Neonatal Infectious Diseases/Immunology
Category: Abstract Submission
Neonatal Infectious Diseases/Immunology: Sepsis
566 - Host Maturity and Microbial Factors Regulate the Anti-Inflammatory Effects of Adjunctive Pentoxifylline in Murine Neonatal Sepsis
Monday, April 25, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 566
Publication Number: 566.427
Publication Number: 566.427
Esther M. Speer, Stony Brook Children's Hospital, Stony Brook, NY, United States; Atilade A. Adedeji, Stony Brook Children's Hospital, Centreach, NY, United States

Esther M. Speer, MD
Associate Professor of Pediatrics
Stony Brook Children's Hospital
Stony Brook, New York, United States
Presenting Author(s)
Background: Neonatal sepsis triggers inflammation that contributes to mortality and brain injury. The phosphodiesterase inhibitor pentoxifylline (PTX), which suppresses pro- and enhances anti-inflammatory cytokines, is a candidate adjunctive therapy for newborn sepsis. The effects of PTX on sepsis-induced cerebral inflammation in the newborn and its interaction with microbial and host factors remain however poorly understood.
Objective: To determine the role of postnatal age and microbial agents on the anti-inflammatory effects of PTX in an antibiotic-treated murine neonatal sepsis model.
Design/Methods: Newborn ( < 24 hours (h)) or infant (7 days old) C57BL/6J mice (n=209), corresponding immunologically to preterm and term human neonates, were injected intraperitoneally with live Escherichia coli K1 (105 colony forming units (CFU)/g weight) or Staphylococcus epidermidis (107 CFU/g). 1.5 h later, pups were randomly assigned to saline, antibiotic (gentamicin or vancomycin), antibiotic with PTX, or PTX alone, and were euthanized after an additional 4 h. CFUs, cytokines and chemokines were measured in homogenized tissue and compared with 1-way ANOVA and Kruskal-Wallis tests.
Results: Cerebral cytokine and chemokine concentrations were significantly lower in newborn vs infant mice with E. coli sepsis, and were lowest in S. epidermidis-infected pups. PTX did not suppress pro-inflammatory cytokines (IL-1, IL-2, IL-12, TNF, interferon-γ) except for IL-12p40 in E. coli septic newborn mice. Whereas adjunctive PTX augmented the anti-inflammatory and pro-resolution cytokines IL-10, IL-6 and G-CSF in E. coli septic infant mice, IL-6 and G-CSF were diminished and IL-10 unchanged in E. coli-infected newborn mice, without any changes in S. epidermidis septic infant mice. Addition of PTX to antibiotics decreased cerebral expression of keratinocyte-derived chemokine (CXCL1), chemokine ligand 2 (CCL2), CCL3 and CCL4 in E. coli septic newborn, however showed blunted chemokine suppression in E. coli septic infant mice, without any changes in S. epidermidis septic infant mice. Cerebral tissue CFUs remained low in saline- and antibiotic-treated mice, and addition of PTX did not augment bacterial growth.Conclusion(s): Postnatal age and microorganisms differentially modify the anti-inflammatory profile of adjunctive PTX in antibiotic-treated neonatal septic mice, with prominent chemokine suppression in newborn and enhanced anti-inflammatory cytokine expression in infant mice with E. coli sepsis, without changing S. epidermidis-induced cerebral inflammation. These findings may have implications for individualized therapy of newborn sepsis.
Figure 1: Adjunctive PTX differentially modifies anti-inflammatory and pro-resolution cytokines in newborn and infant mice with E. coli sepsis.jpg) a) Newborn mice ( < 24 hours old) b) Infant mice (7 days old).
a) Newborn mice ( < 24 hours old) b) Infant mice (7 days old).
SAL (saline), GENT (gentamicin), G+P (gentamycin and pentoxifylline), PTX (pentoxifylline).
Statistical significance: *p < 0.05, **p < 0.01,***p < 0.001.
Figure 2: Adjunctive PTX inhibits cerebral chemokine responses in murine neonatal E. coli sepsis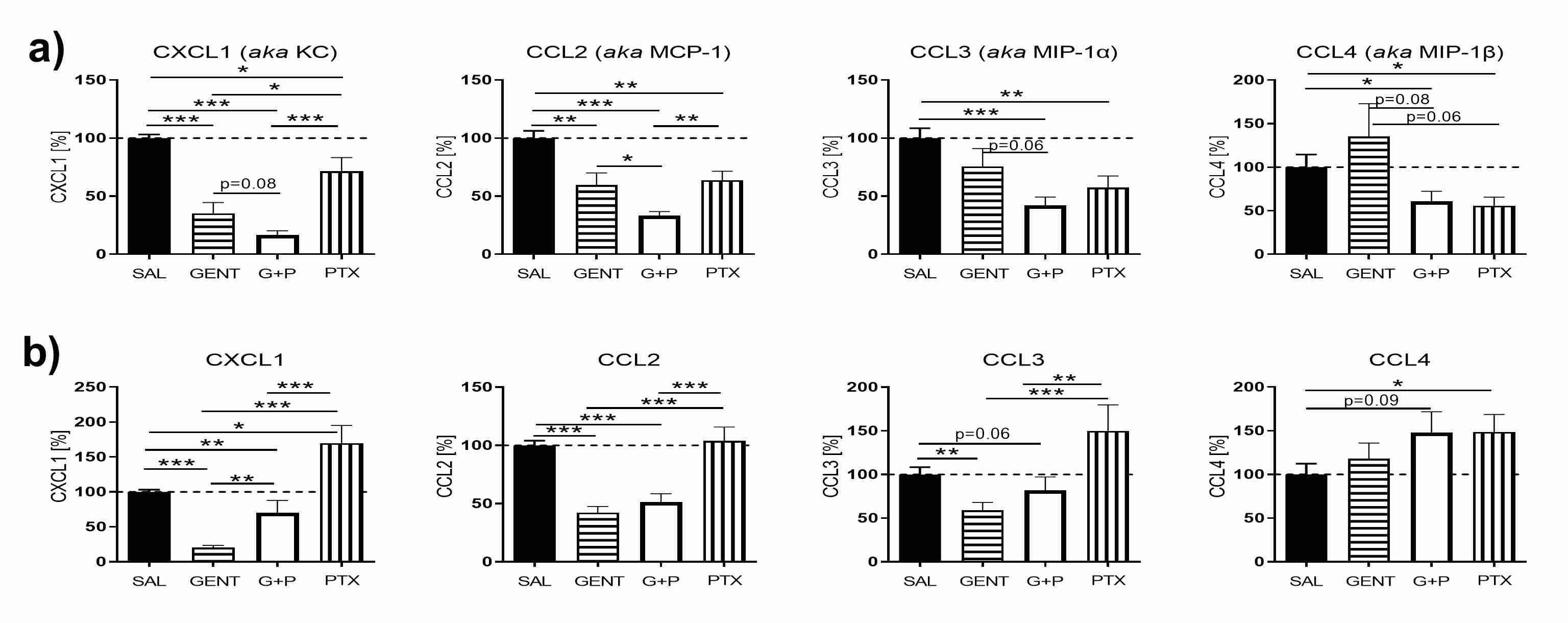 a) Newborn mice ( < 24 hours old) b) Infant mice (7 days old).
a) Newborn mice ( < 24 hours old) b) Infant mice (7 days old).
SAL (saline), GENT (gentamicin), G+P (gentamycin and pentoxifylline), PTX (pentoxifylline).
Statistical significance: *p < 0.05, **p < 0.01,***p < 0.001.
Objective: To determine the role of postnatal age and microbial agents on the anti-inflammatory effects of PTX in an antibiotic-treated murine neonatal sepsis model.
Design/Methods: Newborn ( < 24 hours (h)) or infant (7 days old) C57BL/6J mice (n=209), corresponding immunologically to preterm and term human neonates, were injected intraperitoneally with live Escherichia coli K1 (105 colony forming units (CFU)/g weight) or Staphylococcus epidermidis (107 CFU/g). 1.5 h later, pups were randomly assigned to saline, antibiotic (gentamicin or vancomycin), antibiotic with PTX, or PTX alone, and were euthanized after an additional 4 h. CFUs, cytokines and chemokines were measured in homogenized tissue and compared with 1-way ANOVA and Kruskal-Wallis tests.
Results: Cerebral cytokine and chemokine concentrations were significantly lower in newborn vs infant mice with E. coli sepsis, and were lowest in S. epidermidis-infected pups. PTX did not suppress pro-inflammatory cytokines (IL-1, IL-2, IL-12, TNF, interferon-γ) except for IL-12p40 in E. coli septic newborn mice. Whereas adjunctive PTX augmented the anti-inflammatory and pro-resolution cytokines IL-10, IL-6 and G-CSF in E. coli septic infant mice, IL-6 and G-CSF were diminished and IL-10 unchanged in E. coli-infected newborn mice, without any changes in S. epidermidis septic infant mice. Addition of PTX to antibiotics decreased cerebral expression of keratinocyte-derived chemokine (CXCL1), chemokine ligand 2 (CCL2), CCL3 and CCL4 in E. coli septic newborn, however showed blunted chemokine suppression in E. coli septic infant mice, without any changes in S. epidermidis septic infant mice. Cerebral tissue CFUs remained low in saline- and antibiotic-treated mice, and addition of PTX did not augment bacterial growth.Conclusion(s): Postnatal age and microorganisms differentially modify the anti-inflammatory profile of adjunctive PTX in antibiotic-treated neonatal septic mice, with prominent chemokine suppression in newborn and enhanced anti-inflammatory cytokine expression in infant mice with E. coli sepsis, without changing S. epidermidis-induced cerebral inflammation. These findings may have implications for individualized therapy of newborn sepsis.
Figure 1: Adjunctive PTX differentially modifies anti-inflammatory and pro-resolution cytokines in newborn and infant mice with E. coli sepsis
.jpg) a) Newborn mice ( < 24 hours old) b) Infant mice (7 days old).
a) Newborn mice ( < 24 hours old) b) Infant mice (7 days old).SAL (saline), GENT (gentamicin), G+P (gentamycin and pentoxifylline), PTX (pentoxifylline).
Statistical significance: *p < 0.05, **p < 0.01,***p < 0.001.
Figure 2: Adjunctive PTX inhibits cerebral chemokine responses in murine neonatal E. coli sepsis
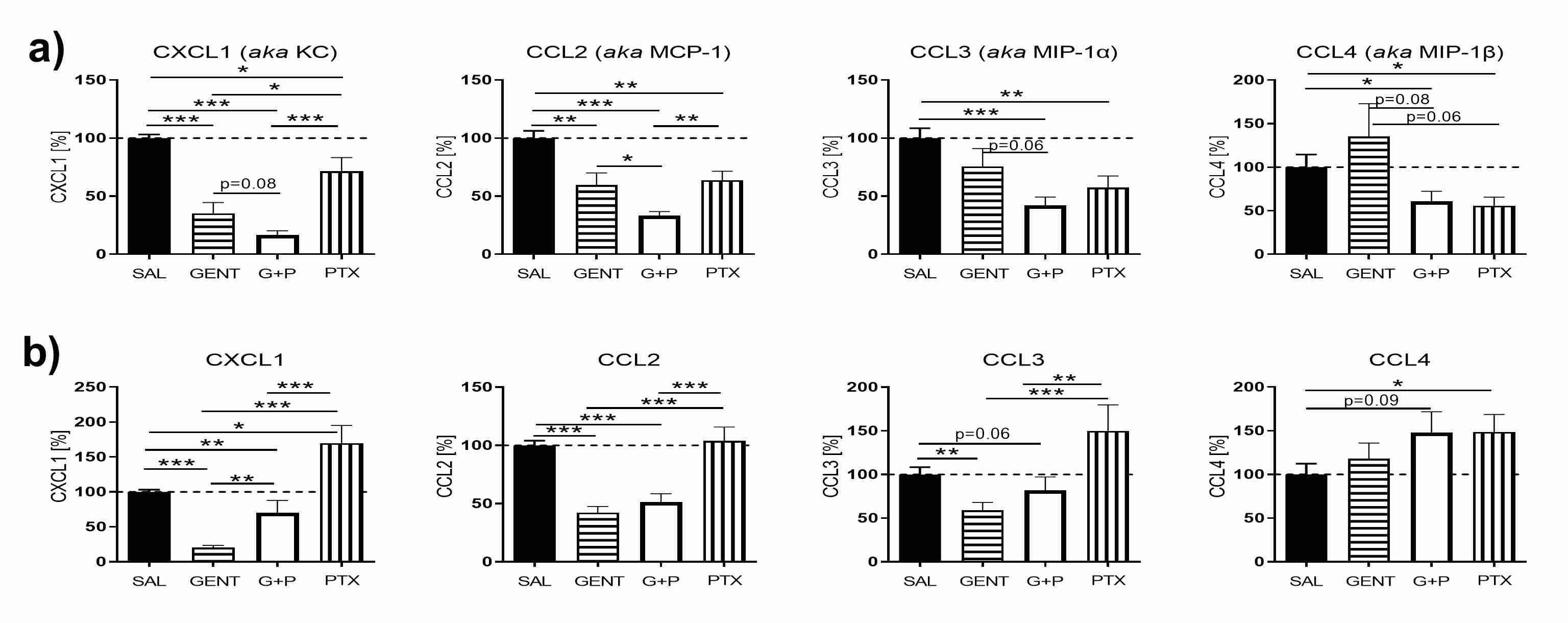 a) Newborn mice ( < 24 hours old) b) Infant mice (7 days old).
a) Newborn mice ( < 24 hours old) b) Infant mice (7 days old).SAL (saline), GENT (gentamicin), G+P (gentamycin and pentoxifylline), PTX (pentoxifylline).
Statistical significance: *p < 0.05, **p < 0.01,***p < 0.001.
