Neonatal Respiratory Assessment/Support/Ventilation
Category: Abstract Submission
Neonatal Respiratory III: BPD
459 - Differential oxygenation index trajectories for bronchopulmonary dysplasia of various grades in infants born less than 32 weeks’ gestation
Saturday, April 23, 2022
3:30 PM - 6:00 PM US MT
Poster Number: 459
Publication Number: 459.229
Publication Number: 459.229
Rebekah M. Leigh, Loma Linda University School of Medicine, Redlands, CA, United States; John B. C. Tan, Loma Linda University Children's Hospital, Riverside, CA, United States; Hung-Wen Yeh, Children's Mercy Hospital, Kansas City, MO, United States; Fu-Sheng Chou, Loma Linda University School of Medicine, Loma Linda, CA, United States

Srinandini S. Rao, BA, DO
Neonatology-Perinatology Fellow
Loma Linda University Children's Hospital
Pomona, California, United States
Presenting Author(s)
Background: Bronchopulmonary dysplasia (BPD) remains a significant challenge in neonatology. The likelihood of developing BPD has been shown to correlate with various distinct patterns of fraction of inspired oxygen (FiO2) trajectories in the first two weeks of life – low FiO2, pulmonary deterioration, and early persistent pulmonary deterioration. With a new grading system of BPD emerging (defined in Table 1 based on Jensen et al. 2019), it is prudent to investigate whether trajectories of respiratory support during early postnatal life can predict BPD grades.
Objective: Since oxygenation index (OI – a function of FiO2, mean airway pressure [MAP], and partial pressure of oxygen [PaO2]) recapitulate the degree of respiratory support more accurately than FiO2 by itself, we modeled OI trajectories in the first three weeks of life for each BPD grade using generalized additive mixed modeling (GAMM).
Design/Methods: We conducted a single-center retrospective study from 2018 to 2020. BPD grade was defined according to Jensen et al. 2019. To calculate OI, FiO2, MAP, and PaO2 data were extracted from electronic medical records. First, GAMM was used to model the OI trajectories for all available data to develop reference curves. This model included log-transformed OI as the outcome variable and a smooth function for the day of life when arterial blood gas tests were acquired; patient-specific intercepts and slopes were used to capture data dependency. Subsequently, a variable for the BPD grade was introduced as an interaction term for the smooth function of time to model OI trajectories for each BPD grade. The differences in OI trajectories between grades were then calculated.
Results: We identified 337 babies born at less than 32 weeks' gestation who either survived until 36 weeks CGA in our NICU for BPD grading or succumbed to morbidities of prematurity after 4 weeks of age. This sample provided 7,702 respiratory/blood gas data points for OI calculation. Demographic characteristics are summarized in Table 1. Raw OI and the trajectory of modeled expected values for each BPD grade is shown in Figure 1. The differences in the expected OI trajectories between BPD grades are shown in Figure 2. Overall, Grade 1-3 groups showed a higher OI from the 1st week of life compared to the no-BPD group (Grade 0), and the distinctions in OI trajectories among Grade 1-3 became apparent in the 3rd week of life. Conclusion(s): OI trajectories differ among different BPD grades during early postnatal life. OI trajectories may be used in BPD grade prediction to guide therapeutic interventions.
CV 2021.pdf
Log-transformed oxygenation index (OI) trajectories for each BPD grade modeled using generalized additive mixed modeling.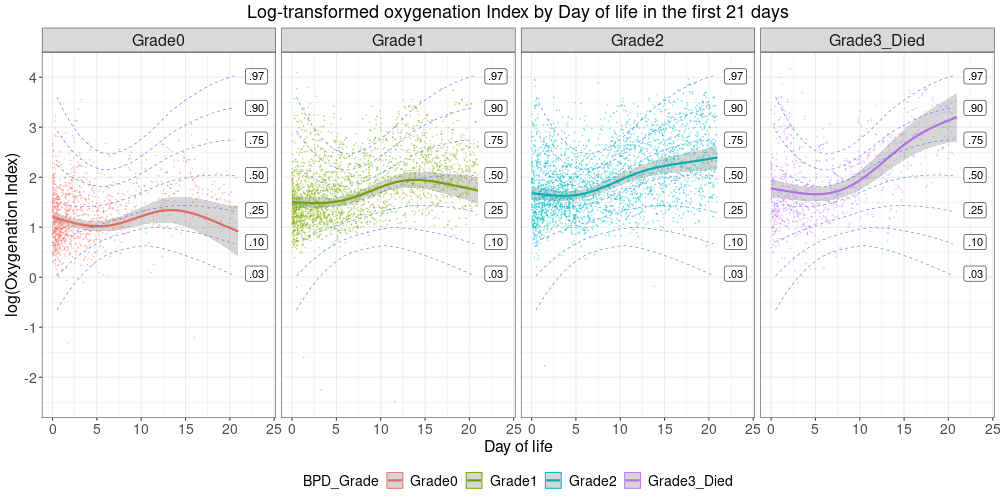 Reference curves were generated using all available log-transformed OI for trajectory modeling and are shown by blue dashed lines. “.50” denotes expected values (50% percentile). Percentile lines were calculated based on standard deviation by multiplying the standard error of the expected values by the number of OI data for each day of life.
Reference curves were generated using all available log-transformed OI for trajectory modeling and are shown by blue dashed lines. “.50” denotes expected values (50% percentile). Percentile lines were calculated based on standard deviation by multiplying the standard error of the expected values by the number of OI data for each day of life.
Objective: Since oxygenation index (OI – a function of FiO2, mean airway pressure [MAP], and partial pressure of oxygen [PaO2]) recapitulate the degree of respiratory support more accurately than FiO2 by itself, we modeled OI trajectories in the first three weeks of life for each BPD grade using generalized additive mixed modeling (GAMM).
Design/Methods: We conducted a single-center retrospective study from 2018 to 2020. BPD grade was defined according to Jensen et al. 2019. To calculate OI, FiO2, MAP, and PaO2 data were extracted from electronic medical records. First, GAMM was used to model the OI trajectories for all available data to develop reference curves. This model included log-transformed OI as the outcome variable and a smooth function for the day of life when arterial blood gas tests were acquired; patient-specific intercepts and slopes were used to capture data dependency. Subsequently, a variable for the BPD grade was introduced as an interaction term for the smooth function of time to model OI trajectories for each BPD grade. The differences in OI trajectories between grades were then calculated.
Results: We identified 337 babies born at less than 32 weeks' gestation who either survived until 36 weeks CGA in our NICU for BPD grading or succumbed to morbidities of prematurity after 4 weeks of age. This sample provided 7,702 respiratory/blood gas data points for OI calculation. Demographic characteristics are summarized in Table 1. Raw OI and the trajectory of modeled expected values for each BPD grade is shown in Figure 1. The differences in the expected OI trajectories between BPD grades are shown in Figure 2. Overall, Grade 1-3 groups showed a higher OI from the 1st week of life compared to the no-BPD group (Grade 0), and the distinctions in OI trajectories among Grade 1-3 became apparent in the 3rd week of life. Conclusion(s): OI trajectories differ among different BPD grades during early postnatal life. OI trajectories may be used in BPD grade prediction to guide therapeutic interventions.
CV 2021.pdf
Log-transformed oxygenation index (OI) trajectories for each BPD grade modeled using generalized additive mixed modeling.
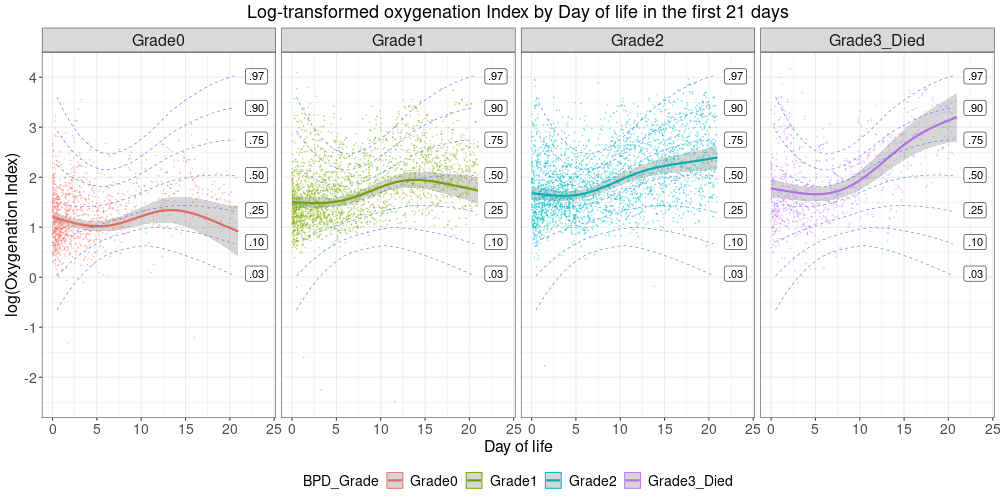 Reference curves were generated using all available log-transformed OI for trajectory modeling and are shown by blue dashed lines. “.50” denotes expected values (50% percentile). Percentile lines were calculated based on standard deviation by multiplying the standard error of the expected values by the number of OI data for each day of life.
Reference curves were generated using all available log-transformed OI for trajectory modeling and are shown by blue dashed lines. “.50” denotes expected values (50% percentile). Percentile lines were calculated based on standard deviation by multiplying the standard error of the expected values by the number of OI data for each day of life.