight, length, and head circumference were measured weekly. Data on mean calories & protein, W/L z-scores & BMI were collected. RSS was calculated as per the STOP-ROP trial. BPD was defined as per the NICHD BPD workshop published in February 2018. Data were analyzed using descriptive and inferential statistics. Linear mixed model regression was used to study the relationship between the continuous variables with potential covariates.
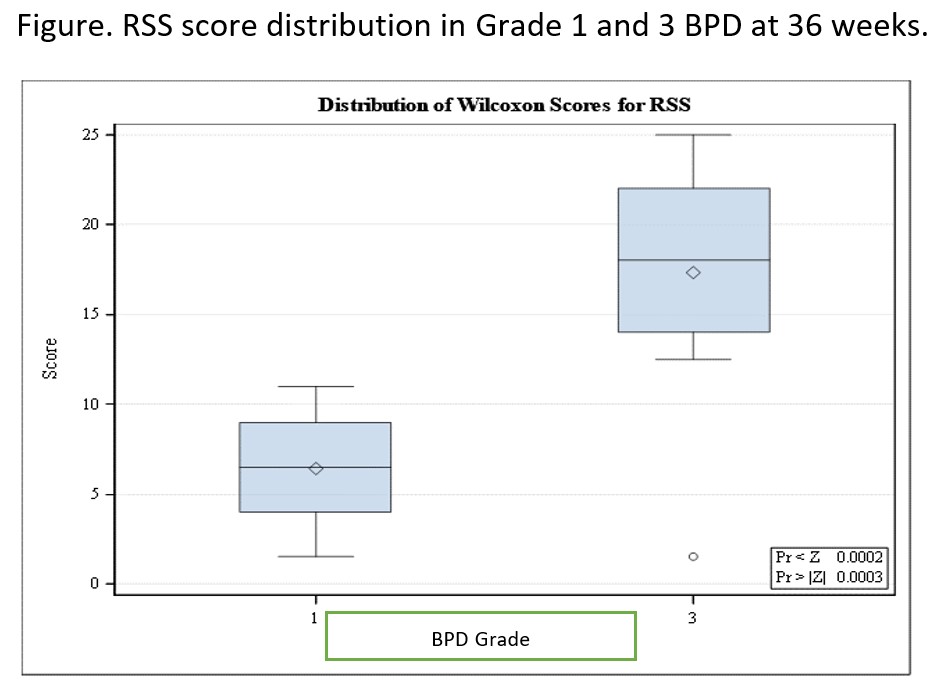
Results: We enrolled 81 preterm infants. Maternal and neonatal demographics shown in table. RSS was significantly higher in grade 3 BPD- 1.0 vs 0.23 in grade 1 BPD (p < 0.0001) (figure). For every unit increase in Wt/L Z score, RSS increased by 0.069 (p < 0.0001). RSS significantly correlated with W/L Z scores, percentiles, and BMI (P < /= 0.0001) after including postnatal steroids, gestational age, and sex in the regression model. When the infants with postnatal steroids were excluded, the results remained significant. The mean RSS @ 40 weeks in W/L < /= 50th percentile was 0.0.09 ± 0.27 compared to 0.47 ± 0.37 in >50 percentile category (p=0.01). Conclusion(s): RSS was higher in grade 3 BPD than in grade 1. Our study is the first to demonstrate that higher BMI and W/L may be associated with worsening respiratory severity in infants with BPD. This correlation remained significant even in those not exposed to postnatal steroids. Hence, the clinician should maintain an optimal W/L ratio to avoid additional respiratory burden in preterm infants with BPD.
Table. Maternal and neonatal demographics.jpg)
Figure. RSS score distribution in Grade 1 and 3 BPD at 36 weeks.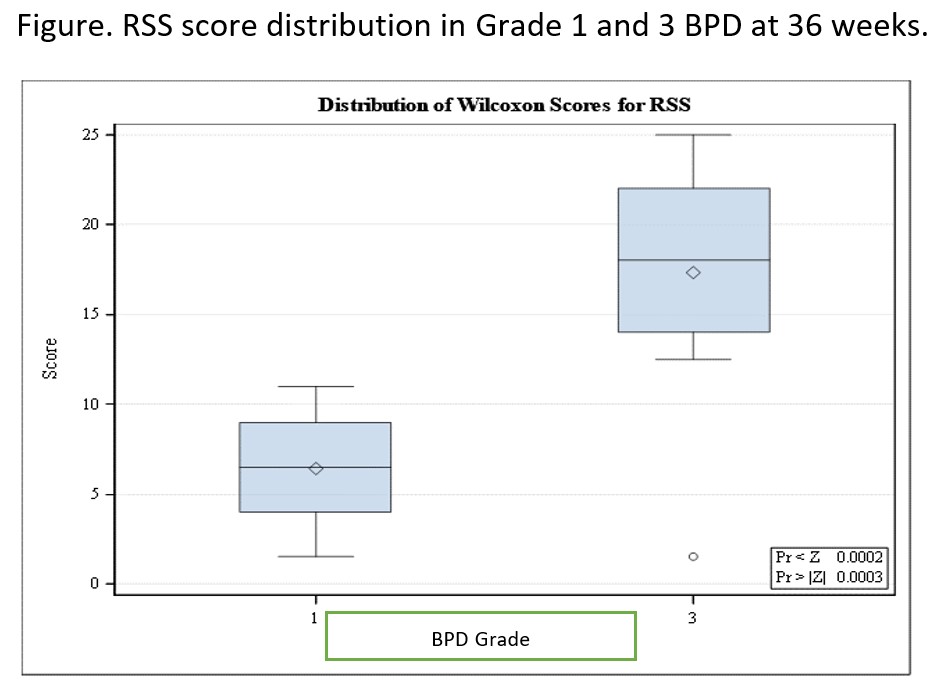
Objective: To explore with a prospective observational study if higher W/L z-scores at 33-36 weeks of gestation correlate with higher RSS at 36 & 40 weeks corrected gestational age in preterm infants with BPD.
Design/Methods: Supported by NIH (Award # 1U54GM115428). Preterm infants born @ < 30 weeks requiring respiratory support for >2 days @ 30-33 weeks were enrolled. Weight, length, and head circumference were measured weekly. Data on mean calories & protein, W/L z-scores & BMI were collected. RSS was calculated as per the STOP-ROP trial. BPD was defined as per the NICHD BPD workshop published in February 2018. Data were analyzed using descriptive and inferential statistics. Linear mixed model regression was used to study the relationship between the continuous variables with potential covariates.
Results: We enrolled 81 preterm infants. Maternal and neonatal demographics shown in table. RSS was significantly higher in grade 3 BPD- 1.0 vs 0.23 in grade 1 BPD (p < 0.0001) (figure). For every unit increase in Wt/L Z score, RSS increased by 0.069 (p < 0.0001). RSS significantly correlated with W/L Z scores, percentiles, and BMI (P < /= 0.0001) after including postnatal steroids, gestational age, and sex in the regression model. When the infants with postnatal steroids were excluded, the results remained significant. The mean RSS @ 40 weeks in W/L < /= 50th percentile was 0.0.09 ± 0.27 compared to 0.47 ± 0.37 in >50 percentile category (p=0.01). Conclusion(s): RSS was higher in grade 3 BPD than in grade 1. Our study is the first to demonstrate that higher BMI and W/L may be associated with worsening respiratory severity in infants with BPD. This correlation remained significant even in those not exposed to postnatal steroids. Hence, the clinician should maintain an optimal W/L ratio to avoid additional respiratory burden in preterm infants with BPD.
Table. Maternal and neonatal demographics
.jpg)
Figure. RSS score distribution in Grade 1 and 3 BPD at 36 weeks.