Health Services Research
Category: Abstract Submission
Health Services Research I
199 - Perinatal Outcomes for Rural Patients in Rural-Located and Metropolitan-Located Hospitals
Sunday, April 24, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 199
Publication Number: 199.319
Publication Number: 199.319
Sara C. Handley, Children's Hospital of Philadelphia, Philadelphia, PA, United States; Molly Passarella, Childrens Hospital of Philadelphia, Philadelphia, PA, United States; Julia D. Interrante, University of Minnesota School of Public Health, Minneapolis, MN, United States; Katy B. Kozhimannil, University of Minnesota, Minneapolis, MN, United States; Scott A. Lorch, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, United States

Sara C. Handley, MD, MSCE (she/her/hers)
Assistant Professor of Pediatrics
Children's Hospital of Philadelphia
Philadelphia, Pennsylvania, United States
Presenting Author(s)
Background: Rural residents receive perinatal care in hospitals located in rural places and metropolitan areas. Little is known about the distribution, characteristics, and outcomes of rural residents across different types of rural-serving hospitals.
Objective: To compare rural resident (birth parent and infant) characteristics and outcomes between 1) rural-located, 2) rural-serving, metropolitan-located, and 3) non-rural-serving, metropolitan-located hospitals.
Design/Methods: This was a retrospective observational cohort study of rural residents who gave birth in a hospital with ≥10 births/year from 2000-2012 in California, 2000-2014 in Pennsylvania, or 2000-2015 in South Carolina. Hospitals in rural counties were “rural-located.” Hospitals located in metropolitan counties with >90
th
percentile (10%) of perinatal patients from rural communities were deemed “rural-serving” and those with < 90
th
percentile were deemed “non-rural-serving”. Birth parent and infant characteristics were examined by hospital type. The primary outcome was any adverse maternal or neonatal outcome (maternal death, severe maternal morbidity, neonatal death, preventable fetal death, unexpected term complications, and preterm complications). Outcomes were compared as unadjusted rates and adjusted odds ratios, using logistic regression models to account for patient characteristics, year, and hospital as a random effect.
Results: Of 466,896 rural resident births, 64.3% occurred in rural-located hospitals, 22.5% in rural-serving metropolitan-located hospitals, and 13.1% in non-rural-serving, metropolitan located hospitals (Table 1). Patients who gave birth in rural-located hospitals were younger, more likely Medicaid-insured, had less education, and fewer complicating conditions. Unadjusted rates of the primary outcome increased between rural-located (7.5%), rural-serving metropolitan-located (9.1%), and non-rural serving metropolitan-located (17.8%) hospitals (Table 2). Compared to rural-located hospitals, adjusted odds of an adverse outcome increased in rural-serving (aOR 1.27, 95% CI 1.10, 1.46) and non-rural serving (aOR 1.35, 95% CI 1.18, 1.55) metropolitan-located hospitals.Conclusion(s): Rural residents receive care in rural-located and metropolitan-located hospitals, with the latter serving 35.6% of rural patients. Patients who give birth in metropolitan-located hospitals have a higher frequency of complicating conditions and increased odds of adverse outcomes. To ensure clinically appropriate and rural-relevant care, institutions should coordinate rural obstetric clinical and policy efforts.
Table 1. Birth Parent and Infant Characteristics by Hospital-Serving Status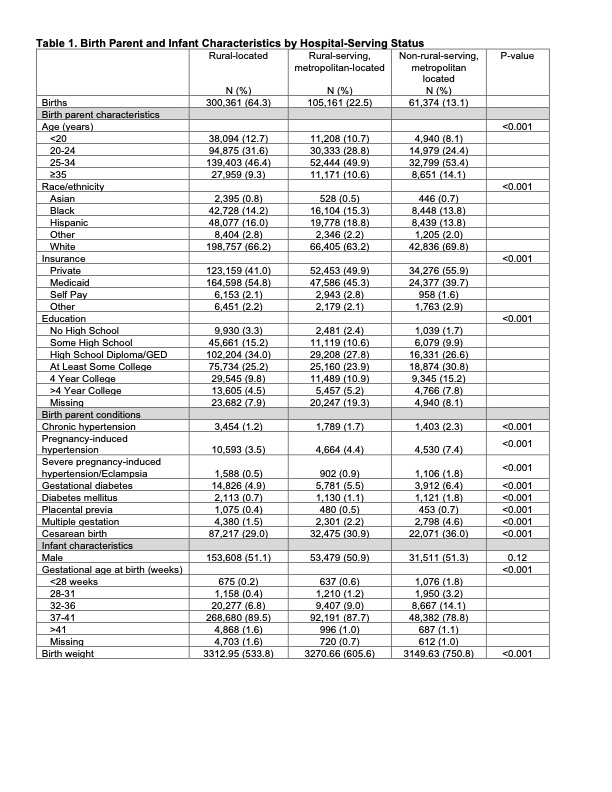
Table 2. Adverse Perinatal Outcomes by Hospital-Serving Status.jpg)
Objective: To compare rural resident (birth parent and infant) characteristics and outcomes between 1) rural-located, 2) rural-serving, metropolitan-located, and 3) non-rural-serving, metropolitan-located hospitals.
Design/Methods: This was a retrospective observational cohort study of rural residents who gave birth in a hospital with ≥10 births/year from 2000-2012 in California, 2000-2014 in Pennsylvania, or 2000-2015 in South Carolina. Hospitals in rural counties were “rural-located.” Hospitals located in metropolitan counties with >90
th
percentile (10%) of perinatal patients from rural communities were deemed “rural-serving” and those with < 90
th
percentile were deemed “non-rural-serving”. Birth parent and infant characteristics were examined by hospital type. The primary outcome was any adverse maternal or neonatal outcome (maternal death, severe maternal morbidity, neonatal death, preventable fetal death, unexpected term complications, and preterm complications). Outcomes were compared as unadjusted rates and adjusted odds ratios, using logistic regression models to account for patient characteristics, year, and hospital as a random effect.
Results: Of 466,896 rural resident births, 64.3% occurred in rural-located hospitals, 22.5% in rural-serving metropolitan-located hospitals, and 13.1% in non-rural-serving, metropolitan located hospitals (Table 1). Patients who gave birth in rural-located hospitals were younger, more likely Medicaid-insured, had less education, and fewer complicating conditions. Unadjusted rates of the primary outcome increased between rural-located (7.5%), rural-serving metropolitan-located (9.1%), and non-rural serving metropolitan-located (17.8%) hospitals (Table 2). Compared to rural-located hospitals, adjusted odds of an adverse outcome increased in rural-serving (aOR 1.27, 95% CI 1.10, 1.46) and non-rural serving (aOR 1.35, 95% CI 1.18, 1.55) metropolitan-located hospitals.Conclusion(s): Rural residents receive care in rural-located and metropolitan-located hospitals, with the latter serving 35.6% of rural patients. Patients who give birth in metropolitan-located hospitals have a higher frequency of complicating conditions and increased odds of adverse outcomes. To ensure clinically appropriate and rural-relevant care, institutions should coordinate rural obstetric clinical and policy efforts.
Table 1. Birth Parent and Infant Characteristics by Hospital-Serving Status
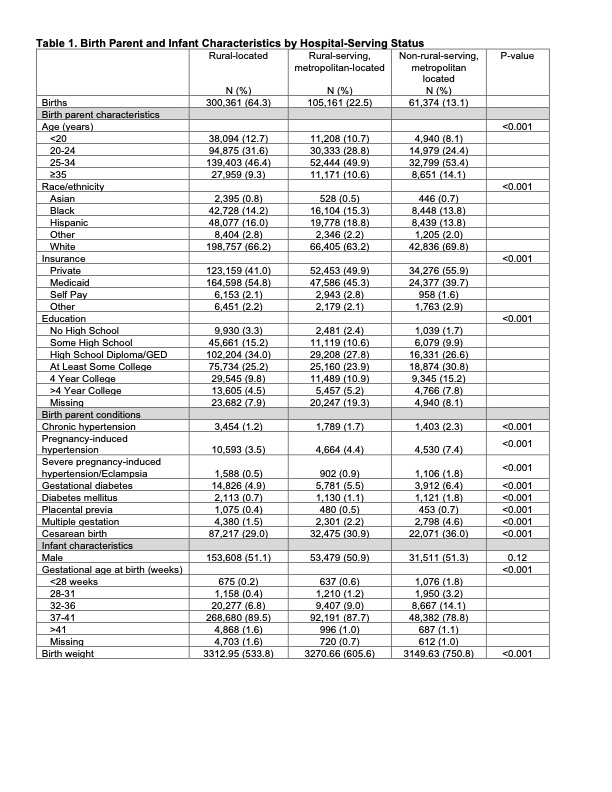
Table 2. Adverse Perinatal Outcomes by Hospital-Serving Status
.jpg)
